Lungs Flashcards
Source of lower respiratory organs
Respiratory primordium. ~28 days
Largnotracheal Groove
Buds off gut tube anteriorly (THINK: ends up in front of the esophagus). Outgrowth from the caudal end of the ventral wall of the primordial pharynx, caudal to the 4th pair of pharyneal pouches.

Laryngotracheal Diverticulum
Forms at the end of the 4th week ventral to the caudal part of the foregut. Elongates and is invested with splanchnic mesenchyme. Its distal end enlarges to form the globular respiratory bud. Responsible for the tracheal bud, which goes on to develop into primary bronchial buds. Maintains communication with pharynx through primordial laryngeal inlet

Primordial laryngeal inlet
Opening of the laryngotracheal tube into the pharynx. Allows communication between developing trachea and pharynx.

Tracheoesophageal folds
Divide gut tube into trachea and esophagus. Folds together to form full separation between trachea and esophagus. Develop in the posteroinferior aspect of the laryngotracheal diverticulum. Approach each other and fuse, becoming the tracheoesophageal septum

Tracheoesophageal Septum
Formed by fusing of tracheoesophageal folds. Divide ventrally into the laryngotracheal tube and dorsally into the oropharynx and esophagus. Failure of this to divide properly results in a fistula.
Tracheoesophageal Fistula
Abnormal presence of a connection between trachea and esophagus. If the tracheoesophageal septum does not form, there is a common tube between the trachea and esophagus allowing for fluids to get into lungs. BAD!

Laryngotracheal Tube
Its distal end (the tracheal portion) differentiates into the trachea starting at the 4th week. The position of this tube gives this bud its new name: respiratory (tracheal) bud. Its endodermal lining is comprised of epithelium and glands of the trachea and has overlying splachnic mesenchyme: cartilage, connective tissue, and muscles of the trachea.
Primary bronchial buds
As the tracheal bud continues to grow inferiorly, the two primary bronchial buds are formed as twin outpouchings. Bronchial buds formed from endoderm grow laterally into the mesenchyme surrounding the pleuroperitoneal canals and primordia of the pleural cavities. Endodermal lining: epithelium and glands of bronchial branches. Overlying splanchnic mesencyme: cartilage, connective tissue, muscles of bronchi, and visceral pleura.

Mainstem bronchi/primary bronchi
Early 5th week, mainstem/primary bronchi form. Right main bronchus larger and oriented more vertically than left main bronchi. Main bronchi further develop into secondary lobar bronchi. By 7th week, segmental (tertiary) bronchi develop with surrounding mesenchyme foring the bronchopulmonary segments. By 24 weeks, 17 orders of branches, respiratory bronchioles have developed (more and more branching)

Maturation of lungs
Pseudoglandular period (6-16 weeks), canalicular period (16-26 weeks), Terminal sac perior (26wks to birth), Alveolar period (32wks-8 years)
Pseudoglandular period
Weeks 6-16. During this time lung has distinctly glandular appearance created by small epitheal-lined tubules surrounded by abundant mesenchyme. By week 16, all bronchial airways have been formed. Further growth occurs by elongation and widening of existant airways; not by further branching.

Canalicular perior
Weeks 16-26. Basic structure of gas-exchanging portion of lung is formed and vascularized. Lumina of the bronchi and terminal bronchioles enlarge and the lung tissue becomes highly vascular; respiration is possible at the end of this period because some thin-walled terminal saccules have developed at the ends of the respiratory bronchioles. A fetus born at the end of this period may survive if it receives intensive care

Respiratory Bronchioles
Initially develop during canalicular stage of development from dividing of bronchi. Narrowest airways in lungs. Deliver air to exchange surfaces to lungs
Alveolar ducts
Small ducts that connect respiratory bronchioles to alveolar sacs; contain a collection of alveoli.
Terminal saccules
Thin walled dilations at ends of respiratory bronchioles. Will develop into alveoli; termed Primordial alveoli.
Alveolar Period
32 weeks to 8 years. Development of alveoli is mostly done by 3 years, but new alveoli may be added until 8 years of age. Primordial alveoli appear as bulges on the walls of respiratory bronchioles. After birth, the primordial alveoli increase in size, forming mature alveoli. 150 million alveoli present in newborn infant; between 3-8 years old, 300 million mature alveoli achieved!

Trachea
Found below larynx, in front of esophagus. Begins at C6, ends at sternal angle (T4-T5). C-shaped cartilages, open posteriorly: cartilages closed by trachealis muscle.
Right primary bronchus
Wider, shorter, and more vertical than left primary bronchus. ~2.5 cm long. If a foreign body is aspirated, it’s likely going to be found in the right lung as a result of the shorter and more vertical path to the right lung.

Left primary bronchus
Passes inferolaterally, inferior to aortic arch, anterior to the esophagus and descending aorta. Longer and more narrow than right primary bronchus.

Carina
Site of bifurcation of left and right primary bronchi. Keel-like ridge located between orifices. Important for bronchoscopy

Aortic Arch
Runs right to left, found over left primary bronchus.
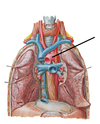
Azygos vein
Forms arch over right priamry bronchus below superior vena cava. Runs directly into superior vena cava.

Lungs
Lungs have lobes and fissures, giving rise to the segmental nature so that lung can function even with part of it damaged.

Right Lung
Larger than the left lung, has one more lobe. Has upper, middle, and lower lobes. Oblique AND horizontal fissures present.

