Anatomy Flashcards
Where does the Upper GI tract end?
Duodenum
Which 3 pairs of muscles are responsible for closing the jaw?
Masseter, Temporalis and Medial pterygiod
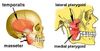
Which pair of muscles is responsible for opening the jaw?
Lateral pterygoid

What is the origin and insertion of the masseter m.?
Angle of mandible to zygomatic arch

What is the origin and insertion of the temporalis m.?
Coronoid process of mandible to temporal fossa

What is the origin and insertion of the medial pterygoid m.?
Angle of mandible (medial side) to pterygoid plates of sphenoid bone

What is the origin and insertion of the lateral pterygoid m.?
Condyle of mandible to pterygoid plates of sphenoid bone

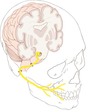
Which nerve supplies all of the muscles acting on the jaw?
Mandibular division of trigeminal nerve – CN V3

Which is the only nerve that attaches to the pons?
Trigeminal nerve
How does the V3 - mandibular branch of trigeminal nerve leave the skull?
Through the sphenoid bone at the foramen ovale

What sits in between the arches of the soft palate?
Palatine tonsils

Where does the anterior 2/3rds of the tongue reside and in what plane does it lie?
It is in the oral cavity, and lies horizontally
Which nerve provides the general sensory supply to the anterior 2/3rds of the tongue?
CN V3 - specifically the lingual nerve (branch of mandibular branch)

Which nerve provides the special sensory supply to the anterior 2/3rds of the tongue?
CN VII (facial)

Where does the posterior 1/3rd of the tongue reside and in what plane does it lie?
It is not in the oral cavity, it is technically the anterior wall of the oropharynx. It lies vertically
Which nerve provides the general and special sensory supply to the posterior 1/3rd of the tongue?
CN IX - Glossopharyngeal nerve

Which nerve supplies general sensation of the superior half of the oral cavity?
CN V2 - Maxillary branch of Trigeminal
Which nerve supplies general sensation of the inferior half of the oral cavity?
CN V3 - Mandibular branch of Trigeminal
What is the gag reflex?
A protective reflex that prevents foreign bodies from entering the pharynx or larynx. Part of the reflex response to touching the posterior wall of the oropharynx is to constrict the pharynx, as the patient attempts to close it off as an entry point into the body
Which nerve provides the sensory supply to the gag reflex?
CN IX - Glossopharyngeal n.
Which nerve provides the motor supply to the gag reflex?
CN IX and CN X - Glossopharyngeal and vagus n.
What is the purpose of spraying a local anaesthetic prior to a endoscopy?
‘block’ sensory action potentials in CN V2, V3, VII and IX, which supply the general sensation to the superior and inferior lower cavity, and sensory and motor supply of gag reflex, respectively
What is the intracranial course of the trigeminal nerve?
Leaves the pons, and passes inferior to the edge go the tentorium cerebella between the posterior and middle cranial fosse
How does V2 - maxillary branch of trigeminal leave the skull?
Through the sphenoid bona via the foramen rotundum
Where does the facial nerve connect at the brain?
Pontomedullary junction
How does the facial nerve leave the skull?
Travells through the internal acoustic meatus in the temporal bone, then most fibres pass out the skull at the stylomastoid foramen
What do the fibres of the facial nevre that leaves the skull via the stylomastoid foramen serve?
Muscles of facial expression

The majority of fibres of the facial nerve leave the skull via stylomastoid formen, however where does the remainder of the fibres go?

The chorda tympani branch: come off before the stylomastoid foramen, joins with the lingual nerve and serves taste and parasympathetic innervation of salivary glands

Where does the glossopharyneal nerve connect with the brain?
Medulla
How does the glossopharyngeal nerve leave the skull?
Therough the jugular foramen - at the jucntion between the temporal and occipital bones
Where does the parotid gland empty into the mouth?
In the mucosa opposite your second upper molar

Where does the submandibular gland empty into the mouth?

