First Aid Microbiology 3 Flashcards
Condylomas

The limited list of rashes that may appear on palms of hands and soles of feet

What is this finding on CT angiography? (It has a correlate on gross pathology)
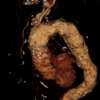
Tree bark aorta
Named for its appearance. This is a characteristic of tertiary syphilis, and is a form of ascending thoracic aortic aneurysm.
The pathology is due to invasion of the vasa vasorum (vessels of the vessel) that supply the thick muscular walls of the aorta.
What is going on in this infant with the displayed findings?

Congenital syphilis
Characteristic findings: Tooth abnormalities, saddle nose, perioral fissures, congenital deafness, high arched palate, and joint separation in feet and sometimes arms.
Treating syphilis
Always treat w/ penicillin
If Jarisch-Herxheimer reaction evolves, simple supportive care, NSAID analgesia, and potentially benzodiazepine sedation are all that will be necessary – it is self limited.
The two diseases caused by Legionella
Pontiac fever and Legionaire’s Disease
Pontiac fever is an acute, nonfatal respiratory disease. It causes a mild upper respiratory infection that resembles acute influenza. Pontiac fever resolves spontaneously and often goes undiagnosed.
Legionaire’s Disease is a severe pneumonia associated with hyponatremia, diarrhea, and neurologic symptoms that usually occurs in smokers and can spread in epidemic fashion.
Both are treated with fluoroquinolones or macrolides.
Why is pseudomonas SO BAD for CGD patients?
It is encapsalted as well as both catalase positive and oxidase positive
What is going on in this individual’s foot?

This is a not uncommon clinical scenario.
Diabetic neuropathy predisposes diabetic patients to these foot ulcers. These ulcers are then at risk for subsequent infections, and one of the major offenders is Pseudomonas aeruginosa. P. aeruginosa is so bluish-green that it can literally color the wound site, making it apparent that it should be at the top of your differential in cases like this.
P. aeruginosa is also the most common cause of osteomyelitis in diabetic patients.
What is the #1 most common and most feared infection in a burn patient?
Pseudomonas aeruginosa
Patient presents to primary care with the following presentation. They report that they are up to date on their vaccination status and have been quarantining at home. They have been spending much of their time enjoying their home built hot tub which was recently finished.
What is the likely causative organism? How could this have been avoided?

This is hot tub folliculitis
It is caused by Pseudomonas aeruginosa, and is prevented from developing in hot tubs and swimming pools by adding chlorine to the water.
Patient with PMH notable for diabetes presents with subacute hearing loss and painful inflammation of the external ear. The following is observed upon speculum exam.
The most likely causative organism for this patient’s disease shares a toxin with what other deadly bacterium? How does the toxin work?

This patient most likely has Pseudomonas aeruginosa infection of the external ear.
Pseudomonas shares a toxin with Corynebacterium diphtheriae which works by ribosylating EF2 and preventing protein translation in mammalian cells, leading to cell deaths
What can kill Pseudomonas?
Piperacillin (penicillinase-resistant penicillin)
Aminoglycosides
Fluoroquinolones
Patient presents with cellulitis of the forearm following being bitten by their pet dog at this site the previous day. What is the likely causative organism?
Pasteurella multocida (think Pasteur’s pet dog Ella)
Note that this could easily have been a cat too, but it would have to be a bite, not a scratch (like for Bartonella). The organism lives in the respiratory tracts of dogs and cats.
Like Pseudomonas, Pasteurella are catalase positive, oxidase positive, and encapsulated, making them a nightmare for patients with CGD.
It displays bipolar “safety pin” staining. Treat w/ amoxicillin-clavulonate.

