Day 12 PAEDS Flashcards
A 3 year old girl presents to A&E after her mother saw her have a ‘fit’.
The child was running around and hit her head on their coffee table.
Her mother reports that after hitting her head, she fell to the ground, turned pale and her arms and legs shook violently.
This lasted for about 10 seconds before her daughter regained consciousness and turned pink again.
She has otherwise been well recently and has no significant past medical history.
On examination, the child appears well and is now contently playing with some blocks in the waiting room.
What is the most likely cause of this episode?
Vagal stimulation
This episode of a generalised tonic-clonic seizure after head trauma with rapid recovery and no post-ictal confusion is consistent with a reflex anoxic seizure.
A reflex anoxic seizure is caused by overactivity of the vagus nerve, causing vasodilation and a collapse from a temporary reduction in cerebral perfusion.
A 12 year old girl is seen for her annual review in renal clinic following a diagnosis of polycystic kidney disease when she was 2 years old. She has hypertension which is successfully managed using ramipril. Her routine bloods are taken in clinic and her estimated glomerular filtration rate comes back as 50ml/min.
What is the stage of her chronic kidney disease?
Stage 3
The estimated glomerular filtration rate range for stage 3 chronic kidney disease is 30-59ml.
A mother brings in her neonate to the GP for her 6-week check.
The mother has a past medical history of bipolar disorder, and gave birth via spontaneous vaginal delivery at 38 weeks with no complications.
The GP hears a pan-systolic murmur on auscultation and so is referred for an echocardiogram.
Cardiac echocardiogram shows;
- an enlarged right atrium
- a small right ventricle
- tricuspid incompetence
What is the most likely diagnosis?
Ebstein’s anomaly
The mother suffers from bipolar disorder and so is most likely taking Lithium monotherapy which, in pregnancy, can cause a congenital heart defect known as Ebstein’s anomaly.
This is characterised by;
- an enlarged right atrium
- a small right ventricle
- tricuspid incompetence
A neonate on the intensive care unit has dysmorphic features, difficulty feeding and is not gaining weight.
He desaturates when feeding and his breathing at rest in noisy.
He is being nursed prone and is fed via a nasogastric tube.
The consultant diagnoses the Pierre Robin sequence.
Which of the following best describes the Pierre Robin sequence?
- Cleft palate
- retracted tongue
- small lower jaw
This makes feeding infants difficult.
Specialised feeding equipment is used before surgical repair.

A father presents to the GP surgery with his six year old son.
The boy is shy and embarrassed but tells you after careful prompting that he is wetting the bed nightly.
You discuss the situation, and after ruling out organic causes, explain that bedwetting is a common phenomenon.
You learn that the boy has been using a star chart for the last month or so.
What would be the appropriate next step in management?
Enuresis alarm
An alarm that wakes the child to alert them to bed wetting, allowing them to pass urine in the toilet, is a useful addition to a star chart. The family already treat the bedwetting in a matter of fact and non-judgemental way. The boy is old enough to assist his parents in cleaning up the mess.
A 14 year old girl as admitted following an overdose.
She loses consciousness during the clerking and has no pulse.
CPR is commenced. The ECG shows the rhythm below.
What does the ECG show?
What is the most appropriate course of action?

Defibrillation
The rhythm shown is ventricular fibrillation, which is a shockable rhythm.
Evidence indicates the two biggest factors enhancing the survival of patients who have arrested is good quality compressions and prompt defibrillation if they have a shockable rhythm.
A 13 year old boy presents to the GP because his mum is worried that he has recently been ‘going blue’.
Friends and family have commented that he looks a bit blue.
On questioning, he reports feeling a little short of breath when playing football, but otherwise reports feeling well.
His mother says he has no known conditions apart from a hole in the heart that was mentioned early on but was never followed up on.
On examination, he appears moderately cyanotic.
He has clubbing of the fingernails.
There is a harsh holosystolic murmur loudest at the lower left sternal edge. The lung fields are clear to auscultation.