- at the side of the frenulum of the tongue
Where does the sublingual glands empty into the mouth?
As lots of different glands along the floor of the mouth

What is the role of the extrinsic mucles of the tongue?
Suspend the tongue in the oral cavity and function to change the position of the tongue during mastication, swallowing and speech
What are the 4 extrinsic mucles of the tongue and where do they each originate from?
Palatoglossus (palate -> tongue)
Styloglossus (styloid process > tongue)
Hyloglossus (hyoid bone > tongue)
Genioglossus (genial tubercle > tongue)

What is the main role of the intrinsic muscles of the tongue?
Modify the shape of the tongue during function
Which nerve gives motor supply all of the muscles of tongue, except palatoglossus?
CN XII - Hypoglossus
What functions does the hypoglossal nerve have?
Motor
What functions does the glossopharyngeal nerve have?
Special sensory, sensory, motor, visceral afferent and parasympathetic
What functions does the facial nerve have?
Special sensory, sensory, motor and parasympathetic
What functions does the maxillary branch of trigeminal nerve have?
Sensory
What functions does the mandibular branch of trigeminal nerve have?
Sensory and motor
Which layer does the constrictor (circular) muscles of the pharynx form and what is their role?
External layer; and constrict the pharynx, almost acting as a sphincter during swallowing
What are the 3 constrictor (circular muscles of the pharynx)?
Superior, middle and inferior

Which nerve supplies the constrictor muscles?
CN X - Vagus
Where do all of the constrictor muscles of the pharnyx insert?
All insert onto the midline raphe, which hangs from the occipital bone

What is the cricopharyngeus?
Acts as the Upper Oesophageal Sphincter.
Inferior part of inferior constrictor muscle where muscle fibres become narrower and more transverse. This acts as a junction for pharynx becomes the oesophagus and the larynx becomes the trachea
At what level is the cricopharyngeus?
C6
Which layer does the longitudunal muscles of the pharynx form and what is their role?
Inner layer; and they act to elevate the pharynx and larynx

Which nerves supply the longitudinal muscles?
All vagus (CN X) except for stylopharyngeus which is glossopharyngeal (CN IX)
What is the relevant anatomy and stages of swallowing?
- Close the lips to prevent drooling (orbicularis oris & cranial nerve VII)
- The tongue (cranial nerve XII) pushes the bolus posteriorly towards the oropharynx
- Sequentially contract the pharyngeal constrictor muscles (cranial nerve X) to push the bolus inferiorly towards the oesophagus
- At the same time the inner longitudinal layer of pharyngeal muscles (cranial nerves IX & X) contracts to raise the larynx, shortening the pharynx and closing off the laryngeal inlet to help prevent aspiration
- The bolus reaches the oesophagus

What types of sphincters are the 2 sphincters of the oesophagus?
UOS = anatomical
LOS = physiological
(Anatomical = have a localised and often circular muscle thickening to facilitate their action as a sphincter
Physiological = achieve their sphincteric action through muscle contraction around (extrinsic) or within (intrinsic) the structure)
Which factors help the LOS achieve its action as a sphincter?
- Contraction of diaphragm
- Intrabdominal pressure slightly higher than intragastric pressure
- Oblique angle at which oesophagus enters the cardia of stomach
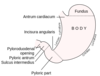
What is the z line?
Marks the Gastrooesophagea jucntion: Abrupt change in type of mucosa lining the wall from squamous epithelium of the oesophagus to glandulaer columnar epithelium of the stomach

What is the incisura angularis?
“angular notch” - a small anatomical notch on the lesser curvature of the stomach, near the pyloric end of the stomach
How long is the small intestine?
~ 7m
Which organs make up the foregut?
Oesophagus to mid-duodenum, liver, gallblader, splen and half of pancreas

Which organs make up the midgut?
Mid-duodenum to proximal 2/3rd of transverse colon; ½ pancreas

Which organs make up the hindgut?
Distal 1/3rd of transverse colon to proximal ½ of the anal canal

Which planes divide the abdomen into 9 quadrants?
Mid clavicular, subcostal and trans-tubercular planes

