Pediatric Trauma Flashcards
when do you take C-spine precauctions in peds?
GCS<13
Dangerous MOI
neck pain
Altered mental status
intoxication
when do pediatric vitals look like adult vitals?
in children > 12 years old
how much blood loss can a child sustain and still be in compensated shock?
45%
what is the verbal GCS scoring for nonverbal pediatric patients?
coos, babbles 5
irritable cry 4
cries to pain 3
moans to pain 2
no response 1
what problem is common in pediatric trauma patients that warrants intervention with a gastric tube?
gastroparesis
what labs do you want to order for a peds trauma patient?
CBC, CMP, UA, Utox, blood glucose
what’s the first part of the secondary survey in peds trauma?
A - allergies
M - medications
P - PMH, pregnancy
L - last meal
E- events/environment leading to injury
AMPLE
If asystole persists after what is the prognosis poor in a pediatric resuscitation patient?
after two rounds of IV epinephrine OR
25 minutes of CPR without ROSC
how is drowning defined and how is near drowning defined?
drowning is death within 24 hours of submersion or immersion in a liquid medium
near drowning is survival > 24 hours from the event
what is the most common cause of death in children 1-4
drowning
what is the most common cause of death in children older than 4?
MVCs
why is hypothermia more of a problem in children?
high suface area: mass
decreased subcutaneous fat
limited thermogenic capacity
moderate hypothermia (32-35) leads to what key metabolic change?
increase in 02 consumption
severe hypothermia (<32) leads to what metabolic changes?
decreases cellular metabolic rate —> inadequate perfusion, hypotension, shock
7% decrease for every 1 degree C
*hypo/hyperglycemia, platelet dysfunction, depressed immune function
Are c-spine precautions routinely recommended in pediatric drowning or near drowning?
No - only if separate indiction
what else can you do in drowning other than O2?
CPAP or BiPAP
intubate if neurologic deterioration or PaO2<60mmHg or Sp02<90% w/o2
or PaCO2>50mmHg
You have just discovered your near-drowning peds patient has a glucose of 15. What do you do?
D5
(some places D10)
If hypothermia occurred first before asphyxia, pediatric patients generally have a better or worse prognosis?
better than if the asphyxia preceded the hypothermia
After you have dried a near-drowning patient and removed their wet clothing, what else can you do to warm them?
external rewarming: blankets, heating pads, radiant heat, forced warm air
internal core rewarming with IV fluids (40-43)
humidified oxygen 42-46 degress via tracheal tube
continue until core reaches 32-35 degrees
what is afterdrop?
the initial drop in temperature you see during initial warming in hypothermia
how long does it take for hypoxemia to result in irreversible CNS injury in peds?
3-5 minutes
you have a young girl that was resuscitated by EMS after she fell in her family swimming pool and was submerged after losing consciousness for 2 minutes. what do you do with her?
admit her and observe her
if she is asymptomatic for 8 hours, she can go home
(75% develop symptoms in first 8 hours)
what is the most common foreign body ingestion in children?
coins
when should you suspect toxic exposure/ingestion in a peds patient?
acute onset of multi-organ system dysfunction
AMS
respiratory compromis
metabolic acidosis
seizure without known disorder
if there are signs of a toxic exposure, what must you rule out in a child <1?
child abuse
what’s the preferred treatment for pediatric patients with hypertension resulting from ingestion?
benzodiazepenes
nitroprussides
Poison Antidote Chart for Peds

what percentage of pediatric bite wounds are by humans?
2-3%
dogs (60-90%) most common
cats (5-20%)
what are the predominant organisms in bite wounds?
gram -ve anerobes
animals - pasturella
humans - eikenella corrodens
primary closure on pediatric bite wounds should be done only if:
cosmetically important area (e.g., face)
clinically uninfected
<12 hour old bite (<24 hours on the face)
what’s the antibiotic treatment for an animal bite?
Augmentin 20 mg/kg dose BID for 3-5 days
what is the abx for human bites?
augmentin
or ampicillin-sulbactam (Unasyn)
50 mg/kg per dose QID for 3-5 days
What is the rx if the human biter is HbsAg+
initiate HB series vaccine in all unvaccinated
HebB vaccine
HepB immune globulin
in a pediatric patient a 2kg weight loss equals how many liters of fluid?
2L
what do you expect to find on labs in a peds patient with dehydration?
increased blood BUN
serum bicarb <17 mEq/L
High serum sodium and potassium
urine sodium, osmolatlity >450 and high specific gravity >1.015
if oral fluid therapy is possible for peds dehydration what are the goals?
5 mL/2 min
goal - 10ml/kg of body weight for each V/D episode
what is the IV fluid of choice in pediatrics?
IV crystalloid isotonic 0.9% saline
NEVER hypo or hyper crystalloids - no benefits to dextrose unless DM or burns
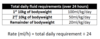
What’s the rate of fluid for pediatric dehydration?
emergent IV - rapid (bolus) infusion of 20mL/kg of isotonic sale in 10-30 minutes
what’s the epi of SIDS?
2-3x higher in AA and American Indian/Alaskan native babies
peaks at 2-4 months, 90% of cases before 6 months
mother: less than 20, smoker, drugs, delayed prenatal care, UTI/STIs
where should you never use lidocaine with epi?
fingers, nose, penis, toes
what are the main sedatives and analgesics used in peds ER procedures?



