distal neurovasculature, ankle and foot Flashcards
What forms the superficial venous drainage route from the lower limb?
Where are they located?
What can happen if they are damaged?
where do they drain to?
- The saphenous veins
- Starts in the distal portion of the dorsum of the foot in the dorsal venous arch, they are located superior to the deep fascia in subcuteaeous tissue.
- If they are damaged they can bleed profusely
- They drain into the deep veins:
- short saphenous drains the lateral surface of the leg and enters posterior portion, empties into popliteal vein
- long saphenous vein drains blood from foot, leg and thigh into the femoral vein.
describe and label the superficial venous drainage of the foot and lower leg

- Venous drainage of the foot starts in the dorsal venous arch of the foot which gives off:
- Small/ short saphenous vein
- Great/ long saphenous vein
-
Small saphenous vein –> formed by dorsal venous arch and dorsal vein of little toe.
- Moves up posterior side of the leg passing posteriorly to lateral malleolus
- moves between two heads of gastrocnemius and empties into popliteal vein in popliteal fossa.
-
Great saphenous vein –> formed by dorsal venous arch of the foot and dorsal vein of great toe
- ascends up medial side of leg
- passes anterior to medial malleolus
- moves up leg draining other structures
- drains into femoral vein inferior to inguinal ligament.

What procedure can the long saphenous vein be used for?
- Long saphenous used for coronary artery bypass graft
- can also be used for cut down procedure to insert cannula in a burns victim
What nerves accompany the long/ great saphenous and small/ short saphenous veins?
- Short saphenous vein accompanied by the sural nerve
- Long saphenous vein accompanied by the saphenous nerve
Describe in detail the route of the long saphenous vein
What is the clinical relevance of the saphenous vein?
- Travels from dorsal arch of the foot, travels superiorly passing anterior to the medial malleolus.
- Along the medial tibial border alongside the saphenous nerve
- passes about 4 fingers breadth from the patella
- travels superiorly to drain into the femoral vein around 1-4 cm lateral and 1-3 cm inferior to the pubic tubercle.
- Clinical relevance: saphena varix:
- saphena varix = dilation of the saphenous vein as it joins the femoral vein, can present as a groin swelling.

What is a varicose vein? What is the cause?
What symptoms may a patient present with?
What conditions predispose?
- varicous vein = swollen, enlarged and dilated vein
- caused by weakness in the one way valves/ walls of the veins. One way valves unable to prevent the backflow of blood leading to the pooling of blood within veins.
- Presents as blue/ purple swollen, tortuous veins in the subcutaneous tissue (just below the skin - superficial veins).
- Can also present with:
- aching and heavy legs
- swollen feet and ankles
- burning/ throbbing in legs
- itchy/ flaky skin over affected vein
- Conditions that can predispose:
- ageing
- female
- pregnancy (increased pressure on veins, diffuclty w venous return)
- obesity (As above).
- standing for prolonged periods or sitting for prolonged periods.
Describe in detail the passage of the short saphenous vein
- Short saphenous vein arised of dorsal venous arch of the foot, travels posterior to lateral malleolus
- Ascends in the midline of the posterior leg alongside the sural cutaneous nerve
- travels deep into the popliteal fossa via the crural fascia and empties into the popliteal vein.

How can damage to the sural nerve present?
- Damage to sural nerve can present with burning pain (paraesthesia)/ diminished sensation/ numbness from the midline of the knee and posterior leg/ lateral side of the foot.

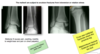
Lable the image:
what veins are shown
what are the dilated regions?
what muscles does the venous plexus in the R image sit between?

Left image:
- top = femoral vein
- popliteal vein
Right image:
- Posteior tibial vein draining into popliteal
- Peroneal/ Fibular vein draining into popliteal
The dilated regions shown in the venogram are the one way valves.
Venous plexus sat inbetween the two heads of gastrocnemius and soleus muscles.

What is the clinical relevance of the deep venous system in the lower limb?
Deep vein thrombosis (DVT) = blood clot that forms in the deep veins of the lower limbs, causing blockage of the vessel.
Causes pain, swelling, tenderness / redness of affected limb.
Main complication = Pulmonary embolism –> thrombus dislodged, travels into the pulmonary circulation, prevents oxygenated blood returning to the heart resulting in mechanical shock.
High risk patients:
Virchows triad –> High coagulability, endothelial injury, stasis of blood flow
E.g. post surgical immobility (stasis of blood), factor 5 leiden thrombophilia (genetic predisposition to clot formation, hypercoaguability).

Describe the popliteal fossa
Label the image

Popliteal fossa:
- superolateral border = two heads of biceps femoris
- Superomedial border = semitendinosus and semimembranosus
- Inferior border = formed by two heads of gastrocnemius
- Floor -> posterior surface of knee joint capsule
- roof –> popliteal fascia and skin
Contents:
Sciatic nerve seen between the biceps femoris and the semitendinosus/ semimembranosus muscles
Splits into the tibial nerve which passes into the posterior compartment of the leg and supplies the muscles of the posterior leg and dorsal foot.
Splits into the common fibular / peroneal nerve that passes laterally to innervate the lateral compartment of the leg.

