Dementia Pathology Flashcards
What is the most common cause of dementia?
Alzheimer’s disease
What is the second most common cause of dementia overall?
Vascular disease -multi-infarct dementia -congophilic angiopathy -Binswanger’s disease
What is the second most common neurodegenerative cause of dementia?
LBD = Lewy’s Body Disease
Describe neuritic plaques
-amyloid beta peptide accumulations in the extracellular space

Describe neurofibrillary tangles
Accumulation of hyperphosphorylated tau protein that cause neuronal dysfunction and eventually neuronal death
What is congophilic angiopathy?
A-beta deposition in the walls of blood vessels in the CNS

Describe three changes in the gross anatomy of the brain that occur in Alzheimer’s disease progression
1) shrinkage of the cerebral cortex
2) shrinkage of the hippocampus (specifically loss of cholinergic pathways)
3) enlargement of ventricles (secondary to decrease in brain matter volume)

Define hydrocephalus ex vacuo
Enlargement of the cerebral ventricles or subarachnoid space
-usually due to brain matter atrophy (not increased CSF pressure like hydrocephalus)
What is tau protein’s normal function in the body?
Stabilizes microtubule formation in axons to maintain structure of the neuron
What happens to Tau protein in Alzheimer’s disease that contribues to the pathology?
-Tau protein gets phosphorylated, which changes its conformation and therefore its ability to perform properly
=> microtubules dissasemble which impairs axonal transport
-also hyperphosphorylated aggregates to form oligomers and neurofibrillary tangles that are toxic to neurons

What are pick bodies?
Histological/pathological finding of Alzheimer’s disease
- pick bodies = spherical aggregates of Tau proteins in neurons
- visible via silver stain

How long before onset of dementia symptoms do A-beta accumulations begin?
About 20 years before onset of dementia
Which start to accumulate first: A-beta or tau protein?
A-beta comes first
- A-beta starts accumulating about 20 years before onset
- Tau proteins start accumulating about 10 years before onset

Name two diseases besides AD that have tau-positive filamentous accumulations
- Down’s syndrome
- Fronto-temporal dementia
What is a presenilin mutation associated with?
-presenilin is an amyloid precursor protein
=> prensilin mutation => early onset AD due to earlier neuritic plaque acumulation
-familial/early onset Alzheimer’s

What percent of AD cases are familial vs. sporadic?
5% familial (PS1, PS2, APP mutations), onset < 65 yoa
95% sporadic, onset > 65 yoa
What are some environmental risk factors for AD?
- age, HTN, hypercholesterolemia, stroke, diabetes
- head trauma
What is the strongest genetic risk factor for AD?
ApoE genotype
-E4/E4 homozygotes have an 8-10x increased risk of developing AD
What is the mechanism of ApoE’s role in AD?
ApoE localizes w/ Abeta plaques
- ApoE binding helps stsabilize Abeta polymers
- apolipoprotein E4 promotes Abeta aggregation and impedes brain clearance

What are two possible immunotherapeutic options against AD?
Monoclonal antibodies against Tau protein and Abeta
How can Binswanger’s Disease be prevented?
By managing HTN and DM thoughout the lifespan in attempt to prevent atherosclerotic build up in the blood vessels of the CNS
What is Binswanger’s disease?
Vascular dementia
= subcortical leukoencephalopathy
-arterioles get infiltreated w/ lipid (so associated w/ HTN and/or DM) which causes loss of perfusion to surrounding neurons which causes demyelination
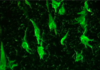
Binswanger’s Disease
(a) Arteriole walls
(b) Perivascular space
(c) Location of demyelination
(d) Cerebral ventricle size
Binswanger’s Disease
(a) Thickened arteriole walls due to lipid infiltration
(b) Widened perivascular space
(c) Perivascular demyelination resulting from vessel pathology
(d) Enlarged ventricles due to shrinkage and softening of white matter

What is a possible link btwn AD and vascular dementia?
Abeta deposition is toxic to endothelial cells => Abeta dposition can predispose to hemorrhage and ischemia (contributing to vascular dementia)