His oxygen saturations are 93%, respiratory rate is 18, heart rate is 80, and temperature is 36.8.
What is the most likely underlying cause of this patient’s colour change?
What is the diagnosis?
Reversal of direction of cardiac shunting
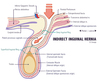
Eisenmenger syndrome describes the reversal of a left-to-right shunt (patent ductus arteriosus, atrial septal defect, or ventricular septal defect) to a right-to-left shunt.

A newborn is noted to have an intermittent squint at the newborn baby check.
What is the most appropriate management?
Refer if still present at 8 weeks
This is the recommendation for a squint in a newborn.
Many children have a squint in the first few weeks of life as the muscles are still weak.
However, most babies grow out of it quickly.
A squint persisting beyond 8 weeks is suspicious and treatment and investigations need to start as soon as possible to ensure the child does not develop amblyopia.
A newborn baby on the neonatal ward has difficulty feeding.
You notice that the baby is constantly drooling saliva and coughs up breast milk after feeding.
The pregnancy was complicated by polyhydramnios. The mother is a 38 year old primip.
On examination of the baby, there is upslanting palpebral fissures and a sandal toe gap.
What is the most appropriate initial investigation to determine the acute diagnosis?
NG tube and a chest X-ray
This is the diagnostic investigation to confirm oesophageal atresia.
The NG tube is passed down until it cannot be advanced any further.
An X-ray is taken at this point.
The tip of the NG tube is radio-opaque so the x-ray will show the level of the atresia.
A previously well 8 year old girl is seen at the General Practitioner following five days of dysuria.
She is otherwise well, with normal observations and examination.
Urine dipstick results are as follows:
- Leuks: ++
- Nitrites: ++
- Hb: -
- Ket: Trace
She is commenced on antibiotics.
What additional investigation should this patient have?
Urine microbiology
All urinalyses indicative for a urinary tract infection (UTI) should be sent for microscopy, culture and sensitivities. This will help inform both current and potentially future treatments. It also is advised in the NICE guidelines for UTIs in children.
What is the purpose of a DMSA Scan?
(2)
This is a scan to check for renal scarring.
It is especially pertinent in very young children with developing kidneys or those with recurrent urinary tract infections (UTIs).

What is the purpose of a Micturating cystourethrogram (MCUG)?
(2)
A micturating cystourethrogram is a form of functional imaging that looks urine flow and bladder function.
It might be indicated in some children with recurrent urinary tract infections (UTIs) or suspicions of overactive bladders.
An 18 month old boy is brought to A&E after his father saw him ‘have a fit’.
He has had a fever up to 39.0 degrees for one day, along with a runny nose and cough.
His father says his son was crying and then lost consciousness and started rhythmically jerking his limbs for around two minutes.
The boy regained consciousness shortly after but has been miserable and lethargic since.
Nothing like this has ever happened before, and the boy is normally fit and well.
What is the chance of something like this happening again in future?
30-40%
This boy with a short history of an upper respiratory tract infection with a high fever has had a febrile convulsion.
Febrile convulsions (or febrile seizures) are relatively common, occurring in around 3% of children.
Once a child has had one febrile convulsion, although the risk of epilepsy is low, the risk of having a future febrile seizure is high, around 30-40%.
A 5 year old boy presents to A&E with vomiting and lethargy.
His mum says he has been feeling feverish since he woke up this morning. He complained of a headache all day at school, and she had to collect him at lunchtime as he vomited. Since then, he has rapidly got worse and complained that his neck felt stiff and that the light hurt his eyes. She brought him in when she found a purple rash on his leg that stayed the same when she put a glass against it.
In the department, the boy appears unwell and drowsy. His respiratory rate is 36 and saturations are 99% in air. His heart rate is 60, blood pressure is 170/90 and capillary refill time is 3 seconds. His temperature is 39.0 degrees. His pupils are dilated and poorly reactive. There is a purpuric rash on his left ankle. Flexion of the neck causes involuntary flexion of the knees.
