GYNO FINAL IMAGES Flashcards
*

Dermoid Tumor
-dermoid mesh

Dermoid Cyst
-tip of the iceburg
Testes
- low level echogenicity
- 7-10 mm diameter
- mediastinum teste and epididymus (not seen until after puberty)
*

Bicornate Uterus
- best seen in trans
- bicornate and didelphys -not associated w/ infertility
- duplicated uterus w/ common cervix
*

Bicornate Uterus
- best seen in trans
- bicornate and didelphys -not associated w/ infertility
- duplicated uterus w/ common cervix

Uterus w/ Fibroids
- fibroid usually has rounded borders
- fibroids are estrogen dependant and grow during pregnancy
- may cause infertility
*

submucosal fibroids
- look how each fibroid interfaces w/ endometrial lining
*

Uterine Polyp
- polyp outlined w/ SIS
- color doppler demonstrating vascular pedicle
*

Uterine Polyp
(on a stalk)

Uterine Synechia
- synechia shows up as linear strands of scar tissue extending from one side of uterus to other

Follicles
- 1st image: follicular phase
- 2nd image: dominant follicle

Polycystic Ovarian Syndrome“string of pearls”
- 12 or more follicles measuring 2-9 mm;
ovarian volume > 10 cm3
- often occurs w/ clinical triad:
- olgiomenorrhea, hirsutism, obesity
- immature follicles continue to produce estrogen and androgen which inhibits pit gland.
- Pit gland produces more LH than FSH –> follicle to remain in arrested state of development- no mature ova released w/ ovulation
- chronic elevation of estrogen


peritoneal inclusion cysts

endometriosis
- most common benign gynecologic disease
- in 10-25% of women w/ gyn disease
- in 40% of women w/ infertility
assess thickness and echogenicity pattern
increased thickness 2-3 mm –> 12-14 mm
- measure long plane
- outer to outer - double layer thickness
- normal pattern - trilaminar
- thin endometrium - < 8mm (in secretory phase)
- -decreased fertility

measuring endometrium

Ovarian Stimulation
- administer clomiphene (Clomid) or gonadotropin (Pergonal) day 3-5 in normal cycle
- enlarges multiple follicles instead of just one dominant follicle
- US monitors # and size of follicles day 8-14 (follicular phase)
- count all follicles > 1cm or 10mm
- optimum follcile size = 15-20 mm
- hCG may be given IM to trigger ovulation w/ retrieval 30-34 hours later

Oocyte retrieval
- oocyte fertilization in dish and incubated for 3 to 5 days before embryo transfer

US guided embryo transfer

Ovarian Hyperstimulation Syndrome
- this is a complication of assisted reproductive technology
- enlarged ovaries, multiple cysts, abd ascites, pleural effusions
- more common w/ PCOS
- mild ovarian enlargement 5- 10 cm

A

interstitial/ cornual
B

isthmus
C

abdominal
D

ampulary
E

fimbrial
F

ovary
G

cornual/ interstitial
H

fornix
I

cervical
J

body of uterus
K

abdominal peritoneum
What is seen inside this double decidual sac sign?

yolk sac



interstitial pregnancy
- endometrial cavity line does not enlcose gestational sac
- absence of surrounding myometrium - pregnancy look like it is at the edge of the right side of uterus
- most life threatening


cervical ectopic pregnancy

abdominal ectopic pregnancy
- pregnancy develops w/in the peritoneal cavity

indications for 1st trimester exam
- Confirmation of IUP vs. EUP
- Define cause of bleeding
- Pelvic Pain
- Viability
- # of embryos
- Gestational age
- Detect anomalies
- R/O hydatidform mole
- Adjunct to CVS, amnio, embryo transfer, IUD removal
- **First trimester exam performed only when deemed necessary**
indications for 2nd & 3rd trimester exam
- Gestational Age
- Fetal Growth
- Vaginal Bleeding
- Abd/Pelvic pain
- Incompetent cervix
- Determine fetal presentation
- # fetuses
- Size discrepance to dates
- Pelvic mass
- Suspected hydatidform mole
- Cervical cerclage placement
- R/O ectopic
- Fetal viability
- Uterine abnormality
- Evaluate fetal well-being
- Amniotic fluid
- Placental abruption
- External cephalic version
- Premature rupture membranes and/or labor
- Abnormal chemical markers
- F/U fetal anomaly
- History prev congenital anomaly
- Eval for late to prenatal care
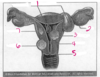
1.

uterine fundus
2

fallopian tube
3

fimbriae
4

myometrium
5

endometrium
6

uterine isthmus
7

lateral fornix
8

vagina
9

ectocervix
10

endocervix
11

ovarian ligament
12

ovary
benign smooth muscle cell tumor; few appear in the cervix

cervical leiomyoma (fibroid)
*

fluid filled uterus

hydrometra
blood filled.

hematometra

1

leiomyoma locations
pedunculated or intracavitary
2
leiomyoma locations

Ovary
3
leiomyoma locations

submucosal
4
leiomyoma locations

uterus
5
leiomyoma locations
cervix
6
leiomyoma locations

subserosal
7
leiomyoma locations

intramural
most common gynecologic tumor of childbearing age women, and is more common in black women?

