6 - Asthma and COPD Flashcards
(54 cards)
What is the pathophysiology of asthma?

- Chronic reversible airway obstruction that responds to bronchodilators
- Increased airway responsiveness and narrowing to stimuli
- Airway narrowing: bronchial muscle contraction, mucosal swelling due to mast cells and basophils releasing mediators, increased mucus production

What are the signs and symptoms of asthma?
Symptoms: Intermittent dyspnea, wheeze, nocturnal cough, sputum
Signs: tachypnea, audible wheeze, hyperinflated chest

What are some differentials for a wheeze apart from asthma>

If a patient presents with asthmatic like symptoms, what are some questions you need to ask in the history?
- Triggers: e.g cold air, exercise, pets, smoking, NSAIDs
- Diurnal variation: worse at night?
- Exercise tolerance
- Disturbed sleep?
- Other atopic diseases?
- Job?
- Days per week off school or work?

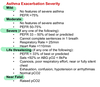
When is asthma classified as mild, moderate, severe, life threatening and near fatal?
What does PEF depend on?
- Age
- Gender
- Height

What is the emergency management for acute asthma?
- Aim for sats of 94-98% with oxygen. If <92% ABG needed
- 5mg Salbutamol NEB and repeat after 15 minutes
- 40mg oral prednisolone or IV hydrocortisone

How do you initially diagnose asthma?

What investigations should you do if a patient is having an acute episode of asthma?
- PEF
- Sputum culture and ?Blood culture
- FBC, U+Es, CRP
- ABG
- CXR to exclude infection or pneumonthorax
What investigations can you do for a patient with chronic asthma?
- PEF monitoring (diurnal variation with >20% variability on >3days in 2 weeks)
- CXR may have hyperinflation
- Spirometry (obstructive pattern, ratio<70% with bronchodilator reversibility)
- Skin prick test to identify allergens
- Metacholine or Histamine challenge
What is the criteria that needs to be fulfilled for a safe discharge after an asthma exacerbation?

What factor means a patient with asthma will be responsive to steroids?
Eosinophillia
Apart from asthma, what are some diseases that cause eosinophilia?

What are some common asthma triggers?
- Smoking
- URTI
- Pollen
- Pets
- Exercise
- Cold air
- Aspirin and beta blockers
- Stress
- Occupational exposures

What is the general management of asthma in a primary care setting?
- Avoid triggers
- Stop smoking
- PEF monitoring
- Self management plan for emergencies
- BTS pharmacological management
- Treat correct inhaler technique

What is the pharmocological management of asthma using the BTS guidelines?
Start at step most appropriate to severity, moving up or down. Can move down after >3months of control
1st: SABA reliever when needed
2nd: Add low dose ICS
3rd: Add LABA with the ICS or LTRA or oral theophylline
4th: Increase ICS
5th: Add regular oral prednisolone with specialist input

What signifies poor asthma control?
- 3 or more days a week with symptoms
- 2 or more days a week with use of a rescue SABA inhaler
- 1 or more nights a week with awakening due to asthma
Need to check inhaler technique, inhaler adherance, smoking and self management plan
How do beta-agnonists help asthmatics and what are the side effects of these?
Relax bronchial smooth muscle within minutes by increasing cAMP
SE: tachyarrhythmias, hypokalaemia, tremor, paradoxical bronchospasm

How do inhaled corticosteroids help asthma and what are the side effects of these?
Act over days to decrease bronchial mucosal inflammation
Used inhaled to minimise systemic effects
SE: usual steroid side effects, oral thrush so rinse mouth adter use

How does aminophylline help asthmatics and what are some side effects of this?
Metabolised to theophylline. Inhibits phosphodiesterase so decreases bronchoconstriction.
Used as prophylaxis at night
SE: arrhythmias, GI upsets, seizures
Monitoring: theophylline levels, ECG monitoring

How do LTRA help asthmatics?
Block the effects of leukotrienes by antagonising the CystLT1 receptor

What is the definiton of COPD and what are the causes of it?
Progressive airflow obstruction that is not reversible
Chronic bronchitis + Emphysema
Causes: smoking, alpha antitrypsin deficiency, industrial exposure e.g soot

What is the definiton of chronic bronchitis and emphysema?
Chronic Bronchitis: Cough and sputum production on most days for 3 months in 2 successive years
Emphysema: Enlarged air spaces with destruction of alveolar walls and loss of elasticity. Visualised on CT and diagnosed histologically

What is the pathophysiology of COPD?
- Mucous gland hyperplasia
- Loss of cilia function
- Emphysema
- Chronic inflammation and fibrosis of small airways

























