10/14- Large Intestine, Pathology Flashcards
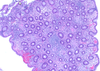
T/F: There are villi and crypts in the colon
False
- Colon has crypts but no villi
- Crypts look like racked test tubes and reach muscularis mucosa

What is seen here?

Cross section of previous pic
- Crypts are equally spaced with mild lymphoplasmacytic infiltrate and capillaries
Describe Entamoeba histolytica
- Transmission
- Prevalence
- Characteristics of agent
- Reproduction
- Location
- Disease
- Amebiasis
- Fecal-oral transmission
- Esp developing countries (500M)
- E. histolytica cysts has a chitin wall and four nuclei
- Resistant to gastric acid: pass through the stomach
- Cysts colonize the epithelial surface of the colon and release trophozoites
- Most frequently in cecum and ascending colon
Results in:
- Dysentery
- Liver abscess
How does Entamoeba histolytica cause dysentery?
- Amebae attach to the colonic epithelium… apoptosis
- Invade crypts and burrow into lamina propria
- Neutrophils -> tissue damage
- Flask-shaped ulcer
How to identify Entamoeba histolytica histologially?
May be difficult; amebae are similar to macrophages
How does Entamoeba histolytica cause liver abscess?
- Parasites may penetrate splanchnic vessels
- Embolize to liver -> abscesses (40% of patients with amebic dysentery)
What is seen here?

Scanning EM of intestinal amebiasis
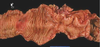
What is seen here?

Intestinal specimen from pt with acute amebic colitis
What is seen here?
Entamoeba histolytica cause liver abscess?
What is the clinical presentation of Entamoeba histolytica?
- Abdominal pain, bloody diarrhea and weight loss
- Occasionally, acute necrotizing colitis and megacolon
- Significant mortality
How to treat Entamoeba histolytica?
(Obligate fermenters of glucose)
The most effective treatment: metronidazole
- Inhibits enzyme pyruvate oxidoreductase
What is Pseudomembranous colitis?
What commonly causes it?
Antibiotic-associated colitis or antibiotic-associated diarrhea
- Diarrhea during or after a course of antibiotic therapy
- Usually caused by Clostridium difficile
- Salmonella, C. perfringens type A
- Staphylococcus aureus
Describe the pathogenesis of Pseudomembranous colitis
- Disruption of the normal colonic flora by antibiotics allows C. difficile overgrowth
- Most commonly: third-generation cephalosporins
- Predisposing factor: immunosuppression
- Toxins:
- Ribosylation of small GTPases, such as Rho
- Disruption of the epithelial cytoskeleton, tight junction barrier loss, cytokine release and apoptosis
What are risk factors for Pseudomembranous colitis?
- Advanced age
- Hospitalization
- Antibiotic treatment
Up to 30% of hospitalized adults are colonized with C. difficile (tenfold greater than the general population)
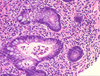
What is seen here?

Psuedomembranes (C. difficile) in Pseudomembranous colitis
What is seen here?

Pseudomembranous colitis
- “Volcano eruption” of neutrophils and dead cells is common
- Increased chronic inflammatory cells in lamina propria

What is seen here?

Pseudomembranous colitis
- Higher magnification of volcano eruption of neutrophils and dead cells
What is the clinical presentation of Pseudomembranous colitis?
How is it diagnosed?
- Fever, leukocytosis
- Abdominal pain, cramps,
- Hypoalbuminemia
- Watery diarrhea and dehydration
+/- fecal leukocytes and occult blood
Diagnosis: C. difficile toxin and characteristic histopathology
Treatment for Pseudomembranous colitis (C. difficile)?
- Metronidazole
- Vancomycin
What is Inflammatory bowel disease?
What does it include? (Important!)
Chronic condition due to inappropriate mucosal immune activation
Two disorders: Crohn disease and ulcerative colitis
- Ulcerative colitis: a severe ulcerating inflammatory disease limited to colon and rectum involving mucosa and submucosa
- Crohn disease: regional enteritis, involves any area of the GI tract and typically transmural
Pictoral difference between Crohn’s disease and ulcerative colitis? (Important!)
Crohn’s:
- Skip lesions (not continuous)
- Transumural inflammation,ulcerations, fissures
Ulcerative colitis:
- Continuous colonic involvement beginning in the rectum
- Pseudopolyps and ulcers

Describe the epidemiology of IBD
- More in females
- Common in teens/early 20s
- Most common in Caucasians in Western industrialized nations
- 3-5x more in eastern European (Ashkenazi) Jews
- Geographic distribution is highly variable
- Most common in N America, N Europe, and Australia
Pathogenesis of IBD (picture)

Describe the pathogenesis of IBD
In genetically susceptible host, release of TNF and other immune-mediated signals epithelia
- > increase tight junction permeability
- > further increases in the flux of luminal material
- Self-amplifying cycle to initiate
A variety of factors are associated with disease for unknown reasons
- Appendicitis: reduced risk of developing UC
- Tobacco modifies IBD epidemiology: increase risk of Crohn while reduce risk of UC
Describe the morphology of Crohn’s disease:
- Location
- Continous/not
- Common features
Affects all the GI tract
- Most common in ileum, ileocecal valve, and cecum
- 40% limited to the small intestine
- 30% involvement of small intestine and colon
- Multiple, separate, sharply delineated areas of disease; skip lesions are characteristic
- Stricture common
What is seen here?
Skip lesions in Crohn’s
- Normal mucosa separated by inflamed mucosa

What is seen microscopically in Crohn’s disease?
- Cryptitis and crypt abscess with crypt destruction
- Ulcer with abrupt transition between ulcerated and adjacent normal mucosa
- Distortion of architecture due to repeated crypt destruction and regeneration
- Epithelial metaplasia
- Architectural and metaplastic changes may persist even in inactive disease
- Noncaseating granuloma: hallmark of Crohn (35% of cases)
- Absence of granuloma does not rule out Crohn
What is seen here?
Colon with distortion of architecture (Crohn’s disease):
- Crypts not equally spaced
What is seen here?

Crohn’s disease
- Increased chronic inflammatory cells in lamina propria
- Granulomas

What is seen here?

Crohn’s disease:
- Cryptitis: neutrophils in the crypt epithelial cells
- Granuloma in lamina propria: epithelioid macrophages surrounded by lymphocyte

What is seen here?
Crohn’s disease:
- Cryptitis: neutrophils int he crypt epithelial cells
- Increased chronic inflammatory cells in lamina propria
- Crypts