10/22- Pathology Case Studies Flashcards
Case 1)
- 23-year-old man
- Mild diarrhea for a month that was resolved without treatment and now presents with diarrhea after a month of normal bowel movement
- Stool exam and culture: negative
- Colonoscopy
What is your diagnosis?
A. Crohn’s disease
B. Ulcerative colitis
C. More information is required for definitive diagnosis
D. Indeterminate
E. Infectious colitis

See biopsy of terminal ileum
- See crypt abscess (filled with neutrophils)
- Dying part on the right
- Top is mucin/goblet-depleted
What is your diagnosis?
A. Crohn’s disease
B. Ulcerative colitis
C. More information is required for definitive diagnosis
D. Indeterminate
E. Infectious colitis
This is just acute ileitis
- May be a part of Crohn’s disease
- In case of pancolitis in ulcerative colitis: backwash ileitis
What is the most common cause of acute ileitis?
Medications
- The entire colon and rectum are edematous and friable
- Multiple biopsies
What is the best pathologic diagnosis?
A. Inflammatory bowel disease, consistent with Crohn’s disease
B. Chronic active colitis
C. CMV colitis
D. Inflammatory bowel disease, consistent with ulcerative colitis
E. Amebiasis

A. Inflammatory bowel disease, consistent with Crohn’s disease
B. Chronic active colitis
C. CMV colitis
D. Inflammatory bowel disease, consistent with ulcerative colitis
E. Amebiasis
On histology, can see:
- Neutrophils invading crypts (cryptitis)
- Distortion of architecture
- Will see the same think in Crohn’s and ulcerative colitis, but absence of other things on endoscopy means just chronic active colitis at this point
Case 2)
- 26-year-old woman
- Abdominal wall mass
- Three months, enlarging
- 10 cm mass on physical exam
- Biopsy followed by excision
What is this?

[not testable]
Desmoid tumor (abdominal fibromatosis)
- Clonal fibroblastic proliferation of deep soft tissue with infiltrative growth
- Locally aggressive (local recurrence, but no metastases)
- May be familial (associated with Gardner’s syndrome/familial adenomatous polyposis (FAP) syndrome or familial desmoid syndrome) or related to trauma
- Arise from abdominal wall of women of reproductive age
- During or after pregnancy
- Treatment: excision with wide margins
Case 2 cont’d)
- 2 yrs later…
- Presents with weakness, fatigue and exercise intolerance for 2 years!
- Hb: 5.8 and MCV 53
- No menorrhagia
- Diarrhea for the past 2 years; 5-6 times noted blood
Bloodwork:
- Low Hb
- Low MCV
- Low MCHC
- High RDW
More lab results:
- Iron panel, ferritin level, vitamin B12, folate, and reticulocyte
- IgA transglutaminase, IgA endomysial Ab and IgA antigliadin (tests for Celiac) are negative
- Fecal WBC, fecal ova, and parasite and fecal fat stain are negative
- Iron: low
- TIBC: normal
- Iron saturation: 4%
- Ferritin: low
- Folic acid: high
- Vitamin B12: normal
- Retic count: high
What do the lab results mean?
A. Iron deficiency anemia with a component of anemia of chronic disease
B. Megaloblastic anemia
C. Celiac disease
D. Steatorrhea
E. Parasite in bowel
A. Iron deficiency anemia with a component of anemia of chronic disease
B. Megaloblastic anemia
C. Celiac disease
D. Steatorrhea
E. Parasite in bowel
What are lab results of:
- Iron deficiency anemia
- Anemia of chronic disease
- The patient
[don’t have to memorize]

Which one of the tests should not have bene ordered? Why?
A. Iron panel
B. Vitamin B12 and folate
C. Reticulocyte
D. Celiac antibodies
E. Fecal WBC, fecal ova and parasite and fecal fat stain
A. Iron panel
B. Vitamin B12 and folate
C. Reticulocyte
D. Celiac antibodies
E. Fecal WBC, fecal ova and parasite and fecal fat stain
- The RBCs here are small; Vitamin B12 and folate contribute to megaloblastic anemia
- If pt comes in with anemia, iron panel is the first thing ordered (#1 anemia = iron deficiency)
- Reticulocyte count is to test bone marrow function
What is seen here on her upper endoscopy?

