Chronic inflammation Flashcards
chronic inflammatory conditions are
incredibly common - not usually life threatening - debilitating (IBD and RA)
definition
prolonged inflammation with associated repair
characterised by
- Delayed onset - Variable duration (days years) - Variable appearances • No 5 cardinal features - Limits damage, initiates repair - Can cause debilitating symptoms
how does chronic inflammation arise
- Takes over from acute inflammation- if resolution not possible with acute inflammation
- Develops alongside acute inflammation- severe/persistent irritation
- Arises “de novo”- without preceding acute inflammation e.g. autoimmune conditions - Rheumatoid arthritis/ IBD/ diabetes
sometimes the proportion of cell types can
indicate diagnosis
which cells are indicative of rheumatoid arthritis
mainly plasma cells
which cells are indicative of chronic gastritis
mainly lymphocytes
which cells are indicative of of leishmaniasis (protozoal infections)
mainly macrophages
which cells are involved in chronic inflammation
- Macrophages 2. Lymphocytes- T/B cells 3. Mast cells 4. Eosinophils 5. Fibroblasts 6. Giant cells
macrophages in circulation
monocytes
macrophages once entering tissue space
macrophage (histiocyte)
features of macrophages
- big cells with a large cytoplasm - abundant foamy cytoplasm - slipper shaped nucleus - can look like a cancer cell

primary role of maxcrophage
phagocytosis - removal of pathogens/ necrosis/ debris - antigen presentation to immune system
secondary role of macrophages
- Also produce inflammatory mediators- controls and regulates inflammatory response
macrophages can look different depending on
what stimulus they are eating

lymphocyte features
- large, spherical stained nucleus
- thin rim of cytoplasm
- small
subdivided into T and B lymphocytes (cant distinguish appearance- have to use immunohistochemistry)

T lymphocytes
CD8+ (protein on surface)- Cytotoxic (MHC I)
CD4+- helper T cells (MHC II)
B lymphocyte
Mature into plasma cells
Produce antibodies (immunoglobulins)
Neutralises pathogens
plasma cell features
- Nucleus pushed off to one side (eccentric)
- Chromatin in the nucleus clumps into spheres (clock-face)
- Next to the nucleus there is slightly paler staining- peri- nuclear cytoplasmic clearing –> Golgi due to antibody synthesis
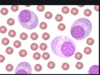
function of plasma cells
fully differentiated B lymphocytes
Produce antibodies
features of eosinophils
- 2 lobes (bilobed nucleus)
- cytolasm stains bright red and granular

why is the cytoplasm of an eosinophil bright red and granuklar
- Full of chemical mediators- Histamine, heparin and prostaglandins
- E.g. Release during hypersensitivity reactions and parasitic infections
features of fibroblasts/myofibroblasts
- webbed cytoplasm
- stretched nucleus

role of fibroblast/myofibroblast
- ‘Prolonged inflammation with associated repair’
- Role in generation and repair
- Produce and secrete and lay down collagen- helping to reconstruct tissue
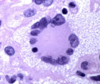
giant cells features
- Multinucleate
- HUGE
- Fusion of multiple macrophages
role of giant cells
- “Frustrated phagocytosis”
- Increasing effectiveness of phagocytosis
- E.g. if there are any resistant foreign body e.g. suture, resistant parasite of bacteria
how many types of giant cell
3
name the 3 giant cells
1) Foreign body giant cells
2) Langhans giant cells
3) Touton giant cells
1) Foreign body giant cells
To destroy foreign bodies
One big cytoplasm
Nuclei randomly assorted

2) Langhans giant cells
- Nuclei line up around the periphery- horseshoe
- Important in TB

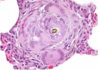
3) Touton giant cell
- Nuclei line up in a concentric circle in the middle of the cell
- Can be seen in fat necrosis

which giant cell associated with TB
langhans giant cell
which giant cell associated with fat necrosis
touton
which type of giant cell

which type of giant cell

Langhans
which type of giant cell
Touton
Effect of chronic inflammation
- fibrosis
- impaired function
- atrophy
- stimulation of immune response
- fibrosis
- a.Deposition of collagen
- b.E.g. chronic cholecystitis, liver cirrhosis
impaired function
a. E,g, IBD
b. Rarely increased function (e.g. thyrotoxicosis in Graves disease- increase production of T3/T4)
atrophy
atrophic gastritis
stimulation of immune repsosne
Antigen presentation- chronic –> brought about by macrophages
fibrosis of the gall bladder
thickened and pale- collagen

impaired functione xample
idiopathic IBD
- Crohns disease
- UC

crohns disease
- can affect all of the GI tract (mouth to anus)
- discontinous patches of inflammation (skip lesions)
- inflammation affects full thickness of the bowel (transmural)
- sometimes find granulomata
- less likely to have rectal bleeding
ulcerative colitis
- affects large boewl only
- continous inflammation
- inflammation affects superficial bowel wall only (mucosa and submucosa only)
- no granulomata
- more likely to have rectal bleeding
cirrhosis
causes impaired function- too much fibrosis and attempted regeneration
e. g. Cirrhoic liver
- alcohol
- hepatitis
- drugs and toxins
- fatty liver disease

granulomatous inflammation found in
chronic inflammation
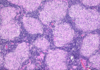
granuloma form
A collection of epithelioid histiocytes (macrophages) with surrounding lymphocytes
May also see giant cells within granuloma

causes of granulomatous inflammation
- forgin body reaction
- infection
- idiopathic
foreign body granulomatous inflammation
granuloma caused by infection
e. g. tuberculosis
e. g. leprae
- dififcult to destory
- thick cell walls
- mycolic acids

idiopathic granuloma
e. g. crohns disease
e. g. sacroidosis (mulitple well formed granulomas form on lymph nodes, lungs and skin - shortness of breath, lumps in lymph and skin lumps)