Lymphoid Neoplasms Flashcards
Lymphocytosis
Lymphocytosis is an increase in lymphocytes in the peripheral blood.
Absolute Lymphocytosis vs. Relative Lymphocytosis
- Absolute lymphocytosis, a real increase in lymphocytes to greater than 4,000/uL, must be distinguished from relative lymphocytosis, which results from a decrease in neutrophils and/or monocytes.
- In the latter situation, when the neutrophils are decreased, the percentage of lymphocytes in the CBC differential will increase. This does not mean there are more lymphocytes, it just indicates that the neutrophils are reduced—with very different clinical implications.
Absolute Lymphocytosis vs. Relative Lymphocytosis Causes
- Absolute lymphocytosis occurs most often during viral infections or in lymphoid neoplasms.
- Neutropenia, with consequent relative lymphocytosis, occurs most commonly during drug reactions, severe infections, and myelodysplasia (ineffective production) or myeloid leukemia (bone marrow is replaced with malignant blast cells). Lymphopenia can also be caused by viruses, most notably HIV, which destroys the CD4(+) T-helper cells.
Absolute Lymphocytosis Differentials
• Infections
– Viruses: EBV, CMV, HIV
– Chronic bacterial: Tb, cat-scratch
– Pertussis, toxoplasmosis
– LYMPHOCYTOSIS USUALLY TRANSIENT
• Lymphoid neoplasms
– Chronic lymphocytic leukemia
– Others
– Distinguish using morphology, clinical history +/- immunophenotype
Benign (reactive) vs. Neoplastic Lymphocytosis
- Reactive lymphocytes (see image) have many different appearances. They are usually larger than normal lymphocytes with more abundant cytoplasm (light blue to dark blue) and have round to irregular nuclear contours and even prominent nucleoli. These may also be classified as “atypical lymphocytes”. These are seen in a wide variety of clinical settings.
- Clinical note: Be careful when the percent of “atypical” lymphocytes is high. Morphologic distinction between reactive and malignant lymphocytes can be difficult. You can always ask for a Pathologist review of the blood smear. More than 1 lineage (red blood cells, white blood cells, platelets) either high or low is particularly suspicious.

Lymphadenopathy
- Lymphadenopathy is not an uncommon clinical presentation and is usually a reaction to infection, medication, vaccination, immune abnormality or foreign material.
- The key question: is the enlarged lymph node most likely part of a reactive or neoplastic process? The clinical scenario is most helpful: Is there a history of infection, autoimmune disease, immunodeficiency, lymphoma, or other malignancy? Location, timing, and duration may give you clues
Lymphadenopathy Symptoms
- Benign (inflamed) lymph nodes: typically, hot, red, swollen but soft, painful, draining infected areas.
- Malignant lymph nodes are more often painless and hard
- Systemic symptoms – fever, night sweats, weight loss
Three histological patterns of benign (reactive) lymphadenopathy:
1) Cortex containing lymphoid follicles (B-cell zone)
2) Paracortex (T-cell zone; between and deep to follicles)
3) Medulla with medullary sinuses (contain histiocytes)
•In most cases of benign lymphadenopathy, there is distortion or expansion of a functional compartment of the lymph node, but not complete effacement, of the normal lymph node architecture. (Complete effacement or loss of normal nodal architecture is more likely to represent a neoplastic process over a reactive condition)



Benign (reactive) Lymphadenopathy - Follicular Hyperplasia
- Follicular (reaction of B cell germinal centers) hyperplasia: autoimmune, bacterial, HIV, toxoplasmosis
- Increase # of secondary lymphoid follicles

Benign (reactive) Lymphadenopathy - Paracortical Hyperplasia
•Paracortical (T cell) expansion: vaccinations, drug reaction (especially phenytoin), viral infections (especially infectious mononucleosis), skin disorders

Benign (reactive) Lymphadenopathy - Sinus Histiocytosis
•Sinus histiocytosis (expansion of sinus histiocytes): drainage of surgical site or malignancy.