Left lung
Smaller than right lung, has one fewer lobe due to the heart sitting slightly more on left. Has upper and lower lobes. Has an oblique feature, and CAN have a horizontal fissure but doesn’t have to. Lingula sits on the upper lobe of left lung.

Lingula
Projection of upper lobe of left lung, sits next to the base.

Apex
Coming up toward thoracic inlet. Near neck

Base
Sits on diaphragm

Cardiac notch
Upper lobe of left lung. Where the heart sits

Surfaces of the lungs
PLANAR. Cervical, costal, mediatstinal, and diaphragmatic
Cervical Surface
Apex

Costal surface
Surface of the lungs that touch the ribs

Mediastinal surface
Surface in contact with with mediastinal pleura. Wheres vessel in and out of in contact with HEART are. In back.

Diaphragmatic Surface
Surface in contact with diaphragm. Base of lungs. In back

Borders of the lungs
Edges. Anterior, anterior, and inferior.
Anterior border
Anterior spine/edge

Posterior border
Rounded ridge parallel to vertebral column

Inferior border
Crown around diaphragm

Hilum of lung
Depression or pit at part of organ where vessels and nerve enter

Roots of lung
Structures going in and out of lung. Present in the hilum. Pulmonary arteries and veins, bronchus, bronchial arteries and veins, nerves, and lymphatics
Pulmonary ligament
Formed by reflection of parietal pleura as it becomes visceral pleura

Pulmonary artery
Pulmonic circulation, going TO lung to get oxygen. Typically superior to pulmonary veins

Pulmonary vein
Pulmonic circulation, going FROM lung TO heart with oxygen in it. Typically inferior to pulmonary artery.

Bronchus
Cartilaginous, large for air flow. Thick tube, wide for air flow, kept open by cartilage

Respiratory Tree
Primary bronchus –> secondary/lobar bronchus –> segmental bronchi/bronchopulmonary segments –> terminal bronchioles –> respiratory bronchioles –> alveolar ducts –> alveolar sacs

Bronchopulmonary segment
Surgical unit of lung. Pyramidal in shape. At base-peripheral, apex-hilum. Separated by avascular septa. Has own segmental artery, bronchus, and vein.

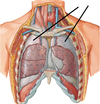
Pleura
Double-layered serous membrane with capillary layer of serous fluid. Pleura reduces friction between pleural layers as lungs expand/contract during inspiration/expiration
Visceral pleura
Inner layer of membrane. Remains closely attached to the lung (moves with lung as lungexpands and relaxes) and cannot be separated.

Parietal pleura
Outer layer of membrane. Stays attached to the internal surface of the thoracic wall by the endothoracic fascia.
Divisions of parietal pleura
Parts of this layer are named as they relate to the surface to which they contact: cervical surface, costal surface, mediastinal surface, diaphragmatic surface

Pleural cavity
Space between two pleural membranes

Pleural reflections
Specific pleural surface becomes another pleural surface. These reflections form spaces that are potential spaces within pleural cavity which can fill with fluid. These are termed recesses: costodiaphragmatic recess and costomediatinal recess
Costodiaphragmatic recess
Potential space at junction of costal pleura and diaphragmatic pleura (runs rib 6 to rib 8). Lungs expand into this space during forced inspiration. Gives the lungs space to grow while expanding. During expiration, this space is filled with fluid

Costomediastinal recess
potential space at the border of the mediastinal pleura and the costal pleura. It helps the lungs to expand during deep inspiration. Not as significant as costodiaphragmatic recess as it has a smaller volume. Most obvious in the cardiac notch of the left lung.

Pulmonary plexus
Anterior and posterior plexi related to carina. Convey nerves from pulmonary branch of vagus, recurrent laryngeal of vagus, and sympathetic trunk to give nerve supply to lungs: sympathetics and parasympathetics. Sympathetics: vasoconstrictors and bronchodilators. Parasympathetics: vasodilators, bronchoconstrictors, secretomotor, and afferents.

Cough reflex
Parasympathetics of lung (recurrent laryngeal of vagus). Located around carina is an irritant receptor –> Coughing
Respiratory Control
Parasympathetics of lung. Stretch receptors located in bronchial tree
Costal and cervical pleura nerve supply
Local intercostal nerves
Mediastinal pleura nerve supply
Phrenic Nerve
Diaphragmatic nerve supply
Central portion: phrenic nerve. Peripheral part: local intercostal nerves
Visceral pleura nerve supply
TRICK QUESTION. Insensitive to pain and pressure
Lymphatics of lung
Superficial lymphatic plexus and deep lymphatic plexus
Superficial lymphatic Plexus
Deep to visceral pleura, draining lung and visceral pleura. Vessels drain into superior and inferior tracheobronchial lymph nodes. Chicken-wire tracks. Flow toward the hilum.

Deep lymphatic plexus
Lymph vessels within the lamina propia of the bronchi –> Pulmonary lymph nodes (located along large branches of main bronchi) –> Bronchopulmoanry lymph nodes (hilar nodes) –> Superior and inferior (carinal) tracheobronchial lymph nodes –> bronchomediostinal lymph nodes (formed from vessels from parasternal, tracehobronchial, and anterior mediastinal lymph nodes) –> split depending on side. Left side to thoracic duct, right side to right lymphatic duct.

Lympathics of alveoli
NO LYMPHATICS OF ALVEOLI