After your ABCDE Assessment and contacting a senior, what is the most important next step in managing this child?
Start IV antibiotics
This child with a headache, fever, vomiting, purpuric rash and photophobia, along with a positive Brudzinski’s sign (neck flexion triggers involuntary knee/hip flexion), has bacterial meningitis. This child is extremely unwell and has signs of raised intracranial pressure. The most important next step for this child is IV antibiotics.
A 7-year-old boy is brought into A&E via ambulance after falling off his bike. His parents report that he hit his head on the pavement and was unconscious for around 1 minute. He has vomited three times in the ambulance and once in A&E, and has remained drowsy since his fall. On clinical examination, there is extensive bruising over the right mastoid process, but no other signs of trauma. There is no focal neurology and his GCS is calculated to be 13.
Which of the following is the next best step in this child’s management?
CT Head within 1 hour
This is the correct answer. This child has vomited more than 3 times, has a reduced GCS and demonstrates signs of a basal skull fracture (bruising over the mastoid process) following a head injury, which are all worrying features that warrant a CT scan within the next hour. CT heads are useful for assessing the impact of trauma and guiding management.
A 4 year old boy is found collapsed on the floor.
He is unresponsive and does not have a pulse.
Which rhythm is the resus team most likely to find on his ECG?
Asystole
Asystole is the most common finding at paediatric cardiac arrests. It is not entirely clear why.
However, there is speculation that this is the most common rhythm as a result of respiratory causes being the most common cause of paediatric arrest, with hypoxia causing profound bradycardia and asystole in severe cases.
A 27 day old neonate is brought in to Accident and Emergency by his mother as she noticed that he is not feeding well.
The baby is exclusively breast fed and has not had any problems with latching on before.
The baby was last weighed a few days ago, and has been putting on weight.
On examination, the baby looks jaundiced and is lethargic.
The stool is of a normal colour and consistency.
The mother says that there have been fewer wet nappies over the last 12 hours.
There is some loss of skin turgor.
There is no hepatomegaly on palpation of the abdomen.
What is your most appropriate management?

Perform a full septic screen
This is correct because in a jaundiced unwell baby, sepsis is the first thing which has to be investigated due to the devastating consequences (organ failure, kernicterus, death). A urinary tract infection (UTI) is a common serious cause of jaundice in the newborn, and can often present with vague symptoms of lethargy or difficulty feeding. UTI in a newborn is particularly serious as it can rapidly progress to sepsis.
Normal neonatal jaundice occurs between 2-14 days
A 2-year-old child presents to paediatric A&E with her mother.
She has had difficulty breathing for the past two nights and has a barking cough.
On examination, there is no evidence of stridor or respiratory distress.
All other observations are normal.
Which of the following is the next best step in the management of this patient?
Give oral Dexamethasone
This is the correct answer. This patient has mild croup (evidenced by the lack of stridor and respiratory distress, and normal vital signs), which is managed with a single dose of oral Dexamethasone 0.15mg/kg.
When can chickenpox patients go back to school?
When all lesions have crusted over.
This girl presents with features in keeping with chicken pox, caused by varicella zoster. The virus is contagious from 1-2 days before the rash appears, until all vesicular lesions have crusted over.
A 4 year old boy who was recently adopted from Peru is brought into the paediatric clinic following referral by his GP who is concerned about his delayed growth.
On examination the patient is noted to have muscle wasting in the gluteal region.
On questioning his mother reports that his stools are often very yellow and often take many attempts to flush.
He has also suffered from frequent chest infections for as long as she can recall. She has not noticed any other changes recently.
Given the most likely diagnosis what would be the most appropriate investigation to order next?
Sweat test
As ions cannot be reabsorbed from the sweat a high to very high concentration of chloride ions will be noted.
A positive sweat test is defined a sweat chloride >60 mmol/L [b %60 mEq/L]. A positive result should prompt immediate referral to a cystic fibrosis specialist.
A 4 year old boy is seen at the GP after developing a pruritic rash on his face which has persisted for 5 days.
