14 - Skin Infections and Infestations Flashcards
What is impetigo caused by and how can it be classified?
Superficial bacterial infection caused by S.Aureus (most common) or S.Pyogenes that has managed to get into a break in the skin e.g cut, eczema
- Bullous (Always S.Aureus and can infect intact skin)
- Non-bullous

What are some risk factors for impetigo?
- Eczema
- Scabies
- Surgical wound
- Chicken pox
- Insect bite
How does non-bullous impetigo present?
- Usually around the nose or the mouth but can affect other sites
- Starts as pink macule, then goes to vesicle then forms a honey crust
- Resolves on 2-4weeks with no scarring

How does bullous impetigo present?
- Small vesicles that turn into flaccid transparent bullae
- Very painful and itchy
- Eventually burst and form honey crust
- Always due to S.Aureus
- Heal with no scarring
- Usually in neonate - 2 years

What is the pathophysiology of bullous impetigo?
S.Aureus release epidermolytic enzymes that break down the proteins that hold the skin cells together
How should you manage both types of impetigo?
Non-Bullous
- Localised: first try topical antiseptic Hydrogen Peroxide 1% cream then add topical fusidic acid abx
- Widespread/Systemically unwell: oral flucloxacillin or topical fusidic acid
- Inform that it is contagious so good hygeine and keep off school until crusted over or until taken abx for 48 hrs
Bullous
- Take swabs of vesicles to get bacteria and sensitivities
- Oral flucloxacillin
- Isolate as very contagioius
- Can turn to SSSS so consider admission

What are some complications of impetigo?
- Cellulitis if the infection gets deeper in the skin
- Sepsis
- Scarring (rare)
- Post streptococcal glomerulonephritis
- Staphylococcus scalded skin syndrome
- Scarlet fever

What is folliculitis and what does it look like?
- Inflammed hair follicle due to any cause
- Tender red spot often with surface pustule
- Acne is a variant of folliculitis

What are some of the different causes of folliculitis?
Infection: S.Aureus (if in deep part of follicle forms boil), HSV, P.Aeruginosa, Candida Albicans, Scabies
Irritation due to regrowing hairs: wax and shaving
Contact: moisturisers, plasters, steroid creams,
Immunosuppression
Inflammatory Disease: Lichen Planus, SLE, Acne

How do you treat bacterial folliculitis?
- Hygeine
- Oral or topical antibiotics
- Antiseptic cream
What is the difference between cellulitis and erysipelas?

- Cellulitis involves deep subcutaneous tissue and is less defined
- Erysipelas is superficial cellulitis. Affects the dermis and upper subcutaneous tissue and has a well defined, red raised border

What are some risk factors for developing cellulitis or erysipelas?
- Immunosuppression
- Wounds
- Leg ulcers
- Toeweb intertrigo
- Minor skin injury
What bacteria causes cellulitis and erysipelas?
Cellulitis: S.Aureus or S.Pyogenes
Erysipelas: Usually S.Pyogenes
What is the clinical presentation of erysipelas/cellulitis?
- Signs of inflammation: swelling, erythema, warmth, pain
- Systemically unwell with fever, malaise or rigors, especially erysipelas
- Lymphadenopathy
How is erysipelas/cellulitis managed?
- Oral flucloxacillin or benzylpenicillin. (Erythromycin if allergic)
- Rest
- Elevate affected area
- Analgesia
- Sterile dressing

What are the complications of cellulitis?
- Local necrosis
- Abscess
- Septicaemia
How does herpes simplex present?
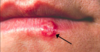
- Grouped painful vesicles on erythematous base
- Recurrent genital (HSV2) and peri-oral (HSV1)
- Often preceded by burning/itching and flu-like symptoms like sore throat and lymphadenopathy

What are some complications of oral herpes simplex virus?

- Eczema herpeticum
- Corneal ulceration
- Erythema multiforme
- Pneumonia
- Encephalitis

How is oral herpes simplex treated?
SUPPORTIVE GENERAL MEASURES
- Analgesia for pain and fever
- Topical aciclovir not recommended
- Avoid trigger factors e.g stress, sunlight
- If severe and recurrent can give topical aciclovir
- Advice on reducing transmission
How is genital herpes simplex treated?
- Oral aciclovir for 5-10 days within 5 days of onset
- Self-care measures (for example topical anaesthetic, increasing fluid intake to produce dilute urine)
- Abstain from sex until lesions have cleared
- Prophylaxis aciclovir every day for 6-12 months if 6 or more attacks in a year
- Refer to specialist if pregnant or immunocompromised

What are some complications of genital herpes simplex?
- Superinfection of lesions e.g candida
- Autonomic neuropathy leading to urinary retention
- Aseptic meningitis
- Neonatal herpes simplex virus
What is the difference between varicella zoster and herpes zoster?
Varicella Zoster - Chicken Pox
Herpes Zoster - Above reactivates after lying dormant in dorsal root ganglion to produce Shingles
How does the rash in chicken pox evolve?
- Patient becomes symptomatic 10-21 days after innoculation and develops a prodromal fever, malaise, flu-like symptoms
- 24 hours later there is a generalised maculopapular rash that turns into a generalied pruritic vesicular rash
Macules –> Papules –> Vesicles –> Crust –> Hypopigmentation

How long are people with chicken pox contagious for?
- 48 hours before rash until the lesions have crusted over (usually after 5 days)
- Spread by direct contact or through infected droplets from cough or sneeze






















































