Kidney Cysts- MJ Flashcards
T/F: you can get renal cyst development in the following ways:
- Genetic and non-genetic processes (autosomal dominant PKD)
- Variety of childhood and adult diseases (Acquired renal cysts 2° to chronic renal failure)
True
What are the 5 ways renal cysts are categorized?
- Size
- Location
- Spetations
- Calcifications
- Contents
- Enhancement
65-70% of renal masses are what?
simple renal cyst
Simple renal cysts are frequently observed in normal kidneys. What age group is it least common to see these in and what group is it most common?
- Least common: 15 to 29 years – 0% males & 0% females
- Most common: >70 years – 32% males & 15% females
T/F: Simple renal cysts are the most common incidental finding
True
T/F: a patient that is found to have a simple renal cyst has a much higher risk of HTN, CA, CKD or ESRD
FALSE
Simple renal cysts have little clinical significance
Where do simple renal cysts develop?
Are they usually solitary or multiple?
Unilateral or bilateral?
- Develop In the cortex of the medulla
- Can be solitary or multiple, unilateral or bilateral- varies greatly in size and shape
- Is obstruction, rupture, infection (renal abscess) and HTN caused by a simple renal cyst common or rare?
- What would be the sxs of rupture of infection?
Rare
- Sxs:
- Rupture= flank pain, hematuria
- Infection= fever, vague lumbo-abdominal pain, +/- hematuria/pyuria
What is the main goal for evaluating someone with a simple renal cyst? What is the first line diagnostic study for this?
- Goal is to distinguish simple cysts from complex cysts
- U/S is first line
What are the 3 ultrasound criteria for simple cysts?
- Sharply demarcated w/ smooth thin walls
- No echoes (anechoic) within the mass
- Enhanced back wall indicating good transmission through the cyst
What are the 5 ultrasound characteristics of complex cysts?
- Thick walls and/or septations
- Calcifications
- Solid components
- Mixed echogenicity
- Vascularity
Evaluation of Simple Renal Cyst:
If US is equivical or is consistent w/ complex cyst, what diagnostic study should be ordered next?
CT w/ and w/o contrast
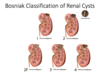
Bosniak Classification of Renal Cysts: Which category?
- CT features:
- sharply demarcated w/ smooth thin wall
- homogenous fluid
- no contrast enhancement
- Significance:
- Simple cyst
- benign
- image in 6-12 mo
Category I

Bosniak Classification of Renal Cysts: Which category?
- CT features:
- Closely resemble simple cysts
- Few thin septa
- +/- few calcifications
- < 3cm
- well marginated
- No enhancement
- Significance:
- Complex cyst
- benign
- image in 6-12mo
Category II

Bosniak Classification of Renal Cysts: Which category?
- CT features:
- Multiple thin septa
- Walls may be thickened and may contain calcifications
- > 3cm
- Significance
- Complex cyst
- likely benign (5% malignant)
- repeat imaging in 3-6mo
Category IIF

Bosniak Classification of Renal Cysts: Which category?
- CT Features:
- Indeterminate cystic masses
- Thickened irregular walls or septa
- measurable enhancement
- Significance
- complex cyst
- 40-60% are malignant
- monitor or excise
Category III

