Lecture 11: The Adrenal Gland Flashcards
(71 cards)
What are the embryological orgins of the adrenal cortex and medulla?
Adrenal cortex = epidermal origin
Adrenal medulla = ectodermal origin
Adrenal cortex releases what classes of hormones?
Corticoids and androgens
Adrenal medulla releases what class of hormones?
Catecholamines
What is released by the Zona glomerulosa, fasciculata, reticularis and adrenal medulla?
Zona Glomerulosa: Minearlocorticoid (aldosterone)
Zona Fasciculata: Glucocorticoids (cortisol)
Zona Reticularis: Androgens
Adrenal Medulla: Catecholamines (E and NE)

What are the 3 kinds of hormones produced in the adrenal cortex?
- Glucocorticoids - Cortisol
- Mineralocorticoids - Aldosterone
- Sex steoids - DHEA and DHEAS
Most common adrenal enzyme deficiency and what hormone levels are affected; how do we treat?
- 21 Hydroxylase deficiency
- Decreased cortisol
- Decreased mineralocorticoid
- Increased sex hormones
- Treatment involves replacing glucocorticoids and mineralocorticoids
What are the signs and symptoms of 21-hydroxylase deficiency?
- Hypotension (decreased aldosterone)
- Sodium and volume loss
- Hyperkalemia
- Elevated renin
- Female: virilization of fetus and sexual ambiguity at birth
- Male: phenotypically normal, precocious pseudo-puberty, premature epiphyseal plate closure
What is seen in 11β-Hydroxylase deficiency?
- Increased androgens
- Virilization of female fetuses
- Increased 11-deoxycorticosterone
Signs and symptoms of 11 β-Hydroxylase deficiency?
- Hypertension
- Hypokalemia
- Suppressed renin secretion
What is seen in 17 α-Hydroxylase deficiency; when are these patients diagnosed?
- Decreased androgens and cortisol
- Excess mineralocorticoids
- Patients diagnosed at time of puberty
What are the signs and symptoms of 17-α-Hydroxylase deficiency?
- Hypertension
- Hypokalemia
- Hypogonadism
- Males: undescended tests
- Females: lack of secondary sexual development
What are the target tissues of Cortisol; what 2 ways can it act?
- Tissues throughout the body
- Glucocorticoid Response Element (GRE)
- Non-genomic actions (endocannabinoids)

What are some of the effects of cortisol on the liver, muscle, fat, cutaneous, immune system, endocrine, and GI?
Liver: increased gluconeogensis
Muscle: breakdown of muscle protein
Fat: promote lipolysis in extremities, central fat deposition
Cutaneous: skin thins, fragile blood vessels
Immune system = immune suppression
Endocrine = insulin resistance or glucose intolerance
GI = interferes w/ calcium absorption (risk of osteporosis)
How is cortisol regulated?
- Begins w/ CRF (CRH) in hypothalamus released from PVN
- Binds CRF1 receptor (GPCR)
- Sitmulates release of ACTH from anterior pituitary

What are some things that can stimulate the release of CRH from the hypothalamus?
- Low cortisol
- Stressors (hypoglycemia, hypotensions, fever, trauma, surgery)
What is the principle hormone that stimulates the adrenal glucocorticoids; derived from and produced where?
- ACTH
- Derived from POMC
- Contains MSH (melanocyte stimulating hormone) activity

What does excess ACTH commonly lead to?
Hyperpigmentation due to its MSH activity

What is the long loop, short loop, and ultrashort loop as it pertains to CRH activity and feedback?
Long loop: cortisol from adrenal gland inhibiting release of CRH from hypothalamus
Short loop: ACTH from anterior pituitary inhibiting CRH release from hypothalamus
Ultrashort: CRH activity in hypothalamus inhibiting CRH release

What is the rhythm of ACTH and cortisol release like; when do we see peaks?
- Cortisol levels are highest around 8am, and then gradually trail off for rest of day, peak again around 2pm and then 7pm, low in the late evening
- ACTH levels will peak just before this since it’s needed to stimulate production of cortisol

Discuss the negative feedback by glucocorticoids onto CRH and ACTH?
- GC’s inhbit POMC transcription
- GC’s inhbit mRNA synthesis of CRH and ACTH

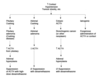
What is the Dexamethasone suppression test (DST); discuss findings at low and high doses?
-
Low dose DST (cortisol analog)
- Determines if there is problem
- Usually overnight
- Pt is administered a supraphysiologic dose
- Normal response: suppression of ACTH and cortisol secretion
- Cushing: no suppression
2. High dose DST (cortisol analog)
- Helps determine the source of the problem (pituitary vs. adrenal Cushing)
What is the Cosyntropin and how is it used; describe the test?
- Synthetic ACTH used in stimulation test (CST) for adrenal gland insufficiency
- *Step 1:** Administer Cosyntropin (ACTH)
- In healthy individuals, cortisol should increase from baseline
- If adrenals unresponsive and cortisol remains the same or rises only small amount, consider adrenal insufficiency
- If adrenals respond dramatically and cortisol increases substantially, consider secondary adrenal insufficiency
What is Cushing Syndrome?
- Hypersecretion of Cortisol
- Usually an adrenal neoplasm
- Elevated cortisol but low ACTH
- An adrenal problem (primary endocrine disorder)

What is Cushing Disease?
- Hypersecretion of ACTH
- Usually a pituitary gland tumor
- Overstimulates the adrenal cortex and excess cortisol secreted
- High serum ACTH and high cortisol
- A pituitary problem (secondary endocrine disorder)





