Lymphoid Neoplasms
- Lymphoid neoplasms are a diverse group of entities with heterogeneous morphologic and clinical features. Note that some of the entities can present as either lymphoma or leukemia, or both. These terms were initially used to designate what were considered distinct entities, but with additional study and understanding, these divisions have blurred. The term “leukemia” is used for neoplasms that present with widespread involvement of the bone marrow and usually, but not always, the peripheral blood. “Lymphoma” is used for proliferations that form a tissue mass in a lymph node or extranodal sites.
- Lymphoid neoplasms are grouped based on their clinical aggressiveness into indolent, aggressive and highly aggressive subtypes.
Leukemia Presentation
- Leukemias tend to come to attention as a result of replacement of normal bone marrow elements by the leukemia: anemia causing fatigue, neutropenia predisposing to infections, and low platelet counts with bleeding.
- Young children with acute leukemia may present with bone pain due to the rapid expansion of the leukemia in the bone marrow.
- Patients may also have CNS symptoms (sleepiness, lethargy, headaches) if the CNS is involved.

Lymphoma Presentation
- The majority of patients will present with lymphadenopathy.
- With indolent lymphomas, lymphadenopathy may wax and wane over months to years. In aggressive lymphomas, masses will grow over weeks, and, in highly aggressive lymphomas, the masses may double in size in days.
- The enlarged lymph nodes are usually painless and show no signs of overlying inflammation (if superficial) such as erythema or discharge that are typical of reactive lymph nodes.
- Extranodal disease is seen in about one third of patients, with bone marrow, GI tract and skin the most common sites. Any area of the body/organ can be involved.
-The most common malignancy of testis in men over 60 years of age is lymphoma

Systemic “B” Symptoms of Lymphoma Presentation
•About 1/3 of patients will have systemic (“B”) symptoms:
- Unexplained fever over 38oC
- Drenching night sweats (necessitating a change of clothes or sheets)
- Unexplained weight loss >10% of total body weight
Etiology of Lymphoid Neoplasms
• Chromosomal translocations involving oncogenes
– Immunoglobulin genes and T cell receptors rely on physiologic breakage, recombination and somatic mutations to produce antigen receptor diversity
– Oncogenes can easily be translocated to these regions, then over expressed by the Ig and TCR promoters
• Inherited genetic factors:
– Disorders of genomic instability, Down syndrome, NF type I
• Viruses:
– EBV: Burkitt, Hodgkin, and post-transplant lymphomas
– HTLV: T-cell lymphoma
• Chronic Immune Stimulation
–Helicobacter pylori and MALT lymphoma
–Gluten sensitive enteropathy and intestinal lymphoma
- Immunodeficiency (HIV, iatrogenic)
- Autoimmune diseases
– Sjogren, Hashimoto
Classification of Lymphoid Neoplasms

Histogenic Basis of Classification of Lymphoid Neoplasms

Non-Hodgkin Lymphoma (NHL) versus Hodgkin Lymphoma

Clinical Grouping of Lymphoid Neoplasms

Precursor Neoplasms - Lymphoblastic Leukemia/Lymphoma (ALL)
- These neoplasms are composed of immature B-cells or T-cells (lymphoblasts). The vast majority are B-cell (85%). Cytogenetic abnormalities further divide B-cell ALL into prognostic groups (B-cell lymphoblastic leukemia/lymphoma with recurrent genetic abnormalities).
- Because of the biologic unity of precursor B lymphoblastic leukemia and precursor B lymphoblastic lymphoma, the use of one or the other term in some patients is arbitrary. If the patient presents with a mass lesion and <25% lymphoblasts in the marrow, the designation lymphoma is preferred.
Precursor Neoplasms - Lymphoblastic Leukemia/Lymphoma (ALL) Clinical Features
• The majority (~85%) of precursor lymphoid neoplasms are of precursor B-cell origin that manifest as leukemia with extensive bone marrow, and variable peripheral blood, involvement.
Precursor Neoplasms - Lymphoblastic Leukemia/Lymphoma (ALL) - B-lymphoblastic leukemia
- Usually blasts (presenting as a leukemia) and cytopenia
- Packed marrow (due to blast proliferation) with decreased normal precursors
•Highly aggressive
Precursor neoplasm
•t(9;22) (bcr/abl)– poor prognosis, not present in all cases - more commonly positive in adults than children
-(Remember, this is translocation is also seen in CML)
•hypoploidy —> prognosis unfavorable
•Cytopenia
Bone pain
Precursor Neoplasms - Lymphoblastic Leukemia/Lymphoma (ALL) - T-lymphoblastic leukemia/lymphoma
- May be normal if only lymphoma presentation; if also leukemia, then same as B - Usually blasts (presenting as a leukemia) and cytopenia
- Mediastinal mass (thymus, classic location) – sheets of blasts
•Highly aggressive
Precursor neoplasm
- Mediastinal mass in adolescent male
- Sxs from mediastinal mass (tracheal obstruction, superior vena cava syndrome)