Bosniak Classification of Renal Cysts: Which category? What is the significance of this type of cyst?
- CT features:
- Indeterminate cystic masses
- thickened irregular walls or septa
- measurable enhancement
- Soft-tissue enhancing
- complonents adjacent to cyst wall
Category IV
significance: Complex cyst, 85-100% are malignant
What are the two major causes of acquired renal cysts? Which one is most common?
- Chronic Renal Failure (MC)
- Dialysis (incidence increases w/ duration)
What is the diagnostic criteria for acquired renal cysts? (3)
- Bilateral involvement
- > 4 cysts
- Diameter rangin from <0.5cm up to 2-3cm
In patients with acquired renal cysts, what size are the kidneys typically?
small to normal in size
Acquired Renal Cysts:
Are patients usually symptomatic or asymptomatic?
What is the clinical significance of these cysts?
- Rarely symptomatic
- Clinical significance= may increase RCC risk
When should you consider screening patients for acquired renal cysts? What should you screen with?
- Yearly screening after being on dialysis for 3-5 years
- US vs CT w/ and w/o contrast (depending on what initial study shows)
What is the treatment for simple/complex renal cysts?
- Excision based on Bosniak Classification (usually not excised b/c benign)
- Acetaminophen or NSAID (if nml kidney funct) if having acute/intermittent pain
Simple/complex renal cysts:
How do you treat a patient with persistent pain and cysts > 5 cm?
- Percutaneous aspiration w/ injection of sclerosing agent
- Laparoscopic unroofing
T/F: Autosomal Dominant Polycystic Kidney Disease (ADPKD) is often clinically silent
True
What are the two genetic mutations that can cause ADPKD? Which one is more common and more aggressive?
PKD1 mutation- MC, more aggressive form
PKD2 mutation- Slow growth
Is PKD inherited? If so, is it autosomal dominant or recessive?
- FHx present in 75% of cases (5% due to spontaneous mutation)
- Autosomal Dominant
What does ADPKD cause?
Irreversible decline in renal function which begins in 4th decade
ADPKD:
- 50% of patients will have ESRD by age ____
- Accounts for 10% of ______ patients in US
- 50% of patients will have ESRD by age 60
- Accounts for 10% of Dialysis patients in US
What is the etiology of ADPKD?
PKD1/2 gene mutation → obstructed tubules → cyst formation (multiple w/ bilateral involvement) → fluid accumulation → significant kidney enlargement → separate from nephron → compress neighboring renal parenchyma → progressive compromise renal function (GFR)
What is the initial presentation of ADPKD and at what age?
- Age: 30s-40s
- Presentation: abdominal/flank/back/chest pain
- 50% will also have HTN
What will be found on physical exam of a person with ADPKD?
- 50% have HTN
- Large palpable kidneys
If you have a patient who comes in with a combination of HTN and abdominal mass, what is this indicative of?
ADPKD
What 2 recurrent sxs can be an early indicator of ADPKD but is often overlooked?
Frequent UTIs
Recurrent nephrolithiasis
What abx should a pt w/ ADPKD be receiving if they have a UTI?
quinolones
_____% of patients with ADPKD have HTN by time of ESRD?
100%
What is the clinical presentation of ADPKD? (4)
- HTN
- Pain (vague w/ dull ache or localized w/ sharp pain)
- Hematuria (usually microscopic, gross suggestshemorrhage)
- Proteinuria (initially mild)
What are the 5 diagnostic studies of ADPKD?
- US for screening and monitoring
- CBC
- CMP
- UA
- Genetic Screening
What are 5 associated manifestations of ADPKD?
•Hepatic cysts 40 – 50% (estrogen sensitive)
- Pancreatic/splenic cysts
- Cerebral aneurysms 10 – 15%
•Mitral valve prolapse – up to 25%
•Colonic diverticula are more common
How do you treat ADPKD?
- No tx to halt disease progression or induce regression
- HTN–> ACE/ARB, low Na diet/limit caffeine
- Pain management
- Avoid potentially nephrotoxic agents
- Avoid contact sports
- Manage complications (Infection, cyst hemorrhage, kidney stones)
How do you tx ESRD caused by ADPKD?
Dialysis or kidney transplant
Which disorder?
- Congenital disorder- most sporadic w/o FHx but there is a rare autosomal dominant form
- Asymptomatic
- Found incidentally
Medullary Sponge Kidney
What 2 things is Medullary Sponge Kidney characterized by?
-
Dilation of collecting tubules
- 1 or more renal papillae
- 1 or both kidneys
- Medullary cysts of variable size
What are the 5 complications of Medullary Sponge Kidney?
•Nephrolithiasis
•UTI
•Hematuria
•Decreased urinary concentrating ability
•Renal insufficiency is rare
“DR. HUN”
When is Medullary Sponge Kidney often diagnosed? How is it diagnosed?
- 4th or 5th decade
- Diagnosis
- Intravenous pyelography (IVP)
- Multidetector-row CT

What do you see on Intravenous pyelography (IVP) in a patient with Medullary Sponge Kidney?
•“Brush” or linear striations, radiating outward from calyces
How do you treat Medullary Sponge Kidney?
- No known tx
- Good hydration
- Thiazide diuretic if hypercalciuria present
- Abx for UTI
What is the prognosis of Medullary Sponge Kidney? Is renal function typically maintained or not?
- Excellent long-term prognosis
- Renal function is typically well maintained (recurrent UTI/nephrolithiasis can lead to decline)
How is Medullary Cystic Disease (Nephronophthisis) inherited?
Autosomal recessive
In Medullary Cystic Disease (Nephronophthisis), progression usually occurs before what age?
20 y/o
T/F: there is an infantile, juvenile and adolescent form of Medullary Cystic Disease (Nephronophthisis)?
True
In Medullary Cystic Disease (Nephronophthisis), what appears after 9 years of age
chronic tubulointerstitial nephritis w/ renal cysts
What are the characteristic findings of Medullary Cystic Disease (Nephronophthisis)? (3)
- Reduced urinary concentrating ability
- Bland urinary sediment
- polyuria
- polydipsia
The following is used to diagnose what disease?
- Suggested by clinical characteristics
- Extrarenal manifestations
- Retinitis pigmentosa
- Confirmed by genetic testing
- Ultrasound
- Normal or slight decrease in kidney size for age
- Increased echogenicity w/ loss of corticomedullary differentiation
Medullary Cystic Disease (Nephronophthisis
What is an extrarenal manifestation of Medullary Cystic Disease (Nephronophthisis?
Retinitis pigmentosa
What is seen on US in Medullary Cystic Disease (Nephronophthisis?
•Normal or slight decrease in kidney size for age
•Increased echogenicity w/ loss of corticomedullary differentiation
What is the tx for Medullary Cystic Disease (Nephronophthisis)?
- No specific treatment
- Supportive care