What is the peritoneum and what are its 2 layers?
A thin, transparent semi-permeable, serous membrane which lines the walls of the abdominopelvic cavity and organs. It consists of two layers which are continuous with each other; the parietal peritoneum (in contact with body wall) and the visceral peritoneum (in contact with abdominal organs)

What is peritoneal fluid and what are its roles?
A very small thin amount of fluid in the peritoneal cavity created by the serous lining.
Functions:
- It acts as a lubricant, enabling free movement of the abdominal viscera.
- The antibodies fight infection.
What are the paracolic gutters?
Spaces between the colon and the abdominal wall. Fluid moves upwards through these towards the diaphragm where it is re-absorbed into the blood stream.
What defines an organ as intraperitoneal?
Almost completely covered in peritoneum
What defines an organ as retroperitoneal?
Only its anterior surface is covered in peritoneum
Intraperitoneal or retroperitoneal: Stomach
Intraperitoneal
”SALTED SPRSS”
Intraperitoneal or retroperitoneal: Appendix ( + Caecum)
Intraperitoneal
”SALTED SPRSS”
Intraperitoneal or retroperitoneal: Liver
Intraperitoneal
”SALTED SPRSS”
Intraperitoneal or retroperitoneal: Transverse colon
Intraperitoneal
“SALTED SPRSS”
Intraperitoneal or retroperitoneal: Small intestine (jejunum and ileum)
Intrapertioneal
“SALTED SPRSS”
Intraperitoneal or retroperitoneal: Sigmoid colon
Intraperitoneal
“SALTED SPRSS”
Intraperitoneal or retroperitoneal: (O)esophagus (above thorax)
Intraperitoneal
“SALTED SPRSS”
Intraperitoneal or retroperitoneal: Dudodeunm (first part)
Intraperitoneal
“SALTED SPRSS”
Intraperitoneal or retroperitoneal: Spleen
Intraperitoneal
“SALTED SPRSS”
Intraperitoneal or retroperitoneal: Rectum (upper 1/3rd)
Intraperitoneal
“SALTED SPRSS”
Intraperitoneal or retroperitoneal: Pancreas (Tail)
Intraperitoneal
“SALTED SPRSS”
Intraperitoneal or retroperitoneal: Suprarenal (adrenal) glands
Retroperitoneal
“SAD PUCKER”
Intraperitoneal or retroperitoneal: Aorta & IVC
Retroperitoneal
“SAD PUCKER”
Intraperitoneal or retroperitoneal: Duodenum (Parts 2,3 & 4)
Retroperitoneal
“SAD PUCKER”
Intraperitoneal or retroperitoneal: Pancreas (Head, Neck and Body)
Retroperitoneal
“SAD PUCKER”
Intraperitoneal or retroperitoneal: Ureter
Retroperitoneal
“SAD PUCKER”
Intraperitoneal or retroperitoneal: Colon (ascending & descending)
Retroperitoneal
“SAD PUCKER”
Intraperitoneal or retroperitoneal: Kidneys
Retroperitonal
“SAD PUCKER”
Intraperitoneal or retroperitoneal: (O)esophagus - thoracic part
Retroperitoneal
“SAD PUCKER”
Intraperitoneal or retroperitoneal: Rectum (Lower 2/3rds)
Retroperitoneal
“SAD PUCKER”
What is a mesentety?
A mesentery is double layer of visceral peritoneum, where the visceral peritoneum wraps behind the organ to form a double layer.
It connects an intraperitoneal organ to the (usually) posterior abdominal wall. It provides a pathway for nerves, blood vessels and lymphatics from the body wall to the viscera.
What divides the abdomen into the greater and lesser sac?
The omenta (greater + lesser omenta)
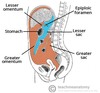
What is the omentum?
The omentum is a double layer of peritoneum that extends from the stomach and proximal part of the duodenum to other abdominal organs.
What is the greater omentum?
The greater omentum consists of four layers of peritoneum. It descends from the greater curvature of the stomach and proximal part of the duodenum, then folds back up and attaches to the anterior surface of the transverse colon.