Acute leukemia: Morphology
• Lymphoblasts, as compared to myeloblasts:
– Smaller
– More condensed chromatin
– Inconspicuous nucleoli
– Scant cytoplasm
– Auer rods are not present (as they are in AML)
– Cannot distinguish B-cell versus T-cell by morphology
– Need phenotyping (usually flow cytometry) to distinguish different blasts.
Lymphoblastic leukemia Bone Marrow Morphology

Lymphoblastic leukemia/lymphoma: Morphology

B-lymphoblastic leukemia: prognosis

Mature B Cell Neoplasms
– Chronic lymphocytic leukemia
– Hairy cell leukemia
– Follicular lymphoma
– Diffuse large B cell lymphoma
– Burkitt lymphoma
– MALToma
– Mantle cell lymphoma
– Lymphoplasmacytic lymphoma
– Plasma cell neoplasms
Mature B Cell Neoplasms - Chronic lymphocytic leukemia (CLL) and small cell lymphocytic lymphoma (SLL)
- CLL is the most common leukemia of adults in the Western world. 15,000 new cases are diagnosed per year in the U.S.
- CLL and SLL differ only in the degree of peripheral blood lymphocytosis and some consider them to be one disease at different stages.
- This is a disease of adults with a median age of diagnosis at 60 yrs.
•Mature B Cell Neoplasms - Chronic lymphocytic leukemia (CLL) and small cell lymphocytic lymphoma (SLL) Features
- By definition, the patient has lymphocytosis; +/- cytopenias
- Small, mature lymphocytes with scant cytoplasm and smudge cells
- Indolent; treated when criteria met
- Anemia can be multifactorial: marrow infiltration, red blood cell aplasia, marrow suppression, autoimmune hemolysis.
Immunodeficiency
- hypogammaglobulinemia, cell mediated immunity
- Flow cytometry: CD5+ monoclonal B-cells
- Richter’s transformation to diffuse large B-cell lymphoma
Mature B Cell Neoplasms - Chronic lymphocytic leukemia (CLL) and small cell lymphocytic lymphoma (SLL) Clinical Manifestations
- Asymptomatic
- 25% with lymphocytosis on routine CBC
- Nonspecific symptoms
- Easy fatigability, weight loss, anorexia
- Generalized lymphadenopathy and hepatosplenomegaly
- <10% of patients present with a non-leukemic picture having only nodal involvement (SLL)
- Leukocyte count is highly variable
-Diagnostic criteria for CLL:
Sustained monoclonal lymphocytosis > 5,000/uL

Mature B Cell Neoplasms - Chronic lymphocytic leukemia (CLL) and small cell lymphocytic lymphoma (SLL) - Morphology

Mature B Cell Neoplasms - Chronic lymphocytic leukemia (CLL) and small cell lymphocytic lymphoma (SLL) - Immunophenotype
•Monoclonal B-cells (CD20+, CD19+) that express CD23 and CD5