It started near has nose and now has spread to both sides of his face.
The lesions are erythematous and slightly weepy.
Some have a golden crusting over them.
His observations are stable and he has a temperature of 37.8C
What is the appropriate course of treatment?
What is the diagnosis?
What is the causative agent?
Fusidic acid
This boy has impetigo,
which is most commonly caused by Staphlyococcus aureus.
An appropriate treatment would be topic fusidic acid.
Hydrogen peroxide 1% cream is currently considered first line but this is not an option here.
7 year old girl is brought into the GP practice by her parents who noticed that she had her first period last week.
Her mother reports that she started her own periods early at 10 years of age.
On examination the GP notices breast budding and sparse pigmented pubic hairs around the labia.
She is plotted in the 99th percentile for height on her growth chart.
Her parents confirm that she is otherwise doing well and has not had any problems in school.
What is the medical term for this phenomenon?
What would be the most appropriate next step for the GP to take at this stage?
Refer to paediatrics
This girl has clearly entered puberty at a very early age.
Whilst this is not unheard of and the most likely cause of precocious puberty is that she has simply entered normal puberty prematurely, such an early onset of puberty should prompt a referral to a paediatric endocrinologist in order to investigate a possible cause and initiate treatment.
A boy born at 31 weeks gestation is admitted to neonatal intensive care following a ventricular haemorrhage.
The boy is at risk of central apnoeas.
On the ward round, there is a pause in his breathing that is lasting 15 seconds.
What is the most appropriate course of action?
Physical stimulation
Physical stimulation is the first step that should be considered to see if this triggers the baby to start breathing again.
After that, one should move onto an airway manoeuvre and supplying artificial breaths on oxygen via a bag-valve-mask if in a hospital setting.
A 3 year old boy is brought to A&E by his mother who is very worried about him.
He has been lethargic for the last 24 hours, not wanting to eat or drink much and his mother says he looks pale compared to normal.
Prior to that he was well, with no cough, coryzal symptoms or sign of infection.
He has a history of type 1 diabetes mellitus, which is managed with a basal-bolus insulin regime, administered in three daily doses.
His blood sugars are well controlled.
On examination the boy is laid down on the bed, rousable to voice but closes his eyes again soon after.
There is no visible rash, heart sounds are normal and chest clear on auscultation.
He has some mild suprapubic tenderness but no guarding or rigidity of the abdomen. Bowel sounds are normal.
Vital observations: temperature 38.4 degrees Celsius, heart rate 120bpm, respiratory rate 24/min, oxygen saturation 98% on room air, blood pressure 100/70.
Which of the following options is the most appropriate initial management of his presentation?
What is the diagnosis?
Cephalexin
Cephalexin is a broad-spectrum antibiotic that can treat urinary tract infections.
Although this boy has a suspected urosepsis, it is most appropriate to administer a broad-spectrum antibiotic in the first instance, until identification of the source of sepsis can be confirmed.
A 32-year-old primigravida attends a routine GP appointment with her partner to discuss the risk of having a child with cystic fibrosis. Neither herself or her partner have been diagnosed with cystic fibrosis and they are yet to undergo any screening tests to identify whether they are carriers of the cystic fibrosis gene.
What is the risk of their first child being affected by cystic fibrosis?
1 in 2500
This is the correct answer. In Europe, each parent has a 1 in 25 chance of being a carrier for the cystic fibrosis gene. If both parents were to be carriers of the gene, then the risk that their child is affected by cystic fibrosis is 1 in 4, as it is an autosomal recessive condition.
1/25 x 1/25 x 1/4 = 1/2500
A 9 year old boy is brought to A&E for difficulty in breathing that started at a school football practice.
On arrival at the department, he is unable to complete sentences, has a respiratory rate of 44 and a diffuse wheeze is heard throughout the chest on auscultation.
He is treated with high flow oxygen, back-to-back salbutamol nebulisers, ipratropium bromide nebulisers, and IV magnesium sulphate.