What role does the greater omentum play in immunity?
Protective because it can migrate to sites of abdominal infection and stop the spread of intra-abdominal infection.
What is the lesser omentum?
The lesser omentum is considerably smaller and attaches from the lesser curvature of the stomach and the proximal part of the duodenum to the liver.

What 2 compartments is the greater sac divided into?
- Supracolic
- Infracolic
Divided by the transverse meso colon

What organs are found within the supracolic compartment of the greater sac?
Stomach, liver and spleen

What organs are found within the infracolic compartment of the greater sac?
Small intestine, ascending and descending colon

What is the omental foramen (aka epiploic foramen)?
The passage of communication, or foramen, between the greater sac (general cavity (of the abdomen)), and the lesser sac.

What lies at the free edge of the lesser omentum?
Portal triad (= hepatic artery (L), bile duct (R) (ant), and portal vein (post).

What pouches are formed by the peritoneum in the greater sac, in males and females?
In males: Rectovesical (between rectum and bladder)
In Females:
- Retro-uterine (pouch of douglas) (between rectum and uterus)
- Vesico-uterine (between bladder and uterus)

What is the Pouch of Douglas also known as?
Rectouterine pouch (in females)
During a paracentesis, where must the needle be placed and why?
The needle must be placed in the anterolateral abdominal wall lateral to the rectus sheath. This avoids the inferior epigastric artery which ascends in anterior abdominal wall (deep to rectus abdominis).

What is the clinical relevance of paracolic gutters?
They provide a route for the flow ascitic fluid, and for the spread of intraperitoneal infections and cancer metastases.
True or False: Visceral pain is hard to localise, while somatic pain is sharp and focal
True
True or False: Visceral pain tends to be sharp and stabby
Fasle, visceral pain tends to be dull/achey
True or False: Somatic pain tends to be sharp and stabby
True
In terms of nerve supply, is the visceral peritoneum classd as organ (visceral) or body wall (somatic)?
Organ (Visceral)
Which types of nerves are associated with the abdominal organs?
Autonomic motor nerves (sympathetic and parasympathetic)
Which types of nerves are associated with the abdominal walls?
- Somatic sensory nerves
- Somatic motor nerves
- Sympathetic nerve fibres
How do sympathetic nerve fibres get from the CNS to the abdominal organs (except adrenal glands)?
- Leave the spinal cord between levels T5 and L2
- Enter the sympathetic chains (bilaterally) but do not synapse
- Leave the sympathetic chains within abdominopelvic splanchnic nerves
- Synapse at prevertebral ganglia (celiac, superior mesenteric etc) located anterior to the aorta at the exit points of the major branches of the abdominal aorta
- Postsynaptic sympathetic nerve fibres pass from the prevertebral ganglia (celiac, superior mesenteric etc) onto the surface of the arterial branches leaving the abdominal aorta
- They take part in “periarterial plexuses” (around the arteries) with other nerve fibres (parasympathetic and visceral afferent) as they “hitch a ride” with the arteries, and their branches, towards the smooth muscle and glands of the organs

How do sympathetic nerves get to the adrenal glands from the CNS?
- Leave the spinal cord (T10-L1)
- Enter the abdominopelvic splanchnic nerves
- DO NOT synapse at prevertebral ganglia
- Are carried with periarterial plexuses to the adrenal gland
- Synapse directly onto cells