Mature B Cell Neoplasms - Chronic lymphocytic leukemia (CLL) and small cell lymphocytic lymphoma (SLL) - Prognosis and Survival
- Staging: based on presence/absence of lymphadenopathy, organomegaly, anemia and/thrombocytopenia
- Genetic Features also predict prognosis
– Most common findings
* Good: del13q, trisomy 12
* Poor: del17p (p53 gene)
• Survival:
– Natural history of CLL is extremely variable
– >10 years for patients with minimal tumor burden
– If large cell transformation (Richter transformation) occurs, then survival is less than 1 year
Mature B Cell Neoplasms - Hairy Cell Leukemia
•Hairy cell leukemia is an uncommon, indolent, lymphoid malignancy accounting for only 2% of all leukemia with <1000 cases per year nationwide.
Mature B Cell Neoplasms - Hairy Cell Leukemia Features
•Pancytopenia; rare hairy cells in circulation (lymphocytosis not typical)
•Fried-egg appearance
Hairy projections
Dry tap
Marrow fibrosis
•Indolent; good prognosis
•-TRAP+
-BRAF mutation (treatment with BRAF inhibitor – Vermurafenib)
•Cytopenia
Splenomegaly
Mature B Cell Neoplasms - Hairy Cell Leukemia Clinical Features
•HCL is most common in older men, who present with pancytopenia and splenomegaly. Infectious associated with neutropenia, fatigue from anemia, petechiae from thrombocytopenia, and abdominal fullness or early satiety from splenomegaly are common symptoms.
Mature B Cell Neoplasms - Hairy Cell Leukemia Morphology
- The name is derived from the characteristic appearance of the neoplastic B-cells seen in the blood and bone marrow with “hairy” cytoplasmic projections.
- The bone marrow is frequently fibrotic leading to a “dry tap” (meaning no liquid bone marrow is obtained when attempting a bone marrow aspirate). •The abundant cytoplasm causes the cells to be spaced relatively far apart in the bone marrow leading to a “fried egg” appearance.
- The red pulp of the spleen is characteristically infiltrated.

Mature B Cell Neoplasms - Hairy Cell Leukemia Pathogenesis
•Mutation in the BRAF oncogene leads to constitutive activation of the RAF-MEK-ERK mitogen activated signaling pathway leading to cell division and differentiation.
– Same mutational “hotspot” as reported in melanoma
Mature B Cell Neoplasms - Hairy Cell Leukemia Prognosis
– Excellent with appropriate chemo
– BRAF inhibitors
Mature B Cell Neoplasms - Follicular Lymphoma
•Most common indolent non-Hodgkin lymphoma
Mature B Cell Neoplasms - Follicular Lymphoma Features
•Normal to cytopenias (depends on degree of marrow involvement); may have circulating lymphoma cells
•Lymph node with back to back follicles consisting of small cleaved cells
BCL-2+ germinal centers (reactive germinal centers are BCL-2-negative)
•Indolent (most common indolent lymphoma)
•-t(14;18) – places the BCL2 gene on chr 18 next to the immunoglobulin heavy chain promoter (IGH) on chr 14, resulting in overexpression of BCL-2 protein which is anti-apoptotic (cells immortalized, do not undergo apoptosis).
-Transformation to diffuse large B-cell lymphoma
•Lymphadenopathy, may wax and wane (come and go); usually slow growing
Mature B Cell Neoplasms - Follicular Lymphoma CLinical Features
•Adults (some variants occur in children), usually multiple lymph node sites involved at presentation, otherwise asymptomatic, variable relapsing course (“wax and wane”)
Mature B Cell Neoplasms - Follicular Lymphoma Morphology
- Neoplastic germinal center cells recapitulate a normal germinal center resulting in a nodular pattern.
- The cells are a mixture of small and large cells with irregular nuclear contours (“cleaved”).
- Some cases transform to diffuse large B-cell lymphoma (sheets of large cells, no germinal center formation)

Mature B Cell Neoplasms - Follicular Lymphoma Pathogenesis
- Diagnostic hallmark: t(14;18) that translocates the BCL-2 gene next to the promoter of the immunoglobulin heavy chain gene (on chromosome 14).
- This leads to increased expression of the anti-apoptotic BCL-2 protein and immortalizes the cells.

Mature B Cell Neoplasms - Follicular Lymphoma Prognosis
- Median survival with most current therapies is estimated at >90% at 5 years.
- May transform into an aggressive lymphoma such as diffuse large B cell lymphoma; prior to rituximab therapy, transformed cases had poor prognosis.
Mature B Cell Neoplasms - Mantle Cell Lymphoma
•Accounts for 3-5% of non-Hodgkin lymphoma
Mature B Cell Neoplasms - Mantle Cell Lymphoma Clinical Features
- Adults (median age 60 yrs).
- Lymph nodes are most common site of involvement; spleen, marrow with or without blood involvement are other important sites of disease).
- GI tract frequently involved.
Mature B Cell Neoplasms - Mantle Cell Lymphoma Morphology
•Composed of small lymphocytes with slightly irregular nuclear contours.

