7 - Less Common Neurological Disorders Flashcards
(76 cards)
What is the presentation of Horner’s syndrome?
Triad of miosis, partial ptosis and anhydrosis
Due to interruption of the face’s sympathetic supply (oculosympathetic pathway)
Miosis leads to anisocoria

What is the aetiology of Horner’s syndrome?
Lesion anywhere from first to third order neurone
1st Order (Brainstem)
- Stroke (Medullary), MS, SOL, Syringomyelia (Bilateral), Cervical Cord trauma
2nd Order (Thoracic Outlet)
- Pancoast tumour, Thoracic outlet lesion, Brachial plexus injury, Thoracic aneurysm
3rd Order (Carotid)
- Carotid artery dissection, Cavernous sinus pathology, neck mass

How can you tell if a Horner’s syndrome is due to a carotid artery dissection?
Will be acute and painful!!!

What is the degree of anhidrosis in Horner’s syndrome?
Depends on the neurone affected

What investigations should you do if a patient has Horner’s syndrome?
Prompt evaluation for underlying cause
- CT angiography: look for carotid dissection as risk of stroke
- CT chest: look for Pancoast tumour
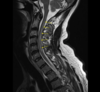
- MRI spine: spinal cord lesions
- MRI head: look for brainstem or cavernous sinus pathology

If a Horner’s disease is very subtle, what test can you do to confirm diagnosis?
- Cocaine Drops: no dilation if sympathetic chain involved
- Apraclonidine: dilation due to dennervation sensitivity
- Hydroxyamphetamine: Localises lesion, if doesn’t dilate it is 3rd order lesion. Stimulates release of noradrenlaine from post ganglionic neurones

How is Horner’s syndrome managed?
Treat underlying cause
- If acute and painful this is a neurological emergency as could be carotid artery dissection need to be sent to stroke unit (HASU)
What is the best way to do a neurological examination of a patient in a coma?

What pathology can arise at the cerebellopontine angle?

- Acoustic Neuroma/Vestibular Schwanomma (80%)
- Lipoma
- AV malformations
- Haemangioma

What is an acoustic neuroma? (vestibular schawnomma)
Benign cerebellopontine angle tumour of the schwann cells of the vestibular nerve
Usually unilateral and grow very slowly (1-2mm/year)
Bilateral in Neurofibromatosis Type 2

How do acoustic neuromas typically present?
- Unilateral sensorineural hearing loss
- Vertigo
- Tinnitus
- Facial nerve palsy
- As they grow larger they can cause ipsilateral V, VI, IX and X enrve palsies and ipsilateral cerebellar signs. Can also have signs of increased ICP

How are acoustic neuromas investigated and managed?
Ix
- Serial gadolinium-enhanced MRI
- Audiogram
Mx
- Surveillance with serial MRIs every 6/12 for 2 years then 2 years then every 5 years
- Microsurgery
- Radiotherapy

What are some of the risks with microsurgery for an acoustic neuroma?
- CSF leak and meningitis.
- Cerebellar injury.
- Stroke.
- Epilepsy.
- Facial paralysis (V and VII)
- Hearing loss (IX)
- Balance impairment (IX)
- Persistent headache
What is subacute combined degeneration of the spinal cord?
Vit B12 deficiency causes degeneration of the dorsal columns and the corticospinal tracts
Peripheral neuropathy (loss of fine touch, 2-point discrimination, proprioception, and vibration sensations) but pain and temperature fine
Combination of LMN and UMN signs
How does subacute combined degeneration of the cord typically present?
Signs and symptoms
- Symmetrical pins and needles, numbness progressing to weakness
- Visual impairment
- Change in mental state
- Bilateral spastic paralysis
- Sensations diminished (pressure, vibration, proprioception)

What signs may you elicit on examination of a patient with subacute combined degeneration of the cord?
- +ve Romberg sign (e.g falls in low light and shower)
- + Babinski sign (UMN)
- Absent ankle jerk reflex (LMN)
- Brisk knee jerk reflex (UMN)
- Unsteady ataxic gait
- Spastic paralysis
- Loss of vibration sensation

What other symptoms can B12 deficiency cause apart from subacute combined degeneration of the cord?
- Optic atrophy
- Anaemia
- Cognitive impairment

How is subacute combined degeneration of the cord investigated and managed?

Ix
- Serum B12 and Folate levels
- FBC
- MRI spine T2
Mx
- B12 replacement either IM, SC or sublingual with hydroxycobalamin
- Folate replacement
- Can take 3-6 months to improve, sometimes deficit is irreversible

What is a cavernous sinus syndrome?
How can it present?
Any pathology of the cavernous sinus leads to certain symptoms to paralysis of CN’s in the sinus
Causes: Cavernous Sinus Thrombosis, Cavernous Sinus Tumours, Carotid Cavernous Aneurysms
Presentation: Ophthalmoplegia, proptosis, ocular and conjunctival congestion, trigeminal sensory loss and Horner’s syndrome.

What are some causes of a cavernous sinus thrombosis and how does it present?
Causes: spread of infection from sinuses or boil/folliculitis on face
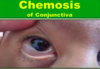
Presentation: headache, chemosis, oedema of eyelids, proptosis, painful opthalmoplegia, fever
How is a cavernous sinus thrombosis investigated?
- Bloods: thrombophillia screen
- Non-contrast CT: hyperdensity in the affected sinus.
- CT venogram: look for filling defect (‘ empty delta sign’)
- MRI-T2: look for thrombus

How is a cavernous sinus thrombosis treated?
- IV antibiotics
- LMWH
- Corticosteroids for swelling
- Surgical drainage of any pus
How do intracranial venous thrombi present in general?
- Presentation is variable but headache, confusion/drowsiness, impaired vision, and nausea/vomiting.
- Seizures, reduced consciousness, focal neurological deficitis, cranial nerve palsies, and papilloedema

What are some causes and some differential diagnoses for an intracranial venous thrombosis?
Causes of hypercoagulable state: Pregnancy, COCP, Trauma, Local infection, Tumours, Malignancy, dehydration
Differentials:
- SAH
- Meningitis
- Encephalitis
- Stroke
- Intracranial abscess















