How do parasympathetic nerve fibres get from the CNS to the abdominal organs?
Vagus nerve:
- Presynaptic parasympathetic nerve fibres enter abdominal cavity on surface of the oesophagus (“vagal trunks”)
- Travel into the periarterial plexuses around the abdominal aorta
- Carried to the walls of the organs where they synapse in ganglia
- Supply parasympathetic nerve fibres to the GI tract + abdominal organs up to the distal end of the transverse colon
Pelvic Splanchnic Nerves:
- Arise from the anterior rami of the sacral spinal nerves S2-S4 and enter the sacral plexus
- They travel to their side’s corresponding inferior hypogastric plexus, located bilaterally on the walls of the rectum.
- From there they innervate the smooth muscle/glands of the descending colon to anal canal (pelvic and genital organs)
“S2, 3, 4 keeps your shit off the floor”
Where is pain from a source in the foregut likely to be felt?
Epigastric region
Where is pain from a source in the midgut likely to be felt?
Umbilical region
Where is pain from a source in the hindgut likely to be felt?
Pubic region
How do pain fibres of abdominal organs usually get back to the CNS?
Run alongside sympathetic fibres
Where do pain fibres of the foregut enter the spinal cord?
T6-9
Where do pain fibres of the midgut enter the spinal cord?
T8-12
Where do pain fibres of the hindgut enter the spinal cord?
T10-12
What is referred pain from abdominal organs?
Pain from these organs tends to be perceived by the patient in the dermatomes of the levels at which they enter the spinal cord (there is a little overlap)
Where is liver pain sometimes referred to and why?
Liver pain can be referred to the shoulder because it irritated the diaphragm, which is innervated by phrenic, the dermatome for C3,4,5 on the shoulder.

What are body wall nerves a continuation of?
Intervcostal nerves
What nerves are the somatic motor, somatic sensory and sympathetic nerve fibres supplying the structures of the abdominal part of the “body wall” conveyed within?
- The thoracoabdominal nerves:
- 7th-11th intercostal nerves
- The subcostal nerve (T12 anterior ramus)
- The iliohypogastric nerve (half of L1 anterior ramus)
- The ilioinguinal nerve (other half of L1 anterior ramus)
Why is pain from appendicitis initially felt as a dull, aching pain, but then becomes a sharper pain at a point in the right iliac fossa?
- The appendix is a midgut organ – usually located in the right iliac fossa
- Pain from midgut organs tends to be felt in the umbilical region because the visceral afferents from these organs enter the spinal cord between levels T8-T10 (appendix is T10 – umbilicus)
- As appendicitis worsens, the appendix will start to irritate the parietal peritoneum in the right iliac fossa, which lies anterior to it.
- The parietal peritoneum is part of the soma so is felt more focally
Where does break down of RBCs mainly occur?
Spleen
Around what level does the coelic trunk arise?
T12
Which artery supplies the foregut?
Coelic trunk
Which 3 arteries does the coeliac trunk branch into?
- Splenic artery
- Hepatic artery
- Left gastric artery

What does the common hepatic branch of the coeiliac trunk divide into?
- Proper hepatic a.
- > R & L hepatic a.
- > Right gastric a.
- > Cystic a.
- Gastroduodenal a.
- R. Gastro-omental (epiploic)
- Superior pancreaticoduodenal

What does the splenic a. branch of the coeliac trunk branch into?
- L. Gastro-omental (epiploic)
- Short gastrics
- Pancreatic branches
What does the L. Gastric a. branch of the coeliac trunk give rise to?
Oesophageal branches, before anastamosing with the R. gastric a.
Behind which ribs is the spleen?
Ribs 9-11
What are the 2 main blood supplies to the stomach?
- R & L gastric arteries
- Running along lesser curvature)
- R & L gastro-omental (epiploic)
- Running along greater curvature
Which ribs cover the liver?
Ribs 7-11
The liver can be described in ? anatomical segments and ? functional segments
4 anatomical segments (lobes) and 8 functional segments

Which is superior, the caudate or quadrate lobe of the liver?
Caudate lobe

True or False: Each of the functional segments of the liver has its own blood supply, venous drainage and bile drainage
True

Describe the venous drainage of the liver
Central veins of each lobule > sublobular veins > 3 main hepatic veins > IVC
What are the 4 ligaments associated with the liver?
- Falciform ligament (attaches the anterior surface of the liver to the anterior abdominal wall)
- Coronal ligament (R&L) - attach the superior surface of the liver to the diaphragm
- Triangular Ligament (R&L) - attach the superior surface of the liver to the diaphragm.
- Lesser Omentum