Mature B Cell Neoplasms - Mantle Cell Lymphoma Immunophenotype
•Monoclonal B-cells (CD20+, CD19+) that express CD5
Mature B Cell Neoplasms - Mantle Cell Lymphoma Pathogenesis
•Diagnostic hallmark: t(11;14) that translocates the Cyclin D1 gene next to the promoter of the immunoglobulin heavy chain gene is seen in >95% of cases.
Mature B Cell Neoplasms - Mantle Cell Lymphoma Prognosis
•Variable clinical course; some patients with only blood and bone marrow involvement have an indolent course. Others have a more aggressive clinical course
Mature B Cell Neoplasms - Diffuse Large Cell Lymphoma (DLBCL)
•The most common type of lymphoma in adults.
Mature B Cell Neoplasms - Diffuse Large Cell Lymphoma (DLBCL) - Features
- Variable; neoplastic cells may circulate late in disease
- Sheets of large B-cells effacing architecture
- Aggressive (most common of the aggressive forms)
•-May have t(14;18) which suggests transformation from follicular lymphoma
-Treatment with multiagent chemotherapy with Rituximab
•Lymphadenopathy, or symptoms of a mass outside lymph node (CNS, GI tract, etc)
Mature B Cell Neoplasms - Diffuse Large Cell Lymphoma (DLBCL) Clinical Features
- Adults (Median age: 60 years), can occur in children and young adults.
- Patients present with rapidly enlarging, mass at single nodal or extranodal site including GI, skin, bone, brain.
- May have fever, night sweats, weight loss, fatigue.
Mature B Cell Neoplasms - Diffuse Large Cell Lymphoma (DLBCL) Morphology
•Large lymphocytes in a diffuse sheet-like pattern (no nodular areas as we see in follicular lymphoma)

Mature B Cell Neoplasms - Diffuse Large Cell Lymphoma (DLBCL) Prognosis
•65% 5-year disease free survival with combined monoclonal antibody (Rituximab) and intensive chemotherapy
Mature B Cell Lymphomas - Immunodeficiency Associated Large B Cell Lymphoma
- Occurs in HIV, post-transplant patients, and inherited immunodeficiency disorders.
- Often arise from B-cells which are latently infected with EBV. Reduced immunosurveillance allows abnormal B cell clones to develop.
- May regress with restoration of T cell immunity (treatment of HIV, decreasing iatrogenic immunosuppression).
Mature B Cell Lymphomas - Immunodeficiency Associated Large B Cell Lymphoma Features
- CBC Variable
- Sheets of large B-cells effacing architecture
- Aggressive; May regress with restoration of immune system, often treated with chemotherapy
•-Seen in HIV, post-transplant (related to immunosuppression that prevents organ rejection), inherited immunodeficiency
-Often EBV-positive
•Lymphadenopathy, or symptoms of a mass outside lymph node (CNS, GI tract, etc)
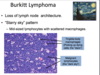
Mature B Cell Lymphomas - Burkitt Lymphoma Features
- Variable – normal to cytopenias; neoplastic cells may circulate
- Sheets of small to medium-sized cells with Starry sky background (macrophages eating dying neoplastic cells); mitotic figures
- Highly aggressive
•-Children; HIV+
-t(8;14)- MYC oncogene translocated to IGH promoter results in overexpression of myc and proliferation
EBV+
•Mass lesion - Africa: Jaw, facial bones; Non-African cases: abdominal mass is most common location
Mature B Cell Lymphomas - Burkitt Lymphoma Clinical Features
- Highly aggressive neoplasms with explosive growth.
- Three epidemiologic variants are recognized which differ in geographical distribution, clinical presentation, and biological features.
1) Endemic:
o Africa (regions endemic for malaria). Most common childhood malignancy.
o >95% EBV+
o Jaw, other facial bones in majority of cases; other sites: GI tract, kidney, breast
2) Sporadic:
o Worldwide, mainly children and young adults
o ~30% EBV+
o Abdominal masses – ileocecal region; other sites include ovaries, kidney, breast
3) Immunodeficiency-associated:
o HIV+ patients
o 25-40% EBV+
o Nodal, bone marrow

