16 - Infectious Diseases including Travel Infections Flashcards
What is antimicrobial stewardship?
Process of persuading prescribers to use evidence-based prescribing to prevent antibiotic overuse and therefore prevent antibiotic resistance
Preserves future effectiveness of antibiotics

What are some of the steps in antimicrobial stewardship for every prescriber?
- Prescribe the most appropriate dose, for the shortest time to be effective and the most appropriate route, with the narrowest spectrum abx
- Take microbiological samples before prescribing antibiotic and review prescription when get the results
- Consider delayed prescribing for self-limiting conditions
- Explain to patients why antibiotics might do them more harm than good
- Avoid repeat antibiotic prescriptions within 6 months

What scenarios do the AMS team review?
- Set local antimicrobial guidelines and review regularly
- Review patient safety events
- Ensure antibiotic pack sizes are appropriate for course length

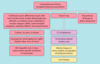
What is the 10 point approach to a patient with a suspected infection?
- What is the evidence for the infection?
- How severe is it?
- Any patient factors to consider?
- Which organ system is infected?
- What is the likely microorganism?
- Which anti-microbial therapy is best?
- Which route of administration is best?
- Any other treatment needed?
- Any risk of transmitting to others?
- How do we follow up and achieve discharge?

What are some causes of immunosuppression?
- HIV
- Immunosuppressive drugs e.g steroids, chemo
- Primary immunodeficiency
- Age
- Malnutrition
- Malignancy
- Asplenism

What do you need to consider with vaccinating immunosuppressed patients?
- Cannot have live vaccines as can develop disseminated disease
- Try to give inactivated vacines two weeks before immunosuppressive therapy as poor antibody response when immunosuppressed
- Need to be offered flu and pneumovax
How are nosocomial infections managed?
- Identify: e.g screening of MRSA
- Protect: isolate multiantibiotic resistant microbes, highly transmissable diseases or high risk groups
- Treat: using local guidelines
- Prevent: modify risk factors e.g improve nutrition, remove catheters, clean hands
What are the preventative measures used in hospital to stop infection spreading?
- Hand washing/gelling (wash for C.Diff)
- Bare below elbows and tie back hair
- Scrubs in highly infectous areas
- PPE
- Aseptic techniques
- Clean environment

What is the difference between standard isolation and respiratory isolation?
Respiratory:
- Negative pressure room if AGP or room with door closed at all times if NAGP
- Respiratory precautions sign on door
- Gown, gloves, face shield and mask/FFP3
- Dispose of waste in the room
- Hand hygeine after glove removal
- Limit movement to other departments and visitors

What are the most common organisms causing infection in the following systems and what antibiotics are used to treat them:
- Skin/Soft tissue
- MSK
- Respiratory

- Skin: Staph Aureus, Coagulase negative Staph (S.Epidermidis), Group A Strep (S.Pyogenes), MRSA
- MSK: same as above, Pseudomonas for diabetic foot, TB)
- Respiratory: S.Pneumoniae, H. Influenzae, Legionella, Mycoplasma, Rhinovirus, Adenovirus, Influenza

What are the most common organisms causing infection in the gastrointestinal system and what antibiotics are used to treat them?

Diarrhoea: Rotavirus, Adenovirus, Campylobacter, C.Diff, Salmonella
Peritonitis: Enterobacteriacae

What are the most common organisms causing infection in the following systems and what antibiotics are used to treat them:
- Genitourinary Tract
- CNS
- Endocarditis

GU: Enterobacteriacae, P.Aeruginosa, N.Gonnorrhea, C.Trachomatis
CNS: S.Pneumonia, N.Meningitidis, HSV, TB, Listeria (>55 or immunocompromised)
Endocarditis: Strep Viridans, Enterococci, S.Aureus, MRSA

What are the most common organisms causing infection in the following systems and what antibiotics are used to treat them:
- Line infections
- Hospital acquired
- Sepsis


What is the gram stain of the following:
- S.Aureus
- S.Epidermidis
- C.Diff
- S.Pneumoniae
- S.Pyigenes
- H.Pylori
- Salmonella
- Campylobacter
- Pseudomonas Aeruginosa
- H.Influenzae

What are some examples of common parasites?
- Protozoa: malaria, entamoeba histolytica, giardia lamblia
- Hyatid disease
- Schistosomiasis

What are some examples of notifiable diseases?
- Mumps
- Measles
- Food poisoning
- Malaria
- SARS
- TB
- Tetanus
- Whooping cough

What are some bacteria that are encapsulated?
- N.Meningitidis
- H.Influenzae
- S.Pneumoniae
These are destroyed in spleen so sickle cell or after splenectomy need prophylactic vaccinations as higher risk of infection from these
How can antibiotics be grouped by their actions?
Affect:
- Cell wall synthesis
- Nucleic Acid synthesis
- Protein synthesis

What are the two different categories of antibiotic resistance and give some examples of each?
Intrinsic: due to structural characteristics e.g vancomycin cannot outer membrane of gram negative bacteria
Acquired: bacteria have evolved via mutation due to selection pressue from antibiotic use (including agricultural antibiotics)

What are some examples of antibiotics that inhibit cell wall synthesis?
Beta lactams: penicillins, carbapenems, cephalosporins
Non beta lactams: glycopeptides

What is Tazocin?
Piperacillin + Tazobactam
(beta lactam + betalactamase inhibitor)
What are the indications for the following antibiotics:
- Benzylpenicillin (Penicillin G)
- Phenoxymethylpenicillin (Penicillin V)
- Co-Amoxiclav
- Tazocin
- Flucloxacillin
- Vancomycin
- Cetriaxone
Penicillin G: usually gram positive such as streptococci (chest, endocarditis, cellulitis), meningococcus
Penicillin V: prophylaxis after splenectomy, rheumatic heart disease
Co-Amoxiclav: chest, pyelonephritis, cellulitis, bone
Tazocin: broad spectrum gram positive and negative, neutropenic sepsis, nosocomial infection
Flucloxacillin: staphylococcus e.g skin, bone, post viral pneumonia
Vancomycin: complicated gram positive e.g MRSA, oral for C.Diff
Ceftriaxone: meningococcus
What are some examples of antibiotics that inhibit protein synthesis?
- Aminoglycosides
- Macrolides
- Tetracyclines
- Fusidic acid
- Chloramphenicol

What are the indications for the following antibiotics and what are some side effects:
- Gentamicin/Tobramycin
- Azithromycin/Clarithromycin/Erythromycin
- Tetracycline/Doxycycline