6 - Common Neurological Disorders 3 Flashcards
What is the pathophysiology of MS?
Chronic autoimmune inflammatory disease of CNS
Demyelination of neurones in CNS (oligodendrocytes damaged) by immune cells. Leads to inflammation and production of plaques (scars).
Plaques are axonal loss so irreversible neurological damage. The deficits depend on where the plaques are
Lesions are disseminated in time and place

What is the epidemiology of MS and some risk factors?

More common in women, up north and middle aged

Risk Factors
- Genetic
- Viral infections (EBV)
- High geographic latitude
- Lack of sun exposure/Vit D
Where are the common sites for plaques in MS?
- Optic nerves: affects 40% during course of disease. Presenting demyelinating event in 20%.
- Spinal cord: affects 50-75% during course of disease
- Brainstem: intranuclear ophthalmoplegia
- Cerebellum: ataxia and gait disturbance
- Juxtacortical white matter (near the cerebral cortex)
- Periventricular white matter (near the ventricular system)

What are the different classifications of MS?
Relapsing-remitting (RRMS):
- 90% of cases
- Exacerbations then remission. May remit to normal level in early disease but then residual damage with each relapse
Primary progressive (PPMS):
- 10-15%
- Sustained progression of disease severity from onset
- No remission but can be times where disease not active
Secondary progressive (SPMS):
- 50% of RRMS will develop this in 15 years
- Gradual sustained progression with periods of relapse but no remission
Clinically Isolated Syndrome
- First episode of suspected MS
- No previous episode of demyelination
- Some never go on to have another episode

What are some clinical manifestations of MS?
Depends on site of plaques, usually monosymptomatic at a time
Visual: optic neuritis, INO, abducens palsy
Motor & coordination: transverse myelitis, cerebellar syndrome, Bell’s, Horner’s, Limb weakness, Incontinence
Sensory & autonomic: LHermitte’s Phenomenon (flexion of neck), Paraesthesia, Pain, Heat sensitivity (Uhthoff phenomenon), Sexual dysfunction, Bladder & bowel dysfunction, Trigeminal neuralgia
Cognitive & psychological: depression and fatigue

What is internuclear opthalmoplegia?
- Disorder of conjugate lateral gaze due to demyelination of the medial longitudinal fasciculus
- MLF connects abducens nucleus complex with contralateral oculomotor nucleus
- If left INO, when looking to the right, the right eye will abduct but the left will remain central (failure in adduction). There is also nystagmus

What is transverse myelitis and cerebellar syndrome that can be a manifestation of MS?

Transverse myelitis: focal inflammation within the spine. Characterised by sensory and motor symptoms below the level of the lesion (e.g. paraesthesia, weakness). Bladder/bowel involvement may be present and usually there is a sensory level that corresponds to the level of the lesion.
Must exclude compressive pathology in first instance (i.e. metastatic cord compression).
Cerebellar syndrome: disease of the cerebellum, which manifests with ataxia, slurred speech, intension tremor, nystagmus, vertigo and clumsiness.

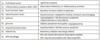
What are 6 MS eponyms?

How is the diagnosis of MS made?
Clincal + MRI for lesion dessiminated in time and space
Revised Mcdonald Criteria
Early treatment reduces relapses and disability so refer to neurology ASA disseminated

What is the definition of a single MS attack and why is an MRI used to aid diagnosis?
- Attack must last >24h with or without recovery and >30d between attacks
- MRI used to look for plaques to prove dissemination in time
- MRI can also prove dissemination in time by gadolinium-enhancing and nonenhancing lesions at any time, or by a new gadolinium-enhancing lesion(s) on follow-up MRI

What are some differentials for MS?
Depends on site of plaque

What is Neuromyelitis optica (Devic’s disease)?
What anti-bodies is it associated with?
MS variant with transverse myelitis (loss of motor, sensory, autonomic, reflex and sphincters below level of lesion), and bilateral optic neuritis
Associated with Anti-Aquaporin 4 antibodies

What investigations should you do if you suspect MS?
- MRI
- LP (Immunoelectrophoresis of CSF): CSF-specific IgG oligoclonal bands present in CSF but not in serum
- Visual evoked response (VER): measuring electrical activity via transducer over occipital cortex in response to light stimulus. Not for acute but can show previous asymptomatic optic neuritis
- Antibody levels: AQP4 and myelin oligodendrocyte glycoprotein (MOG) associated Neuromyelitis Optica not MS

What bloods should you take if you suspect MS and why?
What are the principles of management in MS?
- General Care
- Managing acute relapses
- Disease modifying therapies
What general care measures are put in place for people with MS?
- Avoid stress
- Spasticity: baclofen or gabapentin, physio
- Tremor: botuline A toxin
- Bladder dysfunction: self catheterisation if residual >100ml, tolterodine if residual <100ml
- Depression: SSRI, CBT
- Fatigue: exercise, CBT
- Neuropathic Pain: amitriptyline, gabapentin or pregabalin.
How is an acute relapse in MS managed?
- PO methylprednisolone 0.5 g daily for five days, OR Intravenous methylprednisolone 1 g daily for 3-5 days
- PPI
- Only use steroids twice a year as don’t alter course of disease just help symptoms

What are some disease modifying treatments used in MS?

Aim to decrease the number of relapses and slow disease progression
RRMS (1ST Line):
- Natalizumab
- Teriflunomide
- Ocrelizumab
- Beta-interferon

When should people with MS be offered disease modifying drugs?

What is the prognosis with MS?
Highly variable
- Disease type: RRMS better prognosis than PPMS. Most patients with RRMS eventually develop SPMS.
- Recovery following first attack: incomplete recovery worse prognosis
- Clinical manifestations at onset: motor symptoms (poor prognosis). sensory symptoms, optic neuritis (favourable prognosis).
- Pregnancy: protective during pregnancy. Increased risk of relapse in postpartum period.
- Imaging: lesion load and cerebral atrophy linked to prognosis

How can a relapse of MS be recognised?

What is the main finding on examination with optic neuritis?
- Pain on eye movement
- RAPD
How may pregnancy affect MS?
- Progression halts and no relapses whilst pregnant
- High rate of relapse 3-6months after birth
What are the clinical features of an essential tremor?
Autosomal dominant movement disorder: younger age of onset if inherited
- Postural or kinetic: made worse on arms outstretched
- Usually affects upper limbs, head, lower limbs, face, trunk
- Tremor amplitude increases with time, and patients experience difficulty in writing, eating, holding objects and doing fine motor tasks, dressing, and speaking













