Mature B Cell Lymphomas - Burkitt Lymphoma Morphology
•Medium-sized cells in a starry sky pattern created by macrophages engulfing apoptotic tumor cells (tingible-body macrophages); numerous mitoses
Mature B Cell Lymphomas - Burkitt Lymphoma Pathogenesis
- EBV is one factor in a multi-step pathogenesis. EBV infects epithelial cells of the oropharynx and then B lymphocytes via CD21 expressed on B cells. Within B cells, the linear genome of the EBV circularizes in the cell nucleus. The infection is then latent since there is no replication of the virus, and the B cells are not killed (they are immortalized).
- Most patients remain asymptomatic or develop self-limited infectious mononucleosis. In other patients, for unrecognized reasons, there is sustained proliferation of the EBV immortalized B cells, which are then at risk for genetic changes, such as the t(8;14).
- This translocation places the MYC oncogene adjacent to the immunoglobulin heavy chain gene promoter leading to over-expression of the MYC cell cycle regulator, thereby promoting proliferation
Mature B Cell Lymphomas - Burkitt Lymphoma Prognosis
•60-90% cure with intensive multiagent chemotherapy
Mature B Cell Lymphomas - Marginal Zone Mymphoma of MALT (MALToma) Features
- Usually normal CBC
- Reactive-appearing germinal centers are surrounded by proliferation of cells in the marginal zone area that infiltrate the lamina propria and into the epithelium
•Indolent
May be treated with antibiotic therapy directed against eradicating H. pylori
- H. pylori
- Mass lesion at an extranodal site; stomach most common, also conjunctiva, skin, lung
Mature B Cell Lymphomas - Marginal Zone Mymphoma of MALT (MALToma) Clinical Features
- Most cases occur in adults.
- Extranodal mass (stomach, conjunctiva, skin, lung).
- Indolent.
Mature B Cell Lymphomas - Marginal Zone Mymphoma of MALT (MALToma) - Pathogenesis
- These lymphomas arise in chronically inflamed tissues involved by either autoimmune disorders (thyroid, salivary glands) or infection (stomach, lung, skin, conjunctiva).
- In the stomach, MALT lymphomas are highly associated with presence of helicobacter pylori.
- The lymphoma begins as a reactive polyclonal process, over time a monoclonal B cell population emerges, which then acquires further genetic changes.

Mature B Cell Lymphomas - Marginal Zone Mymphoma of MALT (MALToma) Morphology
•Neoplastic cells surround reactive germinal centers and infiltrate surrounding epithelium (lymphoepithelial lesions).

Mature B Cell Lymphomas - Marginal Zone Mymphoma of MALT (MALToma) Prognosis
- Indolent in early stages. Early gastric lesions may be treated with H. pylori eradicating antibiotics.
- Local radiation or chemotherapy in some patients.
Mature B Cell Lymphomas Lymphoplasmacytic Lymphoma (Waldenstrom Macroglobulinemia) Clinical Features
- Adults. Patients present with weakness and fatigue due to anemia.
- Some patients have a monoclonal IgM protein and bone marrow involvement meeting criteria for Waldenstrom macroglobulinemia.
- In some patients with high levels of the IgM protein present with symptoms of hyperviscosity (mucosal bleeding, visual changes, and neurologic symptoms – vertigo, somnolence, headache, seizures, paresthesias).
Mature B Cell Lymphomas Lymphoplasmacytic Lymphoma (Waldenstrom Macroglobulinemia) Morphology
•Mixture of small lymphocytes, plasmacytoid lymphocytes, and plasma cells

