Lecture 4: Thyroid Gland Flashcards
What are the 3 stimulatory factors for the secretion of thyroid hormones?
1) TSH
2) Thyroid-stimulating immunoglobulins
3) Increased TBG levels (i.e., pregnancy)
What effect do Perchlorate and Thiocynate have on thyroid hormones?
Inhibit the Na+/I- cotransporter

What is the functional unit of the thyroid gland; surrounded by; how can the cells change?
- Thyroid follicle
- Surrounded by single-layer of epithelial cells
- Follicular lumen filled w/ colloid
- Size of epithelial cells and amount of colloid change w/ activity
How does a single dose of thyroxine (T4) affect BMR?
Increases BMR after several hours and the effect is long-lasting >6 hrs

What levels of TBG and T3 resin uptake in a patient who is pregnant vs. hepatic failure?

What does PTU inhibit and what is it used to treat?
- Effective tx for hyperthyroidism
- Inhibits peroxidase, so it has multiple layers of inhibition
- Inhibits production of final thyroid products

What are the actions of thyroid hormones on CHO metabolism?
- Increased gluconeogenesis and glycogenolysis to generate free glucose
- Enhancement of insulin-dependent entry of glucose = increased glucose absorption
How are thyroid hormones transported in the blood stream?
Either bound to plasma proteins (99%) or free (1%)
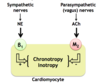
What proteins are synthezised under the direction of thyroid hormones specific to the cardiac muscle cells?
- Myosin
- B1-adrenergic receptors
- Ca+ ATPase

What is the second messenger for TSH?
cAMP

Most circulating thyroid hormons are found in what form; what is the half-life of T4 vs. T3?
- Most found as T4
- T4 half-life is 6 days
- T3 half-life is 1 day
Enough hormone is stored as iodinated TG in the follicular colloid to last the body for how long?
2-3 months!

What levels of T4 and T3 resin uptake in a patient w/ high TBG vs. low TBG?

Explain the T3 resin uptake test
- Standard amount of radioactive T3 is added to a sample that contains a pt’s serum + the T3-binding resin
- Rationale is radioactive T3 will first bind to unoccupied sites on the patients TBG and any “leftover” radioactive T3 will bind to the resin
- T3 resin uptake is increased when circulating levels of TBG are decreased (i.e hepatic failure) or when endogenous T3 levels are increased
- T3 resin uptake is decreased when circulating levels of TBG are increased (i.e., pregnancy) or when endogenous T3 levels are decreased

A deficiency of intrathyroidal deiodinase mimics?
Dietary I- deficiency
What function do thyroid hormone play a role in CNS development; what can a deficiency lead to in a newborn/neonate?
- Important for CNS maturation
- Deficiency during perinatal period leads to:
- Abnormal development of synapses
- Decreased dendritic branching and myelination
- Neural changes induced by thyroid hormone deficiency during the perinatal period are irreversible and lead to Cretinism unless replacemet therapy is started soon after birth
How does hyperthyroidism vs hypothyroidism affect BMR?
Hyperthyroidism: leads to a high BMR
Hypothyroidism: leads to a low BMR

Thyroid hormones contain a large amount of which mineral; where does synthesis of thyroid hormones occur; what is the major secretory product?
- Large amount of iodine
- Synthesis occurs part intracellulary and part extracellularly
- T4 is the major secretory product
What occurs once iodine is in the lumen to join up with thyroglobulin?
- Iodine goes through the process of organification mediated by peroxidase and is joined w/ thyroglobulin
- Thyroglobulin binds to T4, T3, and intermediates MIT/DIT which has now formed the storage molecule within the colloid
How can circulating levels of TBG be indirectly assessed?
T3 resin uptake test
How do we get the thyroglobulin necessary for organification of iodine in the follicular lumen?
- Thyroglobulins are synthesized in the ribosome from the pre-cursor tyrosine, intracellularly. They are processed in the rough ER and golgi before being secreted into the lumen.

What is the main role of TBG?
Provide a large reservoir of circulating thyroid hormones, which can be released and added to the pool of free hormone
What are the actions of thyroid hormones on lipid metabolism; specifically fat mobilization, oxidation of FA, cholesterol/TAG concentration, and fat-soluble vitamins?
- Stimulate fat mobilization –> increases concentration of FA in plasma
- Enhance oxidation of FA
- Plasma concentration of cholesterol and TAGs are inversely correlated w/ thyroid hormones (i.e., hypothyroidism = increased blood cholesterol)
- Required for the conversion of carotene to vitamin A (hypothyroid patients can suffer from blindness and yellowing of skin)
How do high thyroid hormone levels play a role in β1-adrenergic receptors and sympathetic stimulation?
When thryoid levels are high, the myocardium has an increased number of β1 receptors and is more sensitive to stimulation by the sympathetic nervous system