Esophagus
- Multiple white plaques in mid and
lower esophagus
- Brushings
- Stomach
- Multiple sessile polyps in body and fundus
- Biopsy
Duodenum normal
What is seen here on her colonoscopy?

- Many polyps, indicative of familial adenomatous polyposis (FAP)
- Sigmoid mass
What is seen here?

Gastric polyp
What is seen here?

Rectosigmoid polyp
- Tubular type
This is the biopsy of the sigmoid mass.
What is the correct diagnosis? Cause?
A .Stomach polyp has dysplasia
B. Rectosigmoid polyp is a tubulovillous adenoma
C. Sigmoid mass is adenocarcinoma
D. A and B
E. A, B and C

A .Stomach polyp has dysplasia
B. Rectosigmoid polyp is a tubulovillous adenoma
C. Sigmoid mass is adenocarcinoma
D. A and B
E. A, B and C
- AFP with desmoid tumor
- Multiple polyps in GIT and one in sigmoid is cancerous now
- Chronic bleeding and anemia
- Histology shows tubulovillous type
What do you recommend as the next step?
A. Proctoscopy to check for whether mass is low enough to benefit from neoadjuvant chemo, XRT and check for relative rectal sparing surgery
B. Oncology consult
C. Genetic counseling
D. A and B
E. A, B and C
A. Proctoscopy to check for whether mass is low enough to benefit from neoadjuvant chemo, XRT and check for relative rectal sparing surgery
B. Oncology consult
C. Genetic counseling
D. A and B
E. A, B and C
Describe FAP (Familial Adenomatous Polyposis)
- Aka
- Genetic mutation
- Inheritance pattern
- Prognosis
- Features of colonoscopy
- Familial polyposis coli
- Due to defect in APC gene at 5q21
- Autosomal dominant trait with high penetrance
- 100% progress to colonic adenocarcinoma, often in teens, most by thirties
- Patients have >100 colon polyps (usually thousands), beginning as teenagers; most are tubular adenomas
What are common symptoms of FAP? Diagnostic criteria?
- Polyps in stomach and small intestine
- Desmoid tumors in 10-25%
Diagnostic criteria:
- 100+ colorectal polyps
- Germ line mutation in APC gene
- Family history of APC and
- At least one of epidermoid cyst, osteoma or desmoid tumor
What is seen here?