Mature B Cell Neoplasms - Plasma Cell Neoplasms
- A group of mature B-cell disorders characterized by a proliferation of clonal plasma cells that produced a monoclonal immunoglobulin, referred to as an M-protein (M, for myeloma).
- This group of disorders includes the pre-malignant monoclonal gammopathy of undetermined significance (MGUS) and plasma cell neoplasms (plasmacytoma, plasma cell myeloma).
Mature B Cell Neoplasms - Plasma Cell Neoplasms - Plasma Cell Myeloma
•Clinical features
– Monoclonal protein
- IgG (50%), IgA (20%), light chain only (20%)
- Picked up incidentally (MGUS)
– Bone pain is the most common presenting Sx
• Factors produced by plasma cells cause bone lysis
– Hypercalcemia (confusion, weakness, lethargy, polyuria)
– Infection
Mature B Cell Neoplasms - Plasma Cell Neoplasms - Plasma Cell Myeloma Epidemiology
– ~32,000 new cases in 2020 (1.8% of all new cancers)
– Peak incidence: 65-70 years
• Very infrequent in adults <30 yrs
– Higher incidence in men and those of African descent
Mature B Cell Neoplasms - Plasma Cell Neoplasms - Plasma Cell Myeloma Prognosis
•Prognosis: 5-year survival is 54%
Mature B Cell Neoplasms - Plasma Cell Neoplasms - Plasma Cell Myeloma CRAB
1) Growth of plasma cells in bones, leading to lytic bone lesions and pathologic fractures. Bone pain is the most common presenting symptom. Hypercalcemia can give rise to confusion, weakness, lethargy, constipation and polyuria, and can contribute to renal disease.
2) Production of excessive immunoglobulins: Renal insufficiency is multifactorial; however, the most important risk factor is Bence-Jones proteinuria (free light chains in urine) – light chains are toxic to renal tubular epithelial cells.
3) Suppression of normal humoral immunity: Impairment of normal Ig production leads to risk of bacterial infection. Cellular immunity is relatively unaffected.

Mature B Cell Neoplasms - Plasma Cell Neoplasms - Plasma Cell Myeloma Lytic Bone Lesions

Mature B Cell Neoplasms - Plasma cell neoplasms Morphology
- Biopsies of bone lesions (or extraskeletal lesions), or bone marrow biopsies show a proliferation of monoclonal plasma cells.
- The peripheral blood may demonstrate RBCs sticking together in a linear array (Rouleaux formation).
- Rarely, plasma cells may enter the peripheral blood (plasma cell leukemia). Solitary lesions can occur in bone or soft tissue (plasmacytoma).

Mature B Cell Neoplasms - Plasma Cell Neoplasms - Plasma Cell Myeloma Prognosis
•On average, about 1% of people with MGUS go on to develop multiple myeloma each year. In myeloma, survival varies with stage. In general, 5-year survival for myeloma is 54%
Hodgkins Lymphoma Features
- Varaiable CBC
- Reed-Sternberg cells and variants are infrequent and surrounded by reactive inflammatory cells (lymphocytes, eosinophils, histiocytes, plasma cells)
- Aggressive
- -Some are EBV+
- Contiguous spread
- Do not express most B-cell markers (CD20-negative)
•Cervical lymphadenopathy and mediastinum are common sites of involvement; usually nodal
Hodgkins Lymphoma Clinical Features
•0.7% of all new cancers. One of the most common cancers of young adults, particularly young women, median age 32. Arises in a single node or lymph node chain and shows predictable spread: lymph nodes to spleen to liver to bone marrow.
Hodgkins Lymphoma Morphology
•Infrequent large atypical cells called Reed-Sternberg cells are seen in a cellular background rich in lymphocytes, eosinophils, plasma cells, and/or histiocytes.
-Reed-Sternberg cells are large mononucleated or multinucleated cells, with prominent nucleoli resembling viral inclusions.
•Four morphologic variants are described:
1) Nodular sclerosis: Most common type. Nodules of inflammatory cells and lacunar cells (Reed-Sternberg variant) surrounded by bundles of collagen. Lacunar cell cytoplasm retracts leaving the cell sitting in an empty hole (lacuna).
2) Mixed cellularity: Inflammatory cells plus RS cells. No fibrosis.
3) Lymphocyte rich: Reactive lymphocytes make up the majority of the infiltrate.
4) Lymphocyte depleted: Paucity of lymphocytes and a relative abundance of RS cells.