After these treatments, his respiratory rate is 8 and his chest is quiet to auscultation. His blood gas shows a pH of 7.42, pCO2 of 4.9 and pO2 of 9.6.
What is the most appropriate next step in managing this patient?
Call anaesthetist immediately
This patient is having an asthma attack and is deteriorating quickly.
In this patient, a silent chest and a normalising pCO2 are signs of impending respiratory failure as the respiratory muscles are nearing exhaustion.
An anesthetist should be called immediately to help with this rapidly tiring patient, as they might require urgent intubation.
A mother is worried that her daughter’s development may be delayed. On assessment the doctor reports the following:
- The child is able to follow commands and responds to conversation in 3 or sometimes 4 word sentences.
- She responds when asked that her favourite colour is purple.
- Her mother reports that she has a vocabulary of approximately 250 words.
If the child’s development were normal how old are they most likely to be?
3 years
A 3 year old would be expected to use 3 or 4 word sentences frequently and have a vocabulary of at least 200 words. They should also be able to name one colour and answer when asked their name, age and gender.
A 4-year-old girl is brought to paediatric A&E with sudden-onset difficulty breathing.
Her parents say she has not been herself recently and describe coryzal symptoms over the past 24 hours.
The family recently emigrated from Russia and the parents are unable to recall which vaccinations their daughter has had.
On examination, she is drooling and has a inspiratory stridor.
Her temperature is 40.0ºC, she has a heart rate of 80, a respiratory rate of 43, and her oxygen saturations are 89% on room air.
Give the likely diagnosis.
Give the treatment.
Name the causative agent.
Endotracheal intubation
This child has presented with the cardinal features (sudden onset inspiratory stridor, drooling, high fever) of acute epiglottitis, and her incomplete vaccination history increase the likelihood of this diagnosis, as this condition is quite rare in the UK because all children are vaccinated against Haemophilus influenzae, the most common cause of acute epiglottitis.
This girl is acutely unwell and requires a secure airway before they go into respiratory arrest, therefore this is the priority before anything else should be done.
Endotracheal intubation in this scenario is usually carried out by an anaesthetist.
A 38 year old primip with gestational diabetes mellitus (GDM) has gone into spontaneous labour at 29 weeks.
Following signs of foetal distress, she had an emergency caesarean section.
Two hours later on the neonatal ward, the baby has a respiratory rate of 70 breaths per minute.
On examination, the baby is having difficulty breathing with nasal flaring, grunting and intercostal recession.
The oxygen saturations are 93% on room air. The chest x-ray shows a diffuse ground glass pattern.
What is the most likely diagnosis?
Respiratory distress of the newborn
The stem of the question includes the risk factors for respiratory distress of the newborn:
- prematurity
- maternal GDM
- Caesarean section.
This is a typical presentation with an onset within 4 hours of birth with tachypnoea and signs of respiratory distress (grunting, nasal flaring, intercostal recession).
A 6 week old baby boy is brought to A&E as a GP referral because he is still yellow.
He has been getting progressively more yellow for the last 3 weeks.
His mum says his poo has also changed from thick black when he was born to mustardy to chalky.
His wee has also turned a dark yellow.
Otherwise, he has been breastfeeding well and is growing along his centiles.
He was born at 39+6 by spontaneous vaginal delivery after a normal pregnancy.
Antenatal screening and scans showed no abnormalities.
On examination, the baby appears well.
His abdomen is soft and a liver edge is palpable 2cm below the costal margin.
Antenatal screening and scans were all normal.
Blood tests show a significantly raised ALT, ALP and bilirubin (predominantly conjugated).
What is the most likely underlying cause of this baby’s presentation?
In VCV what is the most appropriate response for the GP to give when advising about the incubation period concerning the son?
Up to 21 days
The rash in this case is chickenpox caused by the varicella zoster virus (VZV).
Patients are infectious up to 3 days before lesions appear and up until the last lesion dries.
The incubation period for chicken pox is up to 3 weeks.
