18 - Dermatology Common Drugs Flashcards
What are some of the different formulations of emollients and what are they prescribed for?
Formulations
- Aqueous cream,
- Ointment
- Liquid paraffin
- White soft paraffin in equal parts (50:50)
Indications
- Rehydrate skin and re-establish the surface lipid layer
- Useful for dry, scaling conditions and as soap substitutes

What are some of the adverse effects of emollients?
- Irritant or allergic reactions due to perfumes or preservatives
- Flammable if contain paraffin
- Pump dispensers minimise the risk of bacterial contamination; if using a pot, use a clean spoon / spatula every time to reduce risk

What is the potency ladder with topical steroids?

What are some side effects of topical steroids for the treatment of eczema?

- Skin atrophy (thinning)
- Telangiectasia
- Striae
- Acne
- Perioral dermatitis
- Allergic contact dermatitis
- May mask / cause / exacerbate skin infections

What are some of the side effects of long term oral steroids use for eczema?
- Cushing’s syndrome
- Immunosuppression
- Hypertension
- Diabetes
- Osteoporosis (give bone-protection alongside)
- Cataracts
- Steroid-induced psychosis
- Fluid retention

Why should you avoid oral corticosteroids in psoriasis?
- Risk of unstable disease
- Can develop into pustular psoriasis
What are some of the side effects of anti-histamines used in eczema?
Sedating Antihistamines e.g Chlorphenamine
- Sedation
- Anticholinergic effects (e.g. dry mouth, blurred vision, urinary retention, constipation, acute angle closure glaucoma)

How is dermatitis herpatiformis diagnosed?
Skin biopsy

What is the summary of treatment for eczema? (ladder)

Treated as maintenance and flare ups

Why are topical calcineurin inhibitors used in the treatment of atopic eczema, how do they work and what are some examples of these?
- Steroid sparing agents when steroids are not controlling symptoms but the risk of side effects outweighs the benefits
- Suppress overactivity of T-cells
- Tacrolimus Ointment (Protopic) if severe or Pimecrolimus cream (Elidel) if moderate

What are some side effects and contraindications of topical calcineurin inhibitors?
Side Effects

- Skin irritation (e.g stinging/burning)
- Photosensitivity
- Increased risk of skin cancer and lymphoma
Contraindications
- Do not use near eyes or mucous membranes
- Do not use in infected areas or people susceptible to infections, e.g HSV, as increased risk of developing infection in area used
- Immunodeficiency
What are some of the side effects of oral aciclovir?
- GI upset
- Raised liver enzymes
- Reversible neurological reactions
- Haematological disorders
What is the aim of prescribing anti-virals in shingles?
Reduce the incidence of post-herpetic neuralgia
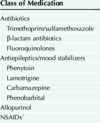
What antibiotic class has a risk of TEN?
Penicillins
How do you explain to a patient how to apply topical calcineurin inhibitors?
Applied thinly twice a day when active eczema starts and then when cleared continued as a maintenance only twice a week.
Do not apply steroid cream to the same areas
Tacrolimus: Apply 2 hours after emollient
Pimecrolimus: Apply to dry skin then add emollient
Methotrexate is an immunosuppressant that can be used for eczema and psoriasis. How does it work and how is it taken?
What should be co-prescribed with it?
Dihydrofolate reductase inhibitor, leading to nitric oxide synthase uncoupling and increased sensitivity of T cells to apoptosis, thereby diminishing immune responses
Only take ONCE A WEEK with folic acid co-prescribed
Can take 8-12 weeks to take effect
What is some pre-treatment screening and monitoring after starting that needs to be done with Methotrexate?
Pre-treatment: Pregnancy test, FBC, U&Es, LFTs, Start contraception, ?CXR, ?Viral Serology
Monitoring (every 1-2 weeks initially then every 2-3 months): FBC, U+Es, LFTs
Report any signs of infection e.g sore throat

What are some side effects and contraindications for the use of Methotrexate in Psoriasis and Eczema?
Side Effects:
- Bone marrow suppression (need to report any infection symptoms)
- GI upset
- Mouth ulcers
- Liver and Lung fibrosis (rare but can develop if also got RA)
Contraindications
- Immunodeficiency syndromes
- Active infections
- Taking trimethoprim can increase risk of bone-marrow suppression

What are some pieces of advice to give patients when starting methotrexate?
- Avoid live vaccines
- Highly teratogenic so both men and women should use contraception whilst using and for 6 months after stopping
- At increased risk of infections. If develop dry cough, diarrhoea, fever or any symptoms need to report as could be toxicity and bone-marrow suppression
- Take care when using with trimethoprim as bone marrow suppression risk
- Avoid alcohol due to liver damage risk
- Need folic acid co-prescribed

What patients taking methotrexate are at an increased risk of developing hepatotoxicity (liver fibrosis)?
- Obesity
- Diabetes
- Alcohol
- Higher dose of MTX
Azathioprine is a steroid-sparing immunosuppressant that can be used off-licence for atopic eczema. What is some pre-treatment screening that needs to be done and monitoring that needs to be done after starting this drug?
Pre-treatment: TPMT levels as if low then risk of bone marrow suppression
Monitoring (at least every 3 months): FBCs, LFTs, U+Es
Takes 4-6 weeks to show effect so not useful for acute flares like ciclosporin is

What are some side effects and contraindications for the use of Azathioprine?

Side effects:
- Nausea, Diarrhoea, Loss of appetitie
- Pancreatitis
- Bone marrow suppression
- Increased risk of skin cancers and lymphomas
- ‘Flu-Like Symptoms’ due to allergy
Contraindications:
- Low levels of TPMT
- Do not have live vaccines

Ciclosporin is a steroid-sparing immunosuppressant used in eczema and psoriasis. How does this drug work and why is this immunosuppressant sometimes preferred?
Inhibition of the production of cytokines involved in the regulation of T-cell activation. Calcineurin Inhibitor
- Faster acting
- Not as teratogenic so not so bad if fall pregnant
- Can still drink alcohol

What monitoring needs to be done whilst on ciclosporin?
Pretreatment: Need U+Es and blood pressure taken twice before starting
Monitoring:
- BP, U+Es and Serum Creatinine every 3/12
- LFTs
- Investigate any persistent lymphadenopathy
- Blood lipids before and after 1/12