True or False: the IVC and hepatic veins have valves
Fasle, they dont - which is why portal hypertension and hepatlomegaly can occur
What makes up the intralobular portal triad?
- Branches of portal vein
- Branches of hepatic artery
- Branches of bile duct
Which blood supply to the liver provide the majority?
Portal vein (75%), while hepatic artery is 25%
What are the two recesses of the peritoneum in the greater sac relating to the liver?
- Hepatorenal recess (Morison’s pouch)
- Sub-phrenic recess

Describe the venous drainage to the liver
- Splenic vein drains the blood from the foregut
- Superior mesenteric vein drains blood from the midgut
- Inferior mesenteric vein drains blood from the hindgut
- These all drain to the portal vein which goes to the liver for first pass metabolism (cleaning)
What is the ligamentum teres/round ligament?
Remnant of the embryological umbilical vein

What is the arterial supply to the gallbladder?
The cystic duct (branch of the right hepatic artery)
Where would gallbladder pain be felt?
Early pain will be in the epigastric region as the gallbladder is a foregut organ and its visceral afferents enters spinal cord between T6 and T9.
Pain will also be felt in the right hypochondrium
Where do the common bile duct and major pancreatic duct meet?
CBD travels down to the 1st (superior) part of the duodenum to a groove on the posterior aspect of the pancrease where it meets the pancreatic duct

What do the CBD and pancreatic duct form together?
Ampulla of Vater
Where does the Ampulla of vater enter to duodenum?
At the 2nd part of the duodenum though the major duodenal papilla
What is Endoscopic Retrograde Cholangiopancreatography (ERCP) used to investigate?
Biliary tree and pancreas
What does a ERCP involve?
- Endoscope inserted through oral cavity, oesophagus, stomach and into duodenum
- Cannula placed into major duodenal papilla and radio-opaque dye injected back into biliary tree
What is the main mechanism for post (extra) hepatic jaundice?
Obstruction of the biliary tree e.g. gallstones or carcinoma of the head of the pancreas
What can the head of the pancreas be futher divided into?
Head proper and uncinate process

What are the blood supplies to the pancreas?
Mainly branches from splenic artery - Pancreatic branches.
The head is additionally supplied by the superior and inferior pancreaticoduodenal arteries due to its close relationship to the dudodenum, which are branches of the gastroduodenal and superior mesenteric arteries, respectively
What structures lie posterior to the head of the pancreas?
Aorta and IVC
What is the blood supply of the duodenum?
The superior and inferior pancreaticoduodenal arteries which are branches of the gastroduodenal and superior mesenteric arteries, respectively. (same as head of pancreas as they are closely related)
Where does the jejunum begin?
At the duodenaljejunal flexure
Where does the ileum end?
At the ileocaecal junction
What are the names of the folds of the mucosa in the jejunum?
Plicae circularis
What are some of the main differences betwee the jejunum and the ileum?
Plus the jejunum has plicae circularis, while the ileum is smoother
What gives the blood supply to the jejunum and ileum?
Superior mesenteric artery via jejunal and ileal arteries
(SMA supplies the midgut)
What is the venous drainage of the jejunum and ileum?
Jejunal and ileal veins > superior mesenteric vein > hepatic portal vein
Once absorbed into the enterocytes, where do the cylomicrons (fat) go?
Into specialised lymphatic vessels of the small intestine called lacteals. They then travel via the lymphatic system to eventually drain into the venous system at the thoracic duct (majority) or right lyphatic duct
True or False: Lymph vessels tend to lie alongside veins
False, they tend to lie alongside arteries
What are the main groups of lymph nodes draining the abdominal organs?
- Celiac (foregut organs)
- Superior mesenteric (midgut organs)
- Inferior mesenteric (hindgut organs)
- Lumbar (kidneys, posterior abdo wall, pelvis and lower limbs)
Where are the venous angles and what are they?
Junction between subclavian and internal jugular veins at both sides of the neck - they are the point where the thoracic duct returns lymph to the circulatory system.
What are the teniae coli?
3 longitudinal bands of thickened smooth muscle, running from the caecum to the sigmoid colon
What is the most common position of the appendix (in relation to the caecum)
Retrocaecal
Where is the appendix attached to the caecum?
Via the appendiceal orifice on posteromedial wall of caecum

