Only diseases Flashcards
what is the most common hyperkinetic basal ganglia dysfunction?
what is the most common hypokinetic basal ganglia dysfunction?
Huntington’s Disease
Parkinson’s Disease
what is chorea?
what is athetosis?
what is dystonia?
what is ballismus?
rapid jerky involuntary movement
continued involuntary movement
locking muscles in a position
involuntary flinging of limbs
What is the cause of developing Huntington’s Disease?
why do we see the symptoms in this disease?
how do we categorize the symptoms seen in Huntington’s Disease?
loss of the ENK neurons of the striatum/neostriatum
Because the loss of ENK neurons allows the Globus Pallidus lateral to keep throwing GABA to the subthalamic nucleus…the globus pallidus medial does not get stimulated, the thalamus keeps active the cortex
Hyperkinetic
When does Sydenham’s Chorea happen?
what ages are susceptible to this disease?
what are the symptom’s seen?
after following a viral infection, in particular Rheumatic Fever
ages 5-15
milkmaids grasp (rhythmic squeezing when the patient attempts to grab something), choreic hand, darting tongue and PRONATOR SIGN
At what age does Parkinson’s Disease start?
What causes the symptoms to be seen in Parkinson’s Disease?
What can be seen in microscopy to identify Parkinson’s?
how do we categorize parkinson’s disease symptoms?
what are parkinson’s disease symptoms?
40-70
loss of neuromelanin due to loss of substantia negra
Lewy bodies
hypokinetic
resting tremor, bradykinesia
what is Wilson’s Disease?
What are the symptoms of Wilson’s Disease?
In what part of the brian will the accumulation occur in wilson’s disease?
Copper accumulation in Liver, eyes, brain, kidneys due to a enzyme deficiency
fatigue, hepatitis, cirrhosis, behavioral changes, hypo or hyperkinetic movements, infertility, arrhytmias, Kayser-Fleischer rings
Copper accumulates in the lentiform nuclei
what are the 3 types of cerebral palsy?
what gets damaged in each?
- spastic = corticospinal (motor cortex)
- ataxic = cerebellum
- athetoid or dyskinetic = basal ganglia damage
What do you see in a Anterior genu Lesion?
Akinetic mutism (patient doesnt move or talk)
tactile agnosia (cant sense things with touch)
What do you see with a Posterior Genu Lesion?
Alexia without agraphia: you can write but cant read)
what is Somatoparaphrenia?
patient shows‘delusional’ misidentification, or confabulation, with regards to the affected limb
(“thats not my arm, but shes wearing my ring”)
what is Asomatognosia?
what may cause it?
- not perceiving one side of the body (or ignoring a part of the body)
- neglect or paralysis of limb
say yes** or **no in each part of the table
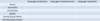

- what is visual agnosia?
- what is color agnosia?
- what is tactile agnosia?
- what is movement agnosia?
- what is anosognosia?
- what is autotopagnosia agnosia?
- what is statognosis?
- what is astereognosis?
- what is auditory agnosia?
- what is prosopagnosia?
- cant recognize an object visually
- cant name or distinguish colors
- cant recognize an object by touching it with either hand
- can’t determine objects that are static or moving
- can’t recognize that you have a disease
- can’t recognize a part of your own body
- can’t recognize spatial positioning of body parts
- tactile agnosia but in both arms
- cant recognize speech, animal sounds, mechanical sounds
- can’t recognize faces
what is constructional apraxia?
cannot reproduce an image
what is this an example of?

neglect
what is this an example of?

contructional apraxia
what is this an example of?
contructional apraxia with neglect
what is neglect?
not recognizing an area of space
what is Papilledema?
non-inflammatory congestion of the optic disc
(papilla) due to increased intracranial pressure.
what is Retinitis Pigmentosa?
hereditary condition causing progressive deterioration of rods, resulting in loss of peripheral vision.
what is Diabetic retinopathy?
Blood vessels swell, proliferate and distort. Will cause blindness if untreated.
what is Proliferative retinopathy?
advanced form of diabetic retinopathy
what do you get if the optic nerve is damaged?
what may cause optic nerve damage?
unilateral blindness
trauma and optic neuritis
what happens if you damage the lateral part of the Optic chiasm?
what may cause bilateral damage to the lateral optic chiasm?
what is the most common cause for damage to the lateral part of the optic chiasm?
binasal hemianopia
internal carotid aneurysm
calcified internal carotid arteries
Damage to CN VI will result in?
there will be what type of diplopia? and only when looking in which direction?
Lack of abduction, medial deviation at rest (strabismus)
Horizontal diplopia only, when looking in direction of lesion.
what is 1 and a half syndrome?
Damage to abducens nucleus may only affect the lateral rectus itself; it may also affect the connections of abducens nucleus to the contralateral, CN III (lateral/horizontal conjugate gaze, reviewed in a few slides).
can result from damage to pons: leading
- Ispilateral CN VI (lateral rectus).
- MLF connection to ispilateral CN III (medial rectus).
- MLF connection to contralateral CN III (medial rectus).
rostral MLF damage can cause what?
what happens if you damage the Frontal Eye Fields?
paralysis of vertical (upward) gaze (Parinauds)
there is no conjugate gaze to the lesioned side and inability of the eyes to look voluntarily to the opposite side.
Damage to frontal eye fields, or PPRF, can be considered as?
supranuclear opthalmoplegia