Familial Adenomatous Polyposis
What is thet treatment for FAP?
- Prophylactic colectomy by 20-25 yo and screening of relatives
- May also develop carcinoma of thyroid gland, gallbladder, and adrenal gland
Case 3)
- 61-year-old woman
- Epigastric discomfort, loss of appetite and a 10 lb. weight loss in the last four months
- A few days prior to seeking medical attention noticed a faint yellow tinge to her skin and sclera
- Past medical history: smoking for many years
PE:
- A woman appearing her stated age and in no apparent distress
- Moderate tenderness in both epigastrium and right upper quadrant
- Pale skin with a yellow tinge, also noted in her buccal mucosa and sclerae
Relevant labs:
- Low/normal Hb
- Low Hct
- High total bili
- High alkaline phosphatase
- Normal amylase nad lipase
- CA19-9 high
Imaging:
- Ultrasound
- Stones in the gallbladder
- Slight dilatation of the common bile duct and main pancreatic duct
- No masses in the pancreas
- CT scan
- Slight increased size of the head of the pancreas
What are the possible causes of the mild jaundice in this patient?
A. A gallstone
B. Edema and fibrosis associated with chronic pancreatitis
C. A neoplasm of the head of the pancreas
D. A neoplasm in the pancreatic duct
E. All of the above
What are you thinking from the lab results?
A. A gallstone
B. Edema and fibrosis associated with chronic pancreatitis
C. A neoplasm of the head of the pancreas
D. A neoplasm in the pancreatic duct
E. All of the above
Lab results:
- Confirm obstruction of the bile flow (total bilirubin and alkaline phosphatase)
- Raise the possibility of pancreatic malignancy (slightly-to-moderately elevated CA 19-9)
- Normal amylase and lipase do not rule out chronic pancreatitis
What do the following tumor markers indicate:
- CA19-9
- AFP
CA19-9
- Blood test for pancreas
- Less in hepatobiliary Ca
AFP (alpha fetoprotein)
- Liver cancer
- Testicular cancer
What should be the next step?
A. Evaluation of respectability of the mass by CT scan
B. Endoscopic-guided fine needle aspiration (EUS-FNA) of the head of pancreas and/or a large lymph node
C. Exploratory laparotomy and intraoperative consultation with pathology
D. A and B
E. B and C
A. Evaluation of respectability of the mass by CT scan
B. Endoscopic-guided fine needle aspiration (EUS-FNA) of the head of pancreas and/or a large lymph node
C. Exploratory laparotomy and intraoperative consultation with pathology
D. A and B
E. B and C
What is a Whipple procedure?
- A major operation with considerable morbidity and mortality
- A few consider it unjustified taking into account the overall dismal prognosis of pancreatic cancer
- Most regard this procedure as the only opportunity to cure early neoplasia of the head of the pancreas or of the ampulla of Vater
Aka pancreaticoduodenectomy
- Remove duodenum, pancreas head, and common bile duct; sometimes also a little stomach
What are pros/cons of EUS-guided FNA of pancreas?
Cost effective
Minimally invasive
- Confirm or exclude malignancy
- Prevent unnecessary surgery in patients with inoperable tumor
- Neoadjuvant radiation and chemo in potentially resectable malignancies
Identification of local metastases or invasion
Simultaneous diagnosis and staging: managzment plan
How accurate is EUS-guided FNA of pancreas?
- False sampling vs. false positive
- Sensitivity: 75-94%
- Specificity: 100%
- Adequacy check at the time of performance improves accuracy
- False sampling: sampling or interpretation errors
- False positive: less common; over-interpretation of reactive atypia in pancreatitis
On EUS-guided FNA, saw pancreas head mass but no large LNs
- If large LN seen with positive FNA, no surgery
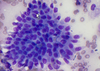
What is seen on this FNA sample?

Malignancy
- Normal ductal cells are honeycombed
- Malignant cells seen on right

What is seen here?
Normal ductal cells
- Honeycomb pattern with no overlapping
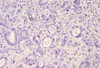
What is seen here?

Malignant cells with cells (nuclei) that have different shapes and sizes, and overlapping
What is seen here?

Malignant cells with cells (nuclei) that have different shapes and sizes, and overlapping
Patient is diagnosed with malignancy: pancreatic adenocarcinoma based on:
- Neoplastic cells overlapping with high N:C ratio, irregular nuclear borders, and prominent nucleoli
What is the next step?
Whipple procedure
What is seen here?

Benign pancreas
- Pancreatitc acini
- Langerhans island

What is seen here?
Adenocarcinoma
What is seen here?
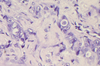
Adenocarcinoma
What are key features/characteristics of pancreatic adenocarcinoma?
- Marked pleomorphism; very different ranges of cell sizes
- Perineural invasion, also into lymphatics
What is seen here?
Perineural invasion (pancreatic carcinoma?)
What is seen here?