A 4 year old boy is brought by his parents to the GP practice as they are concerned that there is discharge from his right ear.
For the last two days, he has been irritable and tugging on the outside of his ear. He has just recovered from a recent upper respiratory tract infection (URTI). He is afebrile and is alert and active.
On otoscopy, there is a perforated tympanic membrane on the right.
What is the most appropriate management?
Prescribe amoxicillin
Antibiotics are prescribed if there is a perforated eardrum in acute otitis media.
This is recommended as it suggests a more serious infection and antibiotics will reduce the number of days of illness.
A 5 year old girl is brought to A&E with a 6 day history of fever.
Her mother also notices the whites of her eyes look red and that her hands and feet are red and swollen with some skin peeling at her fingertips.
She has swollen neck glands and a red tongue.
What is the most appropriate management?
Aspirin and IV Ig
This child with >5 days of fever, conjunctivitis, erythema and edema of the hands, cervical lymphadenopathy and mucosal involvement (strawberry tongue) most likely has a diagnosis of Kawasaki disease. Kawasaki’s is a rare condition that is treated with aspirin and IV Ig.
An 11 year old with a 6 month history of a wheeze and nocturnal cough was confirmed to have a diagnosis of asthma following spirometry and BDR (bronchodilator reversibility) test, and commenced on salbutamol and an ICS.
Four months later she presents to the GP with poor asthma control.
She has been using her salbutamol at least 10 times a week and is regularly woken at night with coughing.
Which of the following would be the next most appropriate step in her management?
Check inhaler technique
Correct inhaler technique is very important in order to ensure adequate delivery of treatment, and should always be assessed prior to changing management to avoid unnecessary addition of treatments. Children should always have inhalers prescribed with a spacer device (and also face mask if <5 years) in order to improve delivery of medication.
A four year old girl has presented to the GP several times with sore throats and pyrexia in the last two months without a diagnosis. She now presents to the ED with a fever, generalised lymphadenopathy, mild hepatosplenomegaly and a new petechial rash. A full blood count shows anaemia, raised white cells and low platelets. Blood film shows blast cells. What is the most likely diagnosis?
ALL
This is the commonest leukaemia in children (80%). There is marrow infiltration, causing anaemia and thrombocytopenia. Leukaemic blast cells (abnormal lymphocytes) are seen on the blood film and bone marrow biopsy.
A 2 year old girl is brought in to A+E by her parents as they are concerned about her breathing.
She has a constant high-pitched sound on inspiration.
She looks toxic and is leaning forward.
She is drooling and has a temperature of 39.5 degrees Celsius.
She was born in South America and her family moved to the UK recently.
What is the most likely diagnosis?
Acute epiglottitis
Continuous stridor in a child who looks toxic and is drooling is indicative of acute epiglottitis.
Especially since there is a history of living abroad where she may have missed several important immunisations.
A 5 year old girl presents to the GP with a 2 day history of fever, runny nose and a rash.
The rash is blotchy and red, started on her face and since spread to her chest and abdomen only.
She has no cough or conjunctivitis.
She is otherwise healthy. She takes no medicines.
She has never received any vaccinations because her mother does not think vaccinations are safe.
On inspection, the child appears miserable but well. Her respiratory rate is 16, heart rate is 80 and capillary refill is less than 2 seconds.
Her temperature is 38.0.
She has a fine macular rash across her head and torso, sparing the limbs, and post-auricular lymphadenopathy.
If the mother was 10 weeks pregnant and caught her daughter’s infection, which of the following is the fetus at highest risk of developing?
Deafness
This unvaccinated child with a fever and rash should raise suspicion for a rare infection like measles or rubella.
Although many of the symptoms are nonspecific (fever, rash, coryza), she has some features (rash starting on face and spreading to trunk, post-auricular lymphadenopathy) which are more specific to rubella infection.
There is also a lack of the preceding cough and conjunctivitis that is characteristic of measles infection.
