Exam 2: Renal, Lower Urinary, and Prostate Cancer DSA Flashcards
1
Q
List some benign and malignant renal tumors
A
-
Benign tumors of the kidney including
- oncocytoma
- angiomyolipoma
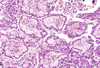
- renal papillary adenoma
-
Malignant tumors of the kidney including
- renal cell carcinoma
- clear cell
- papillary
- chromophobe
- Wilms tumor (nephroblastoma)
- urothelial carcinomas of the renal pelvis
- renal cell carcinoma
2
Q
Tumor type?
Key info?

A
-
Oncocytoma
- Arise from intercalated cells of collecting ducts
- ~10% (5-15%) of renal tumors.
-
Pathogenesis
- associated with genetic changes
- loss of chromosomes 1, 14, and 7.
-
Gross
- Large size
- tan-brown to mahogany color
- central stellate scar.
- Can be multiple with familiar cases.
-
Microscopic
- Abundant mitochondria in finely granular cytoplasm.
3
Q
type of tumor?

A
- Oncocytoma
- Note the central scar (gross) and the tumor cells (microscopic) with the eosinophilic, finely granular cytoplasm.
- (a)
- circumscribed tumour with central area of scarring
- (b)
- conglomerate islands of cells separated by a pale-staining myxoid stroma
4
Q
type of tumor?

A
- Oncocytoma
- Note this EM of oncocytoma shows abundant mitochondria, a characteristic finding.
- Electron microscopic
- The cytoplasm of the tumor cells is characteristically filled with mitochondria, many of which have stacked cristae.
5
Q
Tumor type?
Key info?

A
-
Angiomyolipoma
- Benign
-
Composed of
- blood vessels
- smooth muscle, spindle cells
- adipose tissue from perivascular epithelioid cells.
-
Occurs in 25-50% patients with tuberous sclerosis
-
TS
- hamartomatous lesions of brain (“tubers”)
- skin abnormalities
- benign tumors of heart and other organs
-
Loss-of-function mutations
- in TSC1 or TSC2 tumor suppressor genes
-
TS
- Susceptible to spontaneous hemorrhage
6
Q
Renal Cell Papillary Adenoma
Key info?
A
-
Renal Cell Papillary Adenoma
- Common finding at autopsy
-
Frequently papillary.
- clear cell and chromophobe lesions should not be termed adenomas.
-
Gross
- small (usually <0.5 cm) cortical lesions
- pale, yellow, well-circumscribed
-
Microscopic
- Indistinguishable from low-grade papillary renal cell carcinoma
- Cuboidal or low columnar cells in papillary formations
-
Natural history
- consider as potentially malignant.
7
Q
Renal Cell Carcinoma
Key info?
A
-
Renal Cell Carcinoma
-
Malignant Tumor
- Can metastasize and invade.
-
Malignant Tumor
-
Most common primary cancer of the kidney (85%)
- Occurs in 6th to 7th decade
- and males > females (3:1)
-
Etiology/Risk factor
- Tobacco is most significant.
- Obesity
- HTN
- unopposed estrogen therapy
-
toxic/industrial exposures
- including cadmium and heavy metals, asbestos, petroleum products.
-
Genetics
-
Von Hippel-Landau (VHL) gene
- familial and sporadic clear cell tumors
-
MET proto-oncogene
- hereditary papillary tumors
-
Chromophobe carcinoma
- multiple chromosome losses and extreme hypodiploidy
- Others
-
Von Hippel-Landau (VHL) gene
8
Q
Tumor type?
Key info?