submucosal leiomyoma (common location)
- fibroid is anterior & is pushing endometrium posterior
- smooth muscle cell tumor
- encapsulated with pseudocapsule
- fibrosis w/ degenerative changes
- out grow their blood supply and atrophy
- estrogen dependant
- pregnancy and tamoxifen = ↑ growth (size)
- menopause w/o HRT = ↓ growth (size)
- Clinical findings: irreg bleeding, menorrhagia, menometrorrhagia, enlarged uterus, infertility, pee alot
- on US: (variable) enlarged uterus w/ irregular wall, bright echoes w/ clcifications & shadowing, discrete mass

very common benign disease of the uterus; infiltration of endometrial tissue from stratum basalis into myometrium?

adenomyosis
- Ectopic endometrial tissue within myometrium
- More common posterior uterus
- Does not bleed with hormone cycle
- Product of multiple pregnancies
- Elevated estrogen levels
hypermenorrhea, menorrhagia, metrorrhea, dysmenorrhea
on US:
- Diffuse uterine enlargement
- Thickening posterior myometrium
- Small myometrial cysts - swiss cheese or honeycomb - non vascular
- Subendometrial cysts
- Myometrial heterogenicity with ill-defined endometrial borders
- May mimic fibroid
- MRI characterizes adenomyosis better

overgrowth of endometrial tissue covered by epithelium containing glands, stroma, blood vessels

uterine polyps
- peri & post menopausal women -more common & associated w/ bleeding
- menstruating women - asociated w/ infertility & menometrorrhagia
- differential: hyperplasia, submucosal leiomyoma, or endometrial cancer
- doppler shows a feeding artery in a pedicle

synechiae
- intrauterine adhesions (Asherman’s Syndrome)
- found after trauma or surgery, uterine curettage
- cause of infertility or pregnancy loss
- better seen in gravid uterus, secretory phase
- adhesion bridging bands of tissue- thin membrane or thick broad based adhesion
- can be divided under hysteroscopy

IUCD in place
small endocrine structure that develops w/in a ruptured ovarian follicle and secretes progesterone and estrogen

corpus luteum cyst

requires 3 things: smooth walls, fluid filled, acoustic enhancement

simple cyst
is usually benign

corpus luteum cyst

ovarian hyperstimulation syndrome (OHSS)
- complication of ovulation induction
-
mild
- pelvic discomfort, ovaries enlarged < 5cm
-
severe
- severe pelvic pain
- distended abd.
- ovaries enlarged >10cm
- ascites, pleural effusions
- w/ treatment - resolves in 2-3 weeks
12 or more follicles measuring 2-9 mm and ovarian volume greater than 10 cm3

polycystic ovarian syndrome (PCOS)
- very common
- “string of pearls”
- stein leventhal syndrome
- infertility, oligomenorrhea, hirsutism & obesity
- bilateral enlarged polycystic ovaries
- common cause of infertility and miscarriage
- diagnosis usually made by hormone levels

endometriosis
- functional endometrial tissue present outside the uterus
- diffuse is more common
- localized = chocolate cyst
- bleeds cyclically


dermoid tumor
tip of the iceberg sign

dermoid cyst
dermoid mesh

hydrosalpinx
fluid in the fallopian tube

1
Blood supply to pelvis

internal iliac artery
2.
Blood supply to pelvis

tubal branch of uterine artery
3.
Blood supply to pelvis

ovarian branch of uterine artery
4.
Blood supply to pelvis

infundibulopelvic ligament
5
Blood supply to pelvis

ureter
6
Blood supply to pelvis

uterine artery
7
Blood supply to pelvis

vaginal artery
8
Blood supply to pelvis

internal pudendal artery
9
Blood supply to pelvis

azygos arteries
10
Blood supply to pelvis

cervical branch of the uterine artery
1
genital tract

uterine (fallopian) tube
2
genital tract

cornu
3
genital tract

fundus
4
genital tract

corpus
5
genital tract

isthmus
6
genital tract

cervix
7
genital tract

rugae of mucosal lining
8
genital tract

adventitia
9
genital tract

muscular wall
10
genital tract

mucosa
11
genital tract

vagina
12
genital tract

external os
13
genital tract

lateral vagina fornix
14
genital tract

internal os
15
genital tract

serosa
16
genital tract

myometrium
17
genital tract

uterine cavity
18
genital tract

endometrium
Uterine Position Variations

1
fallopian tube

mesosalpinx
2
fallopian tube

infundibulum
3
fallopian tube

fimbriae
4
fallopian tube

ovarian ligament
5
fallopian tube

interstitial portion
6
fallopian tube

isthmus
7
fallopian tube

ampulla
what endometrial phase is this “thin line”?

early proliferative
what endometrial phase is this “three line sign”?

classic proliferative
what endometrial phase is this thickened ?

secratory phase
what phase?
what position?

early secretory
retroflexed to the right
what phase?

secratory phase
what flexion?

anteflexed
what flexion?

anteflexed
what flexion?

retroflexed