On laboratory testing, the bacteria associated with an individual’s sputum sample are found to be lacking a component of peptidoglycan called muramic acid.
What is the likely causative organism for their pneumonia?
Chlamydophila pneumoniae
Lack of muramic acid in the cell wall is a defining characteristic of the chlamydia and chlamydophila species. It also means that they are resistant to penicillins.
So, treat w/ macrolides. If C. trichomatis, then assume N. gonorrheae is also present and give ceftriaxone too.
When dealing with gram intermediate bacteria with complex life cycles, the ___ form is always the infectious form and the ___ form is the noninfectious form which can divide.
When dealing with gram intermediate bacteria with complex life cycles, the elementary form is always the infectious form and the reticulate form is the noninfectious form which can divide.
Reticulate means to divide!
Organisms that stain w/ Giemsa
- Borrelia (Lyme)
- Chlamydia species
- Klebsiella granulomatis (Donovanosis)
- Amoebic parasites:
- Plasmodium species (Malaria)
- Pneumocystis jirovecii
- Babesia species (Babesiosis)
Subgroups of Chlamydia trichomatis and what they cause
- A-C: Blindness
- D-K: STI
- L1-L3: Lymphogranuloma venerium (LGV)
Patient presents w/ genital infection. You suspect a common STI based on the clinical history.
How do the characteristics of the discharge of the wound influence your suspicion of the causative organism?
If the discharge is thick and purulent, it is more likely to be Neisseria gonorrheae
If the discharge is watery, it is more likely to be Chlamydia trichomatis
Note that either way, your treatment regimen will assume that both organisms are present, since they are often co-infectious.
Reiter’s syndrome
Combination of uveitis, urethritis, and reactive arthritis following Chlamydia trichomatis infection.
“Can’t see, can’t pee, can’t climb a tree”
“Walking pneumonia” etiologies
- Mycoplasma
- Legionella
- Chlamydophilum
Patient presents w/ walking pneumonia. Lab results show that it is Chlamydophilum genus.
What in the history might give you a clue as to if this is C. pneumoniae or C. psittaci?
C. pneumoniae tends to occur in elderly individuals
C. psittaci is transmitted by bird droppings, and Hx will often include pet birds or working at a pet store with birds.
Patient with Hx notable for AIDS w/ poor adherence to HAART presents with many blanching red lesions over the trunck and extremities. Rapid testing is negative for HHV8.
What is this patient’s history likely to reveal? What is the appropriate treatment?
With the fact that these lesions blanche and the HHV8 test coming back negative, the likely diagosis is bacillary angiomatosis, the presentation of cat scratch fever in immunodeficient patients.
Hx is likely to reveal scratch by a pet or stray cat. Treat w/ macrolides.
Patient presents w/ fever, night sweats, and anorexia over the past few days. They report that they have had an undulating fever, peaking at 102oF and dropping down to normal several times over the course of the day. Hx is negative for any recent travel or sick contacts, but patient reports that they work as a farm hand and tend to barn animals and occasionally drink fresh unpasteurized milk from the farm. Hepatomegaly and splenomegaly are detected on exam.
What is the likely diagnosis and treatment?
This is likely to be a case of Burucella infection. It may be acquired from handling animal feces or unpasteurized animal products, like milk or soft cheese.
Undulating fever and nonspecific symptoms in someone w/ history of working on a barn is classical for Burucellosis. It may also present with osteomyelitis or culture-negative endocarditis.
Treat w/ a combination of doxycycline and rifampin.
Patient presents with high fever, chills, and anorexia following return from a trip to Martha’s Vineyard two days ago. On exam, they are found to have an ulcer on their left calf and inguinal lymphadenopathy.
Biopsy of an inguinal lymph node is performed and shows caseating necrosis at the center of a large granuloma. Acid fast stain is negative for acid fast bacilli.
What is the likely diagnosis and treatment?
Ruling out atypical mycobacterial infection, the most likely cause for this patient’s illness is Francisella tularensis. This patient has ulcero-nodular tularemia.
This is especially common in Martha’s Vineyard due to the importing of rabbits from areas where F. tularensis is endemic in the south, and MV is a hot-spot for tularemia in Massachusetts, with most of the MA cases coming from there every year.
Of note, tularemia also causes caseating granulomatous inflammation, just like TB and atypical mycobacteria.
Patient presents with fever, nausea, and greenish, lumpy, “pea soup”-looking stools, as well as a diffuse rash shown below. Murphy’s sign was present on exam.
Biopsy and culture of fluid from the gall bladder is likely to grow what organism? How would you treat?