Where is McBurney’s point and what does it indicate?
Found 1/3 of the way between right ASIS to umbilicus and represents the appendiceal orifice. Where tenderness is mostly felt in appendicitis.
Why is th sigmoid very mobile and what are the clinical implications of this?
It has a long mesentery (sigmoid mesocolon), however this means it can twist easily (volvulus)
Which artery serves the hindgut?
Inferior mesenteric artery
Which artery supplies the midgut?
Superior mesenteric artery
Which artery supplies the foregut?
Coeilic trunk
True or False: Aorta lies to the right of the IVC
False, the aorta lies to the left of the IVC
At what level does the abdominal arota bifurcate into the common iliacs?
L4/5
What are the branches of the SMA?
- Inferior pancreaticodudoenal a.
- Middle colic
- Right colic
- Ileocolic
- Appenicular
(which ileal and jejunal aa. coming off of these)

What are the branches of the IMA?
- Left colic a.
- Sigmoid colic a.
- Superior rectal a.
What is the name of the maina arterial anastomeses running between the SMA and IMA?
Marginal artery of Drummond
Where does the hindgut extend to?
The proximal half of the anal canal (the pectinate line).
Which artery supplies the remainder of the GI tract below the hindgut at the pectinate line?
Internal iliac a.
Which vein drains the foregut?
Splenic v.
Which vein drains the midgut?
Superor mesenteric v.
Which vein drains the hindgut?
Inferior mesenteric v.
What are the 3 clinically important sites of venous anastamoses between the systemic and portal venous systems?
- Distal end of the oesophagus
- Skin around umbilicus
- Rectum/anal canal

What are venous anastamoses between the systemic and portal venous systems?
Sites where the presence of small collateral veins means blood can flow both ways, either into the systemic or portal venous system. There are no valves in these veins
Where does the venous anastomsis at the distal end of the oesophagus drain?
Most inferior part drains to the hepatic portal vein and the most superior part drains to the azygous vein
Where does the venous anastomsis around the umblicus drain?
via inferior epigastric veins to the IVC
Where does the venous anastomsis around the rectum/anal canal?
- rectum and superior anal canal drains to inferior mesenteric vein
- most inferior part of GI tact drains to the internal iliac veins
Based on the venous anastamoses, which 3 clinical pathologies can occur from portal hypertension (increased blood pressure within the portal veins)?
More blood is forced into the collateral vessels at the anastomoses, resulting in:
- Oesophageal varices
- Caput medusae
- Rectal varices
All of which are dilated veins
What 4 anatomical factors are required for faecal continence?
- A “holding area” (the rectum) to store faeces until appropriate to defecate
- Normal visceral afferent nerve fibres to sense “fullness” of the rectum
- Storage area only works if it is controlled properly
- Functioning muscle sphincters around the distal end of the GI tract to appropriately contract, preventing defecation, and to relax, allowing defecation
- Normal cerebral function to control the appropriate time to defecate*
Why is the ileum known as the false pelvis?
As it is a pelvis structure but isn’t actually in the pelvic cavity
True or false: There is soemthign separating the pelvic cavity and the abdominal cavity above
False
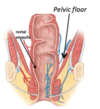
What does the pelvic cavity lie between?
Between pelvic inlet and pelvic floor
What is the pelvic floor made of?
Musclr, primarily the levator ani muscle
At what level is the rectosigmoid junction?
S3

At what level does the rectum become the anal canal?
At the tip of the coccyx, just before passing through the levator ani m.

What is everything below the pelvic floor classed as?
Perineum
Where does the rectal ampulla lie?
Immediately superior to the levator ani
What is the role of the rectal ampulla?
Its walls can relax to accommodate faecal material
What holes are found in the levator ani?
- Rectum
- Urogenital hiatus
Which muscles make up levator ani m.?
- Iliococcygeus: ileum > coccyx
- Pubococygeus: pubic bone > coccyx
- Puborectanlos: pubic bone > rectum

What is the nerve supply to the levator ani m.?
Branches of the sacral plexus (S3-4) & pudendal n. (S2, 3, 4)
“S2,3,4 Keeps your shit off the floor”
Why is the puborectalis m. (part of levator ani) particularly important in faecal continence?
Contraction of this muscle decreases the anorectal angle, acting like a sphincter
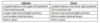
What are the main differences between the internal and external anal sphincters?