Lymphatic invasion (pancreatic carcinoma?)
Specimen descriptin:
- Both the distal pancreatic resection margin and the common bile duct resection margin are negative for malignancy, as are all nine regional lymph nodes recovered from the specimen
What is the prognosis of the patient?
A. Excellent
B. Very good
C.Good
D. Reasonable
E. Poor
A. Excellent
B. Very good
C.Good
D. Reasonable
E. Poor
Prognosis of pancreatic adenocarcinoma
- Very poor prognosis when discovered after clinical presentation
- Most patients have regional spread to lymph nodes or distant metastases at the time of diagnosis
- If left untreated, one-year survival < 10%
- Overall five-year survival for pancreatic cancer: 4%
In the U.S., the five-year survival of carcinoma of the head of the pancreas after the Whipple’s procedure is up to 21%, in selected series
Which has better prognosis?
A. Adenocarcinoma of head of pancreas
B. Adenocarcinoma of tail of pancreas
C. Adenocarcinoma of ampulla of Vater
D. They are all the same
E. A and B
A. Adenocarcinoma of head of pancreas
B. Adenocarcinoma of tail of pancreas- worst, because it presents even later
C. Adenocarcinoma of ampulla of Vater- due to its location; causes symptoms much earlier (will present earlier)
D. They are all the same
E. A and B
Ampulla > Head > Tail
Case 4)
- 49 yo woman
- Abdominal pain
- CT scan: pancreatic mass
What is the diagnosis (staining positive for CD56)? What histological features help you make the diagnosis?
A. Adenocarcinoma
B. Endocrine neoplasm
C. Squamous cell carcinoma
D. Poorly differentiated carcinoma
E. Metastasis

A. Adenocarcinoma
B. Endocrine neoplasm
C. Squamous cell carcinoma
D. Poorly differentiated carcinoma
E. Metastasis
Histologic features:
- High nuclear to cytoplasmic ratio
- Salt and pepper chromatin
- The neoplastic cells are CD56 positive.
- Cytomorphology and immunostaining pattern are consistent with an endocrine pancreas neoplasm
Evaluation of malignancy awaits surgical excision, since evaluation of lymphovascular invasion and invasion into adjacent organs cannot be evaluated on cytology
What is the most common malignant tumor in (non-cirrhotic) liver?
A. Hepatocellular carcinoma
B. Metastatic colon carcinoma
C. Cholangiocarcinoma
D. Metastatic lung carcinoma
E. Metastatic breast carcinoma
A. Hepatocellular carcinoma
B. Metastatic colon carcinoma
C. Cholangiocarcinoma
D. Metastatic lung carcinoma
E. Metastatic breast carcinoma
- In a non-cirrhotic patient, metastatic neoplasms are the most common hepatic malignancy; colon = most common
- If pt has cirrhosis, most common is HCC
Case 5)
- 58-year-old man
- Abdominal pain
- High alkaline phosphatase
- CT showed a liver mass
- Liver biopsy of mass
What do you see in this portion of liver biopsy?
A. Chronic inflammation
B. Steatosis
C. Ballooning degeneration
D. Mallory hyaline body
E. Cholestasis

A. Chronic inflammation
B. Steatosis
C. Ballooning degeneration
D. Mallory hyaline body
E. Cholestasis
- NOT ballooning degeneration because these are clean
What is seen here?
A. Benign liver
B. Tumor
C. Amebiasis
D. Necrosis
E. Red blood cells

A. Benign liver
B. Tumor
C. Amebiasis
D. Necrosis
E. Red blood cells
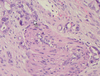
Based on this additional histology…
What is the probable diagnosis?
A. Metastatic adenocarcinoma, colon
B. Metastatic adenocarcinoma, lung
C. Metastatic adenocarcinoma, breast
D. Metastatic adenocarcinoma, bladder
E. Hepatocellular carcinoma

