Lower GI Developmental Pathology Flashcards
Which of the pictured anomalies of the trachea and esophagus is most common?

(Far left - 85%)
What is the VACTERL complex?
Association of several major classes of congenital anomalies
- Vertebral
- Anorectal
- Cardiac
- TEF
- Renal
- Limb
What prenatal and neonatal findings are consistent with TEF?
- Polyhydramnios
- Small stomach
- Prominent proxinal pouch
- Abnormal swallowing
- VACTERL association
- Excessive salivaiton, mucous
- Feeding intolerance
- Failure to pass NG/OG
Physiologic jaundice is a common finding in neonates. What (3) factor contribute to neonatal physiologic jaundice.
When should bilirubin begin to decrease in the infant?
Under what conditions should an infant be evaluated for abnormal jaundice (non-physiologic)?
Physiologic Jaundice
- Decreased RBC half-life compared to adults
- Immature liver has decreased capacity to conjugate/excrete bilirubin
- Decreased enterohepatic circulation
Bilirubin levels should begin to decline around Day 6-7
Abnormal jaundice:
- Jaundice beyond 2-3 weeks of age
- Direct bilirubin >2mg/dL
- Total bilirubin >12mg/dL in a term infant
- Total bilirubin >14mg/dL in a pre-term infant
When does neonatal biliary atresia typically present? Name some key findings.
Typical presentation: 4-6 weeks
Findings:
- Conjugated hyperbilirubinemia
- Acholic (light) stool, dark urine (coca-cola urine)
- Ultrasound abnormalities (gallbladder, spleen, situs inversus, etc)
- Abnormal IDA scan
- r/o other pathologies
Children with congenital biliary atresia typically require liver transplant or portoenterostomy by what age?
2 y.o. (death otherwise)
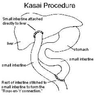
Describe the Kasai Procedure
Aproximately how many children achieve good long-term results?
Kasai Procedure
- Expose porta hepatis
- Transect small intestine (proximal jejunum?)
- Suture distal free end to porta hepatis
- Suture proximal free end to section of small bowel distally to porta hepatis
1/3 have good long-term results (especially if treated before 90 days old to avoid onset of bridging fibrosis)
Describe (3) important elements of postoperative care following the Kasai procedure for biliary atresia
- Supplement fat-soluble vitamins (ADEK) and monitor levels
- UDCA 20mg/kg per day for 2 years
- Ampicillin prophylaxis for chalangitis
What are the two most common types of choledochal cyst? Are they intra-hepatic or extra-hepatic?
What is the treatment commonly used for these two types?
Type I (77-90%) and Type IV (15%)
Both are extra-hepatic
Treatment: Excision with hepatico-jejunostomy or duodenostomy (with or without liver resection)
Give (4) processes that are pathogenic for congenital choledochal cysts
- Disordered organogenesis
- Pancreaticobiliary malunion
- Acquired weakness
- Distal obstruction
What type of anatomic variation of the pancreatic-biliary tree predisposes children to congenital coledochal cysts? Why?
Long common channel (>2cm)
The long common channel likely increases incidence of reflux of pancreatic enzymes into the bile ducts, causing irritation and cyst formation
What cancer is a common late complication of congenital coledochal cysts?
Biliary adenocarcinoma
Bilious emesis (any shade of yellow or green) in an infant… how bad?
SURGICAL EMERGENCY
What are Ladd’s Bands? How are these relevant to congenital malrotation of the gut?
What is Ladd’s procedure?
Ladd’s Bands: stalks of peritoneal tissue that attach the cecum to the abdominal wall. In malrotation, they may cross the duodenum and contribute to obstruction.
Ladd’s Procedure
- Untwist bowel
- Take down Ladd’s bands
- Widen mesentary (by cutting)
- Place small bowel on the right side, colon on the left side
- Perform appendectomy (so a future ER physician is not fooled by appendicitis symptoms presenting on the left side)
The Ligament of Treitz should always be *where* relative to the patient’s spine? What if it’s not?
Should be to the LEFT of the spine
If not, then suspect malrotation