This is classic typhoid fever, characteristic of Salmonella typhi infection.
S. typhi colonizes the gall baldders of infected individuals, who may acquire the bacteria from contaminated water or undercooked seafood, and causes chronic mild cholecystitis as well as episodes of acute typhoid fever with “rose spot” rash, B symptoms, and “pea soup” stools.
Treat w/ fluoroquinolones.
Fever patterns and malaria species

If someone presents with malaria following appropriate chloroquine prophylaxis, it is likely to be. . .
P. falciparum
P. falciparum is chloroquine resistant, unlike other plasmodium species!
Atovaquone-proguanil is an effective prophylaxis for P. falciparum
Patient presents with pneumonia following aspiration. CXR shows cavitating lesion. What is the likely etiology? How should you treat?
Cavitating pneumonias resulting from aspiration are most commonly caused by the oral anerobes: Peptostreptococci, Prevotella species, Bacteroides species, and Fusobacterium species
These guys usually require Clindamycin
Why is the vector for T. cruzi called the “Kissing bug”?
Because it likes to bite around the victim’s mouth while they are asleep at night.
It leaves faeces infected with T. cruzi in the wound, and they are pushed further in when the victim inevitably scrathces the bitten area. After a LONG time, often two or more decades, Chagas disease will start to set in.
The kissing bug is native to South and Central America, but is slowly making its way North with climate change.

Chagas disease syndrome
- Megacolon (often w/ constipation)
- Dilated cardiomyopathy
- Mega-esophagus
Chagas makes things BIG
How is Chagas disease diagnosed?
With active disease: Blood smear! T. cruzi can be easily visualized as these wispy fellows during an active infection.
With chronic disease: Serology and clinical symptoms are sufficient

What is going on in this endocardial biopsy?

Chagas cardiomyopathy
The lesion shown is a T. cruzi burrow. This patient is likely presenting with symptoms of heart failure due to dilated cardiomyopathy.
The only current treatment for active Chagas disease
Nifurtimox
“Knee high fur socks?”
There is no treatment for the chronic form of the disease.
Patient presents with pneumonia, headache, and persistent high fever for the past few days. No rashes are noted on physical exam. The patient works as a farmer and has a barn with livestock. He notes that he recently did a major cleaning of the barn and wonders if he kicked something up in the dust.
On initial workup it is noted that his liver enzymes are also elevated.
What is the differential for this patient? What is the most likely diagnosis? How should they be treated?
The major two diagnoses to consider for this patient are 1) Burucella and 2) Coxiella. Both are commonly acquired from barnyard animals and can present similarly with fever and elevated liver enzymes. However, a hallmark feature of Burucella is the undulating fever. This patient has a persistent high fever, making Coxiella the more likely pathogen, making the diagnosis Q fever (remember Curly Q the Ram).
The infection is self-limited and goes away within 2 weeks. However, patients with valve damage may develop a culture-negative endocarditis. For these complicated cases, dual therapy with hydroxychloroquine and doxycycline is standard.
Relevance of Lactobacilli to G. vaginalis infection
Lactobacilli make up the majority of the normal vaginal flora in healthy individuals.
When the microbiome is pertubed and Lactobacilli take up less space in the biome, that is when individuals are susceptible to G. vaginalis infection.
Female patient presents with grayish-white, malodorous discharge from the vaginal canal. Litmus testing shows pH of 6.5.
You suspect a paritcular diagnosis, and so you do a wet mount of exudate and see the following.
What is the diagnosis? How should you treat?