A. Metastatic adenocarcinoma, colon
B. Metastatic adenocarcinoma, lung
C. Metastatic adenocarcinoma, breast
D. Metastatic adenocarcinoma, bladder
E. Hepatocellular carcinoma
Can recognize this is adenocarcinoma (forming glands)
- Necrosis inside
If this is the first presentation of this patient how do you confirm the diagnosis?
A. CT of abdomen
B. MRI of abdomen
C. Biopsy of colonic mass
D. Performance of immunohistochemical stains
E. Start chemotherapy and evaluate the mass after a few cycles
A. CT of abdomen
B. MRI of abdomen
C. Biopsy of colonic mass
D. Performance of immunohistochemical stains
E. Start chemotherapy and evaluate the mass after a few cycles
Immunostaining results:
- CK7 negative
- CK20 positive
- CDX2 positive
Does this immunostaingin pattern confirm your diagnosis?
A. Yes, since this pattern is seen in > 60% of the cases
B. Yes, since CK7 – and CK20+ is seen in about 70% of cases
C. Yes, since the CDX2 positivity is seen in about 88% of the cases
D. Yes, because of all of the above reasons and the typical cytomorphology
E. No, since there is no specific staining pattern for this entity
A. Yes, since this pattern is seen in > 60% of the cases
B. Yes, since CK7 – and CK20+ is seen in about 70% of cases
C. Yes, since the CDX2 positivity is seen in about 88% of the cases
D. Yes, because of all of the above reasons and the typical cytomorphology
E. No, since there is no specific staining pattern for this entity
If the patient has a history of colon adenocarcinoma, what is the cheapest way to diagnose this metastasis?
A. Compare this biopsy with the tissue from the original tumor
B. Use the immunohistochemical stain that the previous biopsy showed positivity
C. Use cytogenetic studies on both specimens
D. A and B
E. B and C
A. Compare this biopsy with the tissue from the original tumor
B. Use the immunohistochemical stain that the previous biopsy showed positivity
C. Use cytogenetic studies on both specimens
D. A and B
E. B and C
Case 6)
- 81-year-old woman
- History of hypertension
- ED with diarrhea for 2 weeks
- Associated with nausea and abdominal pain in lower quadrants
- Hepatitis panel and HIV negative
- Lipase elevated
- Admitted with suspicion for pancreatitis
Which diagnosis can explain symptoms and CT scan findings?
A. A benign multifocal tumor
B. Infection
C. Metastasis
D. Drug reaction
E. B and C
A. A benign multifocal tumor
B. Infection
C. Metastasis
D. Drug reaction
E. B and C
CT findings:
- Multiple (at least 20) hepatic lesion, largest 5x4 cm suspicious for metastatic lesion
- Jejunum is thickened and perforated
Biopsy is performed. Results shown below, including immunohistochemical positivity for chromogranin and synaptophysin.
What is the diagnosis?
A. Metastatic colon adenocarcinoma
B. Metastatic lung adenocarcinoma
C. Hepatocellular carcinoma
D. (Neuro)endocrine neoplasm
E. Infection with Entamoeba histolytica

A. Metastatic colon adenocarcinoma
B. Metastatic lung adenocarcinoma
C. Hepatocellular carcinoma
D. (Neuro)endocrine neoplasm
E. Infection with Entamoeba histolytica
Diagnosis via: liver, US-guided core needle biopsies of mass
- Pay special attention to chromatin pattern
- Neuroendocrine tumor
- Grade 2
- 2 mitoses/10HPF
What is the cause of diarrhea in this patient?
A. Entamoeba histolytica
B. Her age
C. Her primary neoplasm
D. Metastatic neuroendocrine neoplasm to the liver
E. Reaction to a medication
A. Entamoeba histolytica
B. Her age
C. Her primary neoplasm
D. Metastatic neuroendocrine neoplasm to the liver
E. Reaction to a medication
What is carcinoid syndrome?
Symptoms secondary to carcinoid tumor
- Flushing, diarrhea and less commonly heart failure and bronchoconstriction
Caused by enodgenous secretion of serotonin and kallikrein
Vasoactive substances from the tumors enter the systemic circulation escaping hepatic degradation
- When carcinoid tumors metastasize to liver


