Parasites 2: Geohelmints (Ascaris, hookworm, whipworm, strongyloidis) Flashcards
How are nematodes (round worms) classified?
Soil-transmitted (geohelminths):
- These usually depend on a period of development outside the human host
- Associated with poverty, inadequate hygiene and sanitation
- Often asymptomatic
- Most individuals only have a few worms but in those with many worms and chronic infection -> anaemia, retarded growth and neurological sequelae
- Anti-helminthic treatment can easily solve this
- Helminths are realtively similar, however can be divided by:
- Direct mode of transmission
- Can go straight from anus to mouth without development period in soil
- Modified direct mode of transmission
- Period of development in soil
- Penetration of the skin
- Develop in soil, get ready for infiltration of the skin to go back through oesophagus into intestine
- Direct mode of transmission

What is the life cycle of ascaris lumbricoides?
- Adult worms live in the lumen of the SMALL intestine
- The female is 20 – 25cm long, male about 30cm long
- The female produces 200k eggs per day which are passed in the stool
- Once deposited and the conditions are right (moist, warm and shaded soil), the fertile eggs become embryonated and infective, they then develop within a few days or a few weeks
- Once they are swallowed, the larvae hatch and infect the mucosa and are carried via the portal and then systemic circulation to the lungs
- There the arvae mature for 10 to 14 days
- There they break the alveolar walls, ascend the bronchiolar tree, reach the throat and are swallowed
- Once they reach the small intestine, they develop into adult worms
- It takes about 2-3 months form ingestion of the egg to mature adult – they can live for one to two years
- Intensity of disease is related to the worm burden and light infection are often asymptomatic with serious disease starting with >100 worms

What are the clinical features of ascaris?
- GI phase:
- Sometimes lactose intolerance and micronutrient deficiency
- Worms may ball up and cause obstruction -> most severe complication
- Most common in childen below ten years, likely due to narrow lumen and high worm-burden

How do we diagnose ascaris?

What does ascaris look like under the microscope?

How do we treat ascaris infection?

Which organisms cause hookworm infections?
- Two species that we focus on:
- Ancylostoma duodenale
- This one has large teeth
- Neactor americanus
- This one has dorsal and ventral cutting plates
- Ancylostoma duodenale
- Causes hookworm anaemia and disease
- Affects >700 million people globally
- Impairs physical and intellectual development of children and communities
- Found in all tropical and sub-tropical countries

What is the lifecycle of hookworm infections?
- Simple lifecycle:
- Eggs are passed in the stool and then the eggs hatch in or two days depending on whether the conditions are right (moist shaded soil)
- After 4 or 5 days they become filariform larvae
- This is the infectious stage of the hookworm
- They can survive 3 or 4 weeks of this stage
- On contact with the host, the larvae penetrate the skin and then travel through the blood to the heart and then to the lungs
- They break through the alveoli, ascend the bronchial tree to the throat and are swallowed
- In the intestine they attach to the wall causing blood loss
- Longevity: up to several years

What are the clinical features of hookworm infection?
Most infections are asymptomatic
But gradually worsening anaemia
Initially:
- itch at site of entry with possible pustules and vesiculation
Pneumonitis:
- Dry cough, asthmatic wheezing
- Fever and eosinophilia
- Not common in endemic areas
GI:
- Early:
- Epigastric discomfort
- Late:
- IDA + hypoproteinaemia
*
- IDA + hypoproteinaemia

How do we diagnose a hookworm infection?
Stool exmaination for ova and parasites

How do we treat hookworm infection?

Which organism causes whipworm infection and what is its life cycle?
Trichuris trichiura
- Found in areas with constant sunshine and rainfall
- Few symptoms normally
- But heavy infections can cause GI problems, rectal prolapse, anaemia, growth stunting and cognitive impairment
- Approx. 500 million people infected with whipworm globally in 2010
- Life cycle simple:
- Infective eggs are ingested via contaminated soils or hands
- The eggs are hatched and produce larvae that mature in the colon
- The adult worms of 4cm length live in the caecum and ascending colon
- The worms are fixed in that location but the anterior part go straight into the mucosa
- The females begin laying eggs 60 – 70 days after infection
- Females in the caecum shed up to 20k eggs per day
- The life span is about 1 year
- The unembryonated eggs pass with the stool
- In the soil the eggs develop into a two cell stage, then advanced cleavage and become embryonated
- Become infective in 15 to 30 days

Microscopy of trichuris?

What are the clinical features of trichuris infection?
- Light infection:
- Worms confined to caecum and ascending colon, causing little damage
- Heavy infection
- Worms spred through colon to rectum
- Cause haemorrhages, mucopurulent stools, dysentery, rectal prolapse
- Trichuris dysentery syndrome:
- severe dysentery
- prolapse of rectum
- It’s due to immune response
- Massive infantile trichuriasis
- Children between 3 and 10
- Hypoproteinaemia, severe anaemia, clubbin of fingers
- Growth retardation
- Effect on cognition and later achievements
How do we diagnose trichuris?

How do we treat trichuria?
Mebendazole > Albendazole
Strogyloidiasis facts
Strongyloides stercoralis = threadworm

What is the life cycle of strogyloidiasis?
- Two options
- Free living adult worms that prefer sandy warm moist soil environement
- Straight to infective larvae
- Free living worms:
- Mate and eggs are deposited in soil
- Eggs hatch
- Then develop into adult worms once again
- However, when condition for living become unfavourable, the eggs develop into infective larvae
- Infective larvae can penetrate skin and then usually migrate to lung via blood stream from where they are coughed up and swallowed into GI tract
- Larvae can also migrate directly to GI tract via connective tissues
- Small intestine: larvae multiply and become female adult worms
- There are no adult male worms in the parasitic cycle
- The females live in the wall of the small intestine and produce eggs by parthenogenesis
- The eggs yield rhaptidiform larvae which can be passed in the stool
- In auto-infection the rhaptidiform larvae become infective filariform larvae which can either penetrate the intestinal mucosa or the skin of the perianal area
- In either case, filariform larvae can disseminate through the body
- That is how people develop chronic infections or hyper-infection in immunosuppressed individuals

What are the clinical features of strongyloides infection?

How do we diagnose strogyloides?
- Repeated stool microscopy for rhabditiform larvae
- Hyperinfection: easily diagnosed by exmaining stool, sputum, CSF, etc.
- Duodenal biopsy and miscroscopy of duodenal aspirate
- Detection of filariform larvae
- Flexible gastroduodenoscopy
- String test more practical in resource limited settings
- Serology - for IgG
- Blood count - Elevated WCC and eosinophilia possible
- Generally difficult to diagnose
Microscopy difference strongyloides / ascaris

Microscopy strongyloides filariform larvae

Microscopy duodenal biopsy strongyloides

Treatment strongyloides
MCQ tips
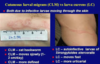
Recognise Larva Currens and do not confuse with cutaenous larva migrans
- Understand that pulmonary eosinophilia can be caused by Loffler’s Syndrome (the passage of helminth larvae through the lungs), Tropical Pulmonary Eosinophilia (immune response to lymphatic filariae) amongst other infective (mostly helminth) and medical causes. If this is the scenario think “Helminth”.
- Spend some time understanding Strongyloides – it is the most complex and interesting of these Nematodes and it’s a good source of questions.
Further microscopy of eggs

Which soil transmitted helminths pass through the lung?

What drug can lead to strongyloides hyperinfection?
A change in immune status can increase parasite numbers, leading to hyperinfection syndrome, dissemination, and death if unrecognized. Corticosteroid use is most commonly associated with hyperinfection syndrome