Hodgkins Lymphoma Immunophenotype
•The RS cells are B-cells but they fail to express the usual B-cell markers including CD20. They are positive for CD30 and CD15
Hodgkins Lymphoma Prognosis
•Hodgkin Lymphoma is frequently curable with multi-agent chemotherapy.
Mature T Cell Neoplasms Mycosis Fungoides (MF)/ Sezary Syndrome Features
- CBC isolated to the skin; when Sezary syndrome will have abnormal cells in blood
- Small to medium in size, irregular T-lymphocytes (cerebriform) in the dermis and invading the epidermis – Pautrier’s microabscess
•MF – indolent, Sezary more aggressive
Most common T-cell lymphoma
•-Cerebriform cells (in skin and in circulation when Sezary)
-CD4+ T-cells
•MF – patch –> plaque
–> tumor stages
Sezary – lymph node involvement and diffuse skin erythema
Mature T Cell Neoplasms Mycosis Fungoides (MF) Clinical Features
- Most common of the T-cell lymphomas, most common cutaneous lymphoma. Usually adults.
- Older adults. Erythematous patch–> plaque–> tumor nodule.

Mature T Cell Neoplasms Mycosis Fungoides (MF) Morphology
•Band like infiltrate of CD4+ T-lymphocytes with convoluted nuclei that show clustered invasion of the epidermis forming Pautrier microabscesses.

Mature T Cell Neoplasms Mycosis Fungoides (MF) Prognosis
•Indolent to aggressive. Excellent prognosis with limited disease.
Mature T Cell Neoplasms Sezary Syndrome Clinicopathologic Features
•Seen in Adults. Defined by the following triad:
- Erythroderma
- Generalized lymphadenopathy
- Presence of clonally related T-cells with cerebriform nuclei (Sezary cells) in skin, lymph nodes, and blood.

Mature T Cell Neoplasms Sezary Syndrome Morphology
•Microscopic features in skin may be similar to MF. Sezary cells have cerebriform nuclei.

Mature T Cell Neoplasms Sezary Syndrome Prognosis
•Poor, 10-30% 5 year-survival
Mature T Cell Neoplasms Adult T-cell leukemia/lymphoma (ATLL) Clinical Features
- Occurs only in adults (Median age: 58 years).
- Disease is widely disseminated in most patients at diagnosis with lymph node, skin and blood involvement.
- Endemic in several regions of the world (regions in Japan, Caribbean, and Africa).
- Hypercalcemia.
Mature T Cell Neoplasms Adult T-cell leukemia/lymphoma (ATLL) Morphology
•Leukemic cells show remarkable pleomorphism with multilobed nuclei (“flower cells”).
•

Mature T Cell Neoplasms Adult T-cell leukemia/lymphoma (ATLL) Pathogenesis
•Causally linked to HTLV
Mature T Cell Neoplasms Adult T-cell leukemia/lymphoma (ATLL) Prognosis
•Poor in disseminated cases
Work Up
•The work up begins with a thorough clinical history including the presence, timing, and course of lymphadenopathy, other masses or rashes, questions regarding systemic symptoms, symptoms or signs related to altered CBC values (fevers, infections, fatigue, easy bruising) or symptoms that could be secondary to extranodal organ extension (e.g., early satiety from a gastric mass). Patients should also be asked about risk factors (immune suppression, autoimmune diseases, infections, radiation/toxic exposure, family history).
Physical exam should include:
(1) All peripheral lymph nodes (cervical, supraclavicular, axillary, inguinal, and femoral)
(2) Other lymphoid organs such as tonsils and spleen
(3) Signs of bone marrow involvement: signs of anemia, or thrombocytopenia
(4) Lymphoid pressure on the veins: limb swelling
(5) Testicular exam if suspecting aggressive lymphoma
Laboratory tests:
- Complete blood count with Pathologist review for “atypical lymphs” or “blasts”
- Comprehensive metabolic panel (liver and kidney function)
- LDH and/or sedimentation rate (depending on type of lymphoma)
- If suspect tumor lysis: calcium, phosphorus, uric acid • HIV test if suspecting Hodgkin or high-grade lymphoma
Imaging:
- CT chest, abdomen, pelvis
- CT neck if involved (clinical exam is usually sufficient)
- Positron emission tomography (PET) scan in select cases (particularly diffuse large Bcell lymphoma and Hodgkin)
Pathology
- Lymph node excisional biopsy, or evaluation of involved site (adequate tissue!)
- Bone marrow evaluation for diagnosis of suspected lymphoid leukemia and staging of lymphomas. Peripheral blood flow cytometry may be adequate for CLL.
- Lumbar tap needs to be performed for suspected highly aggressive diseases (Burkitt lymphoma and ALL)