Although rubella infection is generally mild, infection in nonimmune pregnant women puts the foetus at risk for congenital rubella syndrome, which is characterised by cataracts, brain damage and deafness.
A 7 year old girl with a history of asthma is brought to the GP by her mother as she is unable to keep up with the sports activities in school.
She is also getting symptoms at night and this is affecting her ability to concentrate in school.
She is currently on a salbutamol inhaler when required and 50 micrograms beclomethasone inhaler twice a day.
What is the most appropriate next step in management?
Start Montelukast
According to BTS guidance, if asthma is uncontrolled in children over 5 on a paediatric very low dose of ICS (inhaled corticosteroid) as maintenance therapy, you should add a leukotriene receptor antagonist (LRTA) such as montelukast.
The other option would be a long-acting beta-agonist (such as Salmeterol)
A mother brings in her 9-year-old son to the GP saying he has been feeling unwell, with a fever for the past 24 hours.
She reports he had tummy pain all day yesterday and vomited last night, and refused to eat breakfast this morning.
He is drinking normally and passing urine, and had one episode of loose stools today, which did not contain blood.
On examination, the child is pale.
Abdominal examination reveals generalised tenderness with guarding and tenderness to percussion.
Genital examination is unremarkable. Urine dipstick is normal.
His observations are: heart rate 130, blood pressure 80/50, oxygen saturation 98% on air.
Which of the following is the most likely diagnosis?
Appendicitis
The patient likely has appendicitis, and his observations (tachycardia, hypotension) suggest his appendix may have ruptured.
Appendicitis in children often presents with central abdominal pain (which later radiates to the right iliac fossa), vomiting and there may be a low-grade pyrexia.
The child is septic and needs to be taken to A&E for immediate treatment (intravenous fluids and antibiotics initially) which will likely involve surgery.
On the post-natal ward, a two-hour old baby boy born by spontaneous vaginal delivery at 38 weeks chokes whilst feeding.
His mother was giving him a bottle for the first time, and after about 30 seconds the baby started coughing, choking and vomiting milky white fluid.
The baby turned blue during this episode.
Now, 30 minutes later, he is pink in air but tachypnoeic with saturations of 96% and tachycardic.
An NG tube is inserted and the position checked with a chest X-ray which shows the tube is unable to move beyond an upper oesophageal pouch.
Which of the following is the most likely underlying cause of this choking episode?
Blind-ending oesophagus
Oesophageal atresia is a congenital disorder where the oesophagus fails to develop properly.
A six-year old girl presents to ED with her mother, who is worried.
Over the last week and a half the child has had a fever with a headache.
In the last two days the child has developed diarrhoea and a red rash covering her cheeks that spares the nasolabial folds.
She is also complaining of pain in her knees.
The child has been otherwise well, and has completed her vaccines.
What is the most likely diagnosis?
Parvovirus B19 infection
This is a very typical presentation of parvovirus B19 infection.
It is a DNA virus spread predominantly through respiratory secretions.
In children it causes fifth disease.
The ‘slapped cheek’ rash is typical, and shows sparing periorally and on the forehead.
It causes an initial viral prodrome.
In patients with disorders of the red blood cells it can cause an aplastic crisis.
A 2 week old baby boy, born prematurely at 29 weeks gestation, is seen during ward round on the neonatal unit.
He was delivered by emergency C-section for reduced foetal movements. He was born in fair condition with APGAR scores of 4, 5 and 6 at 1, 5 and 10 minutes of life. The baby was transferred to the neonatal unit and required two days of intubation and two doses of intra-tracheal artificial surfactant. There were no concerns in the rest of the pregnancy, and all antenatal scans were normal. He is being fed with fortified maternal expressed breast milk via syringe, and has good urine output.
On inspection, the baby is pink in air and has vigorous spontaneous movements. His chest is clear and abdomen is soft and non-tender without organomegaly. He is afebrile and his observations are within normal ranges. His weight is between the 2nd and 9th centile, and his head circumference is on the 95th centile. His white cell count is 3.0 and CRP is <0.6.