What does the common peroneal/ common fibular nerve branch into?
What regions of the lower limb do these branches innervate?
Label the image shown

- Common peroneal/ fibular nerve branches into superficial fibular nerve and deep fibular nerve.
- The common fibular nerve passes around the fibula neck and is vulnerable to damage here, splitting into the superficial fibular (Which moves laterally) and the deep (moves anteriorly).
- Superficial fibular nerve innervates the lateral compartment of the leg
- Deep fibular nerve innervates the anterior compartment of the leg

What type of injuries are common in the common fibular nerve?
What issues would present in a patient with:
Superficial fibular nerve damage
Deep fibular nerve damage
- Common fibular nerve susceptible to damage as it passes laterally around the fibular neck, particularly Crush injuries
- Crush injuries that occur during car accidents, car bumper hits calf region.
- Superficial fibular nerve innervates lateral compartment of the leg which prevents excessive foot inversion and allows eversion. Damage presents with excessive inversion of foot.
- Deep fibular nerve innervates the anterior compartment of the leg which allows inversion and dorsiflexion of the foot. Damage here presents with foot drop.
- Foot drop may be compensated for by high stepping gait or circumduction gait to allow patients foot to clear the floor. Also presents with toe- heel tapping.

Describe the arterial supply to the lower limb starting from the abdominal aorta
Abdominal aorta splits into the R and L common iliac @ L4.
Common iliac splits at sacroiliac joint into the internal and external iliac arteries. (Approx at L5 - S1)
Internal iliac artery goes on to supply the organs of the pevlvis, perineal and genital regions.
External iliac artery continues into the anterior compartment of the thigh, passing under the inguinal ligament to become the femoral artery contained in the femoral triangle.
In the femoral triangle the femoral artery gives off posterolateral artery –> Profunda Femoris
Profunda femoris gives deep penentrating arteries to the muscles of the anterior thigh, and medial and lateral circumflex arteries which give off retinacular arteries to supply the femoral head.
Femoral artery continues down anterior thigh through the adductor canal and passes through the adductor hiatus in adductor magnus muscle.
Here it enters the popliteal fossa and becomes the popliteal artery.
Popliteal artery splits into anterior tibial artery and tibioperoneal trunk
tibioperoneal trunk splits to give posterior tibial artery and fibular artery.
Anterior tibial artery runs into anterior compartment of the leg and continues on dorsum of the foot as dorsalis pedis.
Posterior tibial artery continues into the sole of the foot, passing posterior to medial malleolus in tarsal tunnel. Pulsation is palpable here. Continues as deep plantar arch.

Fill the blanks
Attach Images

- Femoral artery relatively subcutaneous in femoral triangle –> stab and surgery risk
- Profunda femoris passes close to neck of femorus and shaft, branches pass through adductor magnus
- Femoral artery continues under sartorius, enters adductor hiatus and into popliteal fossa.
- Popliteal artery passes close to supracondylar part of femur, susceptible to bleeds during femoral fracture.
- Aneurysm of popliteal artery presents as pulsatile fossa swelling
- Popliteal artery splits into anterior tibial and tibiperoneal trunk.
- Anterior tibial artery passes deep in anterior compartment
- Anterior tibial artery continues into dorsum of foot as dorsalis pedis, lateral to the extensor hallucis longus tendon.
- posterior tibial artery passes under soleal arch deep in posterior compartment.
- Posterior tibial artery passes posterior to medial malleolus in tarsal tunnel, pulsation palpable.

label the arteriogram


What does the anterior tibial artery continue as in the foot?
How would you find this branches location?
Where does this branch travel towards?
What nerve does the anterior tibial artery run alongside?
- Anterior tibial artery continues as the dorsalis pedis in the dorsum of the foot.
- Located just lateral to the tendon for extensor hallucis longus
- Dorsalis pedis continues towards the 1st webspace where a branch passes deep to join arterial arch on the sole of the foot.
- Anterior tibial artery runs alongside the deep fibular nerve in the leg.

What does the popliteal artery continue as?
Label the image

- Popliteal artery continues as the posterior tibial artery
- Femoral artery travels through adductor canal and adductor hiatus over supracondylar region into popliteal fossa.
- Popliteal artery travels through popliteal fossa, is palpable and proximal to femur.
- Splits into anterior tibial and tibioperoneal trunk.
- Anterior tibial travels deep, passes anterior to interosseus membran and into dorsum of foot as dorsalis pedis
- tibioperoneal trunk splits to give fibular artery and continues as posterior tibial artery. Passes deep in posterior compartment and posterior to medial malleolus into tarsal tunnel, continues as plantar arteries on sole of the foot.

What is the tarsal tunnel?
What passes through the tarsal tunnel?
- Tarsal tunnel is a space behind the medial malleolus formed between the bones and the overlying fibrous flexor retinaculum.
- Passing through the tarsal tunnel is the tibial nerve, continuing into the sole of the foot as the plantar nerve.
- anterior to this is the posterior tibial artery, continuing into the sole of the foot as the medial and lateral plantar arteries.
Tarsal tunnel:
How could you locate:
posterior tibial artery
tibial nerve
How would damage to the tibial nerve here present?
- posterior tibial artery located 1/3 of the way from a line from medial malleolus to the calcaneus.
- The tibial nerve is just posterior to this pulsation by the posterior tibila artery.
- Damage to the tibial nerve presents as pain/ tingling on the sole of the foot.
label the image


Label the contents and covering of the tarsal tunnel


Tarsal tunnel:
What could happen to tendons if they wear excessively on the bones they pass around?
What symptoms will the patient have?
what could consequently happen to the arches of the feet?
- Both the flexor hallucis longus and flexor digitorum are used in the push off phase of walking
- With excessive use the tendons can wear on the bone and eventually snap or rupture.
- consequentially patient will have major pain and difficulty during push off phase of walking
- Tendons also support the arches of the foot –> therefore can lead to secondarily acquired pes planus (flat foot).

What bones form the ankle joint?
What type of joint is the ankle joint?
What movements does the ankle joint allow?
What supports the ankle joint?
When is the ankle joint its least stable?
- Ankle joint = synovial hinge joint formed between the tibia, talus and fibula.
- Ankle joint has a limited range of movement and permits 2 movements: plantarflexion and dorsiflexion.
- It is supported by strong collateral ligaments
- Is the least stable during plantarflexion.