The image shows “clue cells,” shed epithelial cells from the vaginal vault covered in bacteria.
This confirms the diagnosis of bacterial vaginosis, caused by Gardnerella vaginalis.
Treat w/ metronidazole.
The only bacterial family with cholesterol in the cell membrane
Mycoplasma
Makes sense if you think about it – they have no cell wall, so they need something to provide structure, and it happens to be the same thing that eukaryotes use.
Patient presents for X-ray for possible costochondritis and is found incidentally to have diffuse, patchy lung infiltrate. When asked about pneumonia symptoms, the patient responds that they have had a slight cough and feel a bit low on energy, but aren’t in any distress and feel reasonably well.
What is the likely causative organism? How could you confirm this?
Mycoplasma
This is a typical walking pneumonia. X-ray findings are out-of-proportion to the minor presentation of the illness. Most commonly presents in young adults in close contact, such as college dorms or military recruits.
Mycoplasma is difficult to culture and takes a long time. A more reasonable test is the cold agglutination test. Patients w/ Mycoplasma pneumonia tend to have IgM which binds to erythrocytes at cold temperatures (~4 C).
Treat w/ macrolides.
You are on a trip to West Africa. One day following a hike, someone on your tour group begins to feel unwell. They become somnolent and develop recurring fever, as well as prominent axillary and cervical lymphadenopathy. You suspect a certain diagnosis and rush to the hospital to obtain a blood smear, shown below.
What is the diagnosis and how was it acquired? Why does it cause mulitple recurrent fevers? How should you treat?

This is African Sleeping Sickness, caused by Trypanosoma brucei subspecies. It is endemic to Western and Southern Africa, and utilizes the Tsetse fly as a vector.
As the name implies, it causes coma, as well as recurrent fever and lymphadenopathy. The recurrent fever is due to antigen rotation by the protazoa.
Treatment is with Melarsoprol for CNS infection and Suramin for blood infection. Both are usually required, as the infection is usually in both locations.
Patient presents with necrotizing fasciitis. Testing for Group A strep is negative, and instead shows a gram negative organism. What is the likely etiology?
Clostridium perfringens
A notable cause of gram negative necrotizing fasciitis.
“Gas gangrene” is characteristic of ____.
What mediates its pathology? How do you treat?
Clostridium perfringens
Secrete an alpha toxin that cleaves phospholipids, damaging cell membranes, including of red cells (hemolysis). This toxin characteristically produces a double-zone of hemolysis on blood agar.
Treat w/ penicillin G

Clostridial diarrhea
Also caused by Clostridium perfringens, the cause of gas gangrene.
Unlike most spore-associated diarrhea, it is caused by the spores themselves rather than re-activating spores, and has a much slower onset.
Why are ricketsia species obligate intracellular?
They cannot produce their own nicotinamide or CoA
The Weil-Felix test
- Test used to distinguish ricketsia from other organisms and between ricketsial species
- Based on the principle that there is cross-reactivity between Ricketsia and Proteus antigens
- Take a sample of the patient’s blood, add some Proteus antigen, and see if agglutination occurs
- Not used much anymore – low sensitivity and specificity
Patient is treated for lice with a course of permethrin shampoo applied daily and picking of lice with help from a caregiver.
Toward the end of their course, they develop a truncal rash which spreads outward across the body, but spares the hands, feet, and head. They developed myalgia, arthralgia, and pneumonia.
What is the causative organism? How should you treat?
This is a classic Ricketsia prowazekii infection, called epidemic typhus, spread by the common louse.
Disease may still progress from here to encephalitis.
Treat w/ doxycycline.
Patient presents with high fever and purpuric rash on the head, hands, and feet. He notes that the rash started on extremities and has been slowly progressing towards his core. Also notes headache and myalgias. History includes recent hiking trip in western Massachusetts.
What is the most likely diagnosis? How was the disease acquired? What is the treatment?
Rocky Mountain Spotted Fever, caused by Ricketsia ricketsii and spread by the dermatocentor tick
Treat w/ doxycycline