What is the most suitable next investigation in this baby?
Cranial ultrasound
This premature baby with a huge disparity between centiles for head circumference (very large) and weight (very small) most likely has hydrocephalus (buildup of CSF). As the suture lines of the skull are not fused at this stage, the head circumference can rapidly increase as the skull bones move apart to accommodate the excess fluid. The best option to investigate hydrocephalus is with a transcranial ultrasound scan. This premature baby may have had an intraventricular haemorrhage, leading to hydrocephalus.
A junior doctor is called to review a neonate that was born earlier today at term by spontaneous vaginal delivery.
The mother is concerned about a swelling on the baby’s head.
On examination there is a 3cm x 4cm central swelling on top of the baby’s head, which crosses suture lines.
The swelling has a border and is a normal colour.
The neonate is well otherwise.
Which of the following is the most likely diagnosis?
Caput succedaneum
Caput succedaneum is a collection of fluid that collects due to pressure on the head during vaginal delivery. (C)aput (s)uccedaneum (c)rosses (s)uture lines. This will usually spontaneously resolve within days.
Characterisitics of Cephalohaemotoma
(2)
A cephalohaematoma is a haemorrhage which does not cross suture lines and is periosteal.
This is benign and self resolves within the first few months of life.
A 1-year-old child presents to the GP with her parents who are concerned because she has been unwell for the past 4 days.
They say for the first 3 days her temperature was 38.4C, and this has come down since then and she is now afebrile.
They are now worried because since yesterday they have noticed a rash on her chest, with minimal spread.
On examination there is cervical lymphadenopathy and a maculopapular rash on the child’s chest.
What is the diagnosis from the picture?
Which of the following is the most likely causative organism of this child’s condition?

- roseola infantum
- Human herpes virus 6
A 3-5 day fever followed by a maculopapular rash is characteristic of roseola infantum, a condition caused by human herpes virus 6.
A 4-week-old baby girl is brought into A&E by her parents as they are concerned that her skin is yellowing.
On further questioning, the parents report that she has been feeding well and growing along her centiles, but her stools have recently become very pale.
She was born at term by spontaneous vaginal delivery and all antenatal screening tests came back as normal.
Blood tests reveal: ALT 50 U/L, ALP 873 U/L, total bilirubin 135 mmol/L, conjugated bilirubin 110mmol/L. On abdominal examination, masses can be palpated in both the left and right upper quadrant.
What is the most likely diagnosis?
Biliary Atresia
Biliary atresia is a paediatric condition where the bile ducts become progressively fibrosed and obliterated, which obstructs the flow of bile and presents as cholestasis in the first few weeks of life.
Abnormally high levels of conjugated bilirubin is a characteristic finding in biliary atresia.
The spleen becomes palpable in the 3rd-4th week of life (LUQ mass), with the liver also becoming enlarged (RUQ mass).
Prolonged neonatal jaundice with a raised conjugated bilirubin fraction, is biliary atresia until proven otherwise.
A six year old girl presents to the GP with a rash. The rash has been present for around one month, and comes and goes.
It is itchy and erythematous, and affects the flexures.
She has had no febrile illnesses recently and developed normally.
The child is otherwise well, and only uses a preventer inhaler and antihistamines for hayfever.
What is the most likely diagnosis?
Atopic dermatitis
The history and examination findings suggest atopic dermatitis (eczema). In children it typically affects the flexures (antecubital and popliteal fossae, and neck). It is associated with hayfever, other allergies and asthma. It may resolve during puberty, a minority represent in early adulthood.
A young woman attends a GP surgery with her newborn son for a routine check-up.
The boy was hypotonic at birth, has Brushfield spots in the iris, and is known to have a congenital heart defect.
What is the most likely diagnosis?

Trisomy 21
Hypotonia at birth, congenital heart defects (occurring in 40%) and Brushfield spots are features of trisomy 21 (Downs). Brushfield spots are small, white-grey aggregations of connective tissue at the peripheral iris.