A
Renal Cell Carcinoma – Clear Cell Carcinoma
- Most common type
-
Morphology
- clear cytoplasm and non-papillary
- Can be hereditary/familial, but vast majority are sporadic.
-
Von Hippel-Lindau syndrome
- includes cerebellar hemangioblastoma, retinal angiomas, cysts in pancreas/liver/kidney, and pheochromocytomas in addition to renal cell carcinoma.
-
Familial cases involve loss of inherited 3p (3p25.3) with VHL gene.
- Other genes are inactivated by somatic mutation or hypermethylation. Lack of VHL protein stabilizes hypoxia-inducible factor (HIF-1). HIF-1 activates genes such as VEGF (angiogenesis), MYC complex; epigenetic processes are also affected.
-
Von Hippel-Lindau syndrome
-
Gross
- Usually unilateral and solitary
- bright yellow-grey white , cortical, sharply-defined.
- Invasion of renal vein can occur.
-
Microscopic
- Clear/granular cytoplasm containing glycogen and lipids.
- Cystic and solid areas may be seen.
- Wide range of atypicality.
9
Q
Tumor type?
Key info?
A
Renal Cell Carcinoma – Papillary Carcinoma
- 10-15% of renal cell cancers
- Tumors are frequently multifocal (more than clear cell)
- Better prognosis than clear cell
- Familial and Sporadic forms
- Not associated with 3p deletions
- Most common
- Trisomies 7 and 17 and loss of Y chromosome in males.
- Chromosome 7 has MET gene
- a proto-oncogene that codes the tyrosine kinase receptor for hepatocyte growth factor, which influences growth, cell mobility and morphogenetic differentiation.
-
Gross
- frequently multifocal
- hemorrhagic
- and cystic
-
Microscopic
- cuboidal or low columnar cells
- arranged in papillary formations.
- Foamy macrophages (interstitial foam cells) are present throughout the tumor.
10
Q
Tumor type?
Key info?

A
Renal Cell Carcinoma – Chromophobe Renal Carcinoma
- 5% of renal cell cancers
-
Cytogenetic
- multiple chromosome losses and extreme hypodiploidy
- Thought to arise form intercalated cells of collecting ducts.
- Excellent prognosis (vs. clear cell and papillary)
- Hereditary forms occur
-
Birt-Hogg-Dube (BHD) syndrome
- a hereditary disease with risk for bilateral, multifocal chromophobe RCC
- is caused by mutations in folliculin.
- This features skin, pulmonary, and renal tumors with a wide variety of histologic subtypes. Hereditary forms are more apt to be bilateral.
-
Birt-Hogg-Dube (BHD) syndrome
-
Gross
- frequently multifocal
- hemorrhagic
- and cystic
-
Microscopic
- Pale eosinophilic cells that often have halos around nuclei.
- Tumor cells are arranged in solid sheets with a concentration of the largest cells around blood vessels.
11
Q
Urothelial Tumors
A
- 5-10% of primary renal tumors
- benign papillomas to malignant urothelial carcinomas.
- Similar tumors also occur in the ureters and urinary bladder.
- These were known in the past as transitional cell carcinomas.
- Ureter and bladder tumors become clinically apparent early
- due to hematuria.
- They may also block the urinary outflow
- and result in hydronephrosis.
-
Pathogenesis/Risk factors for urothelial tumors include
- cigarette smoking (most important)
- exposure to aryl amines
- schistosomiasis (squamous carcinoma)
- long-term analgesic or cyclophosphamide use,
- chronic inflammation
- and irradiation.
- Heavy caffeine use may be associated with a small increase in incidence.
-
Acquired genetic alterations include
- one pathway with mutations in
-
gain-of-function FGFR3 and RAS
- low-grade lesions
-
loss-of-function p53 and RB
- in progression to high-grade lesions.
-
gain-of-function FGFR3 and RAS
- Another more aggressive pathway includes p53 and loss of chromosome 9 and acquisition of other genetic abnormalities.
- one pathway with mutations in
12
Q
Urothelial Carcinoma - Bladder
A
- In bladder, men > women.
- Lesions can be papillary
- with noninvasive papillomas progressing to invasive papillary carcinoma.
- Lesion can also be flat (carcinoma in situ)
- with progression to flat invasive carcinoma
-
Other types of carcinoma may occur.
-
Squamous
- Schistosomiasis
-
Adenocarcinoma
- Urachal remnants or with extensive intestinal metaplasia
- Small cell carcinoma
-
Squamous
- Prognosis depends on grading and staging
- Recurrence, progression, and mortality are higher with higher grade and stage.
13
Q
Type of tumor?

