Mycobacterium Tuberculosis Flashcards
(38 cards)
Mycobacterium General Charcateristics
- Gram + wall structure
- mycolic acids
- Lipoarabinomannan (LAM), a lipid polysaccharide complex extends from the plasma membrane to the surface.
- acid fast
Mycobacterium - LAM
•LAM is structurally and functionally analogous to the lipopolysaccharide of gramnegative bacteria. These elements give the mycobacteria a cell wall with unusually high lipid content, which accounts for many of their biologic characteristics. It can be thought of as a waxy coat that makes them hardy, impenetrable, and hydrophobic

Mycobacterium Growth
- The most important pathogen, M tuberculosis (MTB), is an obligate aerobe.
- Other nutritional requirements vary among species and range from the ability of some nonpathogens to multiply on the washers of water faucets to the strict intracellular parasitism of M leprae.
- Mycobacteria grow more slowly than most human pathogenic bacteria in part due to their hydrophobic cell surface, which causes them to clump and limits permeability of nutrients into the cell.
Mycobacterium Disease
- Diseases caused by mycobacteria usually develop slowly, follow a chronic course, and elicit a granulomatous response.
- Infectivity of pathogenic species is high, but virulence (disease production) for healthy humans is moderate. Disease following infection with MTB is the exception rather than the rule.
Mycobacteria do not / do produce classic exotoxins or endotoxins.
Mycobacteria do not / do produce classic exotoxins or endotoxins.
Two Host Responses that Cause Disease Process
- a delayed-type hypersensitivity (DTH) reaction to mycobacterial proteins, results in the destruction of nonactivated macrophages containing multiplying organisms. It is detected by intradermal injections of purified proteins from the mycobacteria.
- cellmediated immunity (CMI) activates macrophages enabling them to destroy mycobacteria contained within their cytoplasm.
The balance between these two responses determines the pathology and clinical response to a mycobacterial infection.
M. tuberculosis Organism
- MTB is a slim, strongly acid–alcohol–fast rod. It frequently shows irregular beading in its staining, appearing as connected series of acid-fast granules.
- It grows at 37oC, but not at room temperature, and it requires enriched or complex media for primary growth.
- The classic medium (Löwenstein–Jensen) contains homogenized egg in nutrient base with dyes to inhibit the growth of nonmycobacterial contaminants.
- Growth is slow
M. tuberculosis Cell Wall
- Because of its hydrophobic lipid surface, MTB is unusually resistant to drying, to most common disinfectants, and to acids and alkalis. Tubercle bacilli are sensitive to heat, including pasteurization, and individual organisms in droplet nuclei are susceptible to inactivation by ultraviolet light. As with other mycobacteria, the MTB cell wall structure is dominated by mycolic acids and LAM. Its antigenic makeup includes many protein and polysaccharide antigens, of which tuberculin is the most studied.
- Tuberculin consists of heat-stable proteins released into liquid culture media.
- A purified protein derivative (PPD) of tuberculin is used for skin testing for hypersensitivity.
M. tuberculosis Epidemiology
M. tuberculosis Pathogenesis

M. tuberculosis Primary TB
- MTB is a facultative intracellular pathogen whose success depends on avoiding the killing mechanisms of professional phagocytes.
- Primary tuberculosis is the initial infection in which inhaled droplet nuclei containing tubercle bacilli are deposited in the peripheral respiratory alveoli, most frequently those of the well-ventilated middle and lower lobes. At the earliest stages an attachment protein (ESAT-6) may facilitate binding to laminin in the basement membrane of alveolar epithelial cells. In the alveoli the bacteria are recognized by alveolar macrophage complement receptors (CR1, CR3, CR4) and phagocytosed.
- This inaugurates a two-stage battle within the macrophage, which may be resolved in weeks or last for decades.

M. tuberculosis Primary TB Stage 1
•The first stage is with the phagosome/lysosome digestive mechanisms of the macrophage. In this process, MTB has the upper hand through its ability to interfere with the acidification of the phagosome, which renders the lysosomal enzymes (which require acidic pH) less effective. This allows the bacteria to multiply freely in the phagosome of the nonactivated macrophage.
M. tuberculosis Primary TB Stage 2
- The second stage is the triggering of TH1 immune responses, beginning with digestion and surface presentation of mycobacterial components and ending with cytokine activation of the macrophages.
- The short- and long-term outcomes of the infection depend on the ability of the macrophage activation process to overcome the intracellular edge that MTB has as a result of its ability to block acidification of the phagosome.
Early Stages of M. tuberculosis Infection
•In the early stages of infection, MTB-laden macrophages are transported through lymphatic channels to the hilar lymph nodes draining the infected site. From there, a low-level bacteremia disseminates the bacteria to a number of tissues, including the liver, spleen, kidney, bone, brain, meninges, and apices or other parts of the lung. Although the primary site of infection and enlarged hilar lymph nodes can often be detected radiologically (Ghon complex), the distant sites usually have no findings. In fact, the primary evidence for their existence is reactivation at nonpulmonary sites later in life. Tuberculous meningitis is the most serious of these infections.
Later Stages of M. tuberculosis Infection
- In the primary lesion as MTB cells multiply, macrophages and dendritic cells release cytokines (tumor necrosis factor, interleukin 12, interferon gamma [IFN-γ]), which attract T cells and other inflammatory cells to the site.
- The recruited CD4 T cells initiate the TH1-type immune response over the following 3 to 9 weeks in which IFN-γ is the primary activator of macrophages.
- This process is highly specific involving only the T cells and the above mentioned cytokine mediators. As the bacteria multiply, they release mycobacterial proteins which elicit a cellular hypersensitivity (DTH) response with its inflammatory fluids, phagocytes, and release of digestive enzymes.
- This adds a diffuse destructive component to the process, which is much less specific than the macrophage activation process. The tissue destruction caused by this chronic inflammatory process is the sole known source of injury in tuberculosis.
M. tuberculosis and DTH
- The magnitude of the DTH depends on the size of the MTB population.
- If the TH1 immune process is effective, MTB, the source of antigenic stimulation is controlled and with it the chronic DTH inflammation. As this is the only source of injury, the disease resolves and the patient recovers.
- The mycobacterial protein-specific DTH sensitization remains, and its elicitation is the basis of the tuberculin skin test.
M. tuberculosis and Granulomas
- The mixture of the TH1 immune and DTH responses is manifest in a microscopic structure called a granuloma, which is composed of lymphocytes, macrophages, epithelioid cells (activated macrophages), fibroblasts, and multinucleated giant cells all in an organized pattern.
- As the granuloma grows, the destructive nature of the hypersensitivity component leads to necrosis usually in the center of the lesion. This is termed caseous necrosis because of the cheesy, semisolid character of material at the center of large gross lesions, but the term fits the smooth glassy appearance of microscopic granulomas as well.
M. tuberculosis and Latency
- In tuberculosis, some of the organisms when faced with oxygen and nutrient deprivation instead of dying enter a prolonged dormant state called latency.
- Specific factors facilitating survival are not known but the waxy nature of the MTB cell wall must be of aid as it is in the environment.
- These organisms lie in the lung and elsewhere waiting for reactivation months, years, or decades later. For the vast majority (>90%) of persons who undergo a primary infection this never happens
M. tuberculosis and Reactivation
- The new foci are usually located in body areas of relatively high oxygen tension that would favor growth of the aerobe MTB.
- The apex of the lung is the most common, with spreading, coalescing granulomas, and large areas of caseous necrosis.
- Necrosis often involves the wall of a small bronchus from which the necrotic material is discharged, resulting in a pulmonary cavity and bronchial spread.
- Frequently, small blood vessels are also eroded.
- The destructive nature of these lesions cannot be directly attributed to any products or structural components of MTB. The damage is due to the failure of the host to control growth of MTB and thus the rising load of mycobacterial proteins which stimulate the autodestructive DTH inflammatory response.

M. tuberculosis and Tuberculosis
- Humans generally have a high innate immunity to development of disease. Only 10% of immunocompetent persons infected with MTB develop any form of active disease in their lifetime.
- Adaptive immunity to tuberculosis is primarily related to the development of reactions mediated through CD4 T lymphocytes via TH1 pathways. Intracellular killing of MTB by macrophages activated by IFN-γ and other cytokines is the essential step.
- Cytotoxic CD8 T cells are also generated during infection and may play some role.
- Although antibodies are formed in the course of disease, there is no evidence they play any role in immunity.
M. tuberculosis Symptoms
•Primary
- asymptomatic or fever and malaise
- Ghon complex, inflitrates in mid zone of lung
•Reactivation
- cough (first dry then with sputum, maybe some blood)
- fever, malaise, fatigue, weight loss, sweating
- inflitrates in apices of lungs —> cavities
- can first appear in other organs, such as the kidneys, bones, lymph nodes, brain, meninges, bone marrow, and bowel.
- Disease at nonpulmonary sites ranges from a localized tumor-like granulomas (tuberculomas) to a fatal chronic meningitis.
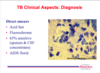
M. tuberculosis Diagnosis
• Intradermal MTB proteins (PPD)
– Induration >15 mm - 48-72 hrs.
• Demonstrates DTH
– Resolved infection (including treated)
– Latent infection
– Active disease
– BCG immunization (<15mm)
– Infection with other mycobacterial species (<15mm)

M. tuberculosis Direct Smears
M. tuberculosis Culture




