12 - T&O Spine, Hip and Thigh Flashcards
What are the different types of fractured neck of femur and what are the causes?
NOF is a fracture anywhere from subcapital region of femoral head to 5cm below the lesser trochanter
High energy: RTA in the young
Low energy: Fall from standing height in elderly
Think pathological fractures if no trauma
Intra or Extracapsular

Why is the mortality with NOF fractures so high in the first year?
Those with poor mobility before fracture, high age and co-morbidities at higher risk
Patient tends to die from complications such as pnuemonia etc
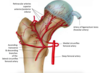
What is the blood supply to the femoral head?

Retrograde from MCFA from deep femoral artery from external iliac
Some blood from ligamentum arteriosum but only enough blood to supply head in children
Displaced intracapsular fractures can disrupt blood supply causing avascular necrosis
Extracapsular fractures can be classified as intertrochanteric and subtrochanteric. What are the different classifications of intracapsular fractures?
Garden Classification
I and II are non-displaced
III and IV are displaced

How will a #NOF present?
- Pain in groin, thigh or referred to knee
- Inability to weight bear
- Shortened and externally rotated
- Pain on pin rolling and axial loading
- Unable to do straight leg raise

What are some investigations that need to be done if you suspect a #NOF?
- AP and Lateral Hip and Pelvis X-Ray
- Full neurovascular exam of the limp
- FBC, U+Es, CK if long lie for rhabdo
- Group and Save
- Urine dip, CXR and ECG in elderly

How is a #NOF managed?
- A to E
- Opioid or regional anaesthesia (fascia-iliaca block)
- Surgical (see image) with urgent physio and mobilisation after
If displaced intracapsular needs arthroplasty (full not hemi if active but will dislocate more) due to risk of AVN. If non-displaced can try screws to see if will repair without AVN as metal work has a life span

What are some post op complications with #NOFs?
Immediate: pain, bleeding, leg length discrepancies, neurovascular damage
Long term: joint dislocation, aseptic loosening, peri-prostethic fracture, deep/prosthetic joint infection, mortality, AVN, malunion-nonunion
Make sure to get early physio, ortho-geriatricians and OTs involved

Why should you not use NSAIDs in fracture healing?
Need inflammatory process for bone healing so will prolong healing time
What is the Nottingham Hip Score?
Tool used by surgeons to work out the 30 day mortality risk of a patient following a #NOF
High lactate is also a marker of mortality in #NOF

What are some of the symptoms and risk factors of hip osteoarthritis?
Symptoms
- Dull pain in groin or buttock that is exacerbated by movement and relieved by rest
- Stiffness and crepitus worse after resting
- May have antalgic gait but if severe may have fixed flexion defority and Trendelenbery gait
- Passive movement painful and reduced range of motion

What are some differential diagnoses for hip OA?
- Trochanteric bursitis
- Gluteus medius tendinopathy
- Sciatica
- Femoral neck fracture

What investigations are done to diagnose and classify hip OA?
- X-ray Pelvis to show at least 2 typical OA features
- MRI gold standard if not sure from X-ray
- Can use WOMAC tool to monitor disease progression. Looks at pain, stiffness and function

How is hip OA managed?
Conservative:
- NSAIDs for pain
- Weight loss, exercise, smoking cessation
- Physiotherapy
Surgical (if above doesn’t work)
- Hip hemi/arthroplasty

What are some complications with a hip arthroplasty?
- Thromboembolic disease
- Bleeding
- Dislocation
- Infection
- Loosening of prosthesis
- Leg length discrepancy
- Need for revision hip arhtroplasty after 15-20 years

What is the pathophysiology of a femoral neck shaft fracture?
- Often due to high energy trauma
- Associated with neurovascular injury
- Large blood loss (up to 1.5L) as highly vascularised due to haemopoetic role. Supplied by penetrating branches of profunda femoris
- Often transverse fracture in proximal femur

How does a femoral shaft fracture present and how is it classified?
- Pain in thigh and/or hip/knee
- Inability to weight bear
- Assess skin as may be open or threatened (tethered, white, non-blanching)
- Proximal fragment in flexion and external rotation (iliopsoas and gluteus medius/minimus)
- Full neurovascular exam needed
- May have signs of hypovolemia

What investigations are done when a femoral shaft fracture is suspected?
- Routine urgent bloods including coagulation and G+S
- Plain Film Radiograph AP and Lateral of femur, hip, knee
- CT scan if polyfracture or concurrent #NOF suspected

How is a fractured femoral shaft managed before surgery?
Initial
- ATLS protocol with A to E and appropriate fluid resus
- Adequate pain relief (opioid or regional block)
- If open fracture abx prophylaxis and photography
- Immediate reduction and immobilisation using in-line traction so haematoma forms in right place
- If too many co-morbidities or undisplaced femoral shaft fracture then long-leg cast and no surgery

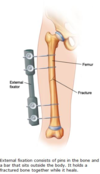
How is a femoral shaft fracture managed surgically after traction splinting?
Within 24-48 hours needs antegrade intramedullary nail (retrograde if hip replacement)
If unstable polytrauma or open fracture then external fixation until intramedullary nail can be done
Early mobilisation after nailing decreases complications. If bilateral fractures more pulmonary complications

When should you not use traction splinting for a fracture?
- Hip or pelvic fracture
- Supracondylar fracture
- Fractures of ankle or foot
- Partial amputation
What are some complications of a femoral shaft fracture?
- Neurovascular injury (pudendal or femoral nerve)
- Mal-union, delayed union non-union (higher risk if smoker or post op NSAID use)
- Infection (especially open)
- Fat embolism
- Hip flexor or knee extensor weakness

What is the pathophysiology and risk factors for a quadriceps tendon rupture?
Rupture usually occurs at site of insertion on superior patella. Mechanism is following sudden excessive loading of quadriceps e.g landing from a jump
Risk factors: increasing age (>40), CKD, Diabetes, RA, medication like corticosteroids and fluoroquinolones
Differentials: patella tendon rupture, patella fracture, femoral shaft fracture

How will a quadriceps tendon rupture present?
Symptoms
- May hear a pop or feel a tearing sensation then…
- Pain in anterior knee or thigh
- Difficult to weight bear
Examination
- Localised swelling
- Tender palpable defect at top of patella
- If complete tear inability to straight leg raise or extend knee