A
Urothelial Carcinoma - Bladder
-
Image A - Papilloma
- consisting of small papillary fronds lined by normal-appearing urothelium
-
Image B - Low-grade papillary urothelial carcinoma
- with an overall orderly appearance
- with a thicker lining than papilloma
- and scattered hyperchromatic nuclei and mitotic figures (arrows).
-
Image C - High-grade papillary urothelial carcinoma
- with marked cytologic atypia.
-
Image D - High-grade invasive transitional cell carcinoma
- at an advanced stage.
- The aggressive multinodular neoplasm has fungated into the bladder lumen and spread over a wide area.
- The yellow areas represent areas of ulceration and necrosis.
-
Image E - Flat carcinoma in situ
- with numerous cells having enlarged and pleomorphic nuclei.

14
Q
Urothelial Carcinoma - Bladder
Treatment?
A
-
BCG instillation into bladder
- for patients at high risk for recurrence or progression
-
Transurethral resection
- of small, low-grade, papillary tumors
-
Radical cystectomy
- for invasive, high-grade lesions
- or lesions resistant to BCG
- and those tumors extending into urethral/prostatic ducts
-
Chemotherapy
- for metastatic
15
Q
Wilms Tumor / Nephroblastoma
A
- Tumor of embryonal renal elements
-
Most common primary tumor in children
- peak incidence between 2 and 5 years.
- Usually prior to 10 years of age.
-
Most are unilateral.
- 5-10% are bilateral
- either simultaneously (synchronous)
- or sequentially (metachronous).
- Bilateral tumors occur earlier and suggest germline mutations.
- 5-10% are bilateral
- Pathogenesis
- Most are sporadic.
-
Increased incidence with 3 groups of congenital abnormalities.
-
WAGR (Wilms tumor, aniridia, genital anomalies, and mental retardation).
- Deletions of 11p13
- First hit is inherited; second hit is necessary.
- WT1 is involved in regulation of other genes (e.g. IGF-II, E-cadherin, PDGF).
- Most also show loss of heterozygosity at another locus on 11p (similar to area involved with BWS; see below.
-
Denys-Drash syndrome
- with gonadal dysgenesis (male pseudohermaphroditism) and early-onset nephropathy (diffuse mesangial sclerosis).
- WT1 mutation affects DNA-biding properties.
-
Tumorgenesis requires bi-allelic inactivation of WT1
- dominant negative inheritance
-
Beckwith-Wiedemann syndrome (BWS)
- has gigantism, organomegaly, macroglossia, hem hypertrophy, omphalocele, and/or abnormal large cells in adrenal cortex.
- Associated with band 11p15.5 but exact gene has not been identified (“WT2”).
- Often associated with imprinting.
-
WAGR (Wilms tumor, aniridia, genital anomalies, and mental retardation).
- Beta-catenin and p53 mutations also occur (e.g. in sporadic cases)
- Nephrogenic rests are putative precursor lesions (i.e. hyperplastic to sclerotic rests)
16
Q
Type of tumor?

A
Wilms Tumor (nephroblastoma)
-
Image A
- Wilms tumor in the lower pole of the kidney with the characteristic tan-to-gray color and well-circumscribed margins
-
Image B
- tightly packed blue cells consistent with the blastemal componen
- and interspersed primitive tubules representing the epithelial component.
-
Image C
- Focal anaplasia was present in other areas
- hyperchromatic cells, pleomorphic nuclei, and abnormal mitoses.
-
Image D
- highly cellular areas composed of undifferentiated blastema (B
- loose stroma (S) containing undifferentiated mesenchymal cells and immature tubules (T).
- Note the many mitotic figures (arrows).
-
Gross
- usually unilateral, large, solitary at presentation
- 10% bilateral or multicentric with higher incidence in familial tumors)
- Soft, homogeneous, tan to gray
- with occasional foci of hemorrhage, cyst formation or necrosis.
-
Micro
- Often undifferentiated and primitive
- Attempt to recapitulate different stages of nephrogenesis
- Blastemal – small blue cells
- Stroma – fibrocytic or myxoid
- Epithelial - abortive tubules
- 5% have anaplasia (with p53 mutations) and chemotherapy resistance