What kind of nervous supply do pelvic structures recieve?
They are body cavity (visceral) structures, so: sympathetic, parasympathetic and visceral afferent
What kind of nervous supply do perineal structures recieve?
They are body wall structures, so: somatic motor and somatic sensory
What is the pathway of the sympathetic innervation of the GI tract in the pelvic cavity (above the pectinate line)?
Sympathetic fibres from T12-L2: travel to inferior mesenteric ganglia, synapse, then travel via periarterial plexuses around branches of IMA
At what level does the visceral afferent and parasympathetic fibres arise from supplying the GI tract in the pelvic cavity (above the pectinate line)?
S2-4
How do the e visceral afferent and parasympathetic fibres supplying the GI tract in the pelvic cavity (above the pectinate line) get to the rectal wall?
Via pelvic splanchnic nerves
What is the effect of the sympathetic innervation of the GI tract in the pelvc cavity?
- Contraction of internal anal sphincter
- Inhibit peristalsis
What is the effect of the parasympathetic innervation on the GI tract in the pelvc cavity?
- Relaxation of internal anal sphincter
- Stimulate peristalsis
What is the role of the visceral afferent innervation on the GI tract in the pelvc cavity?
Sense stretch, indicating faeces building up in the rectal ampulla. Also sense ischaemia etc
What are the 2 main spinal cord levels for faecal continence?
- T12-L2 (Sympathetic innervation arises here
- S2-4 (Visceral afferent and parasympathetic innervation for pelvic cavity, and somatic motor innervation for perineum arise here)
Which nerve supplies the external anal sphincter?
Pudendal n.
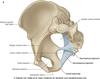
How does the pudendal n. exit the pelvis and then enter the perineum?
Exits the pelvis via the greater sciatic foramen, enters the perineum via the lesser sciatic foramen

What is the difference between the greater sciatic notch and greater sciatic foramen?
Greater sciatic notch when there is no ligaments, but when there are ligaments it creates a hole and is the greater sciatic foramen
What is the pectinate line?
Marks the junction between the part of the embryo which formed the GI tract (endoderm) and the part that formed the skin (ectoderm).
Above this line = visceral
Below this line = parietal (somatic)

What are the different arterial and nerve supplies, and venous and lymphatic drainages for below and above the pectinate line?

What are the main group of lymph nodes draining the pelvic organs?
- internal iliac (draining inferior pelvic structures)
- external iliac (draining lower limb, and more superior pelvic structures)
- interal/external iliac nodes > common iliac nodes > lumbar nodes

Which vein drains the hindgut?
Inferior mesenteric v.
Which vein drains l below the pectinate line?
Internal iliac v.
What sits around the anal canal ‘like a vascular cushion’?
Venous plexus
What is the difference between rectal varices and haemorrhoids?
Rectal varices are dilation of collateral vessels due to portal hypertension, while haemorrhoids are prolapses of the rectal venous plexuses (unrelated to portal hypertension)
What are the ischioanal fossae and what are their clinical importance?
Spaces located laterally to the anus containign fat and connective tissue which aid expansion of the anal canal during defecation.
Ischioanal abscesses can form when anal sinuses within the pectinate line which secrete mucous become blocked and infected.
What does a proctoscopy investigate?
The rectum
Where does the oesophagus pass in relation to the trachea, great vessels, heart and left main bronchus?
Behind
Which segment of the liver does the gallbladder lie anterior to?
Segment 5
Where is the mesentery of the jejunum and ileum attached to?
The mesentery of jejunum is attached to the left of aorta while the mesentery of ileum is attached to the right
What is the widest part of the colon?
Caecum (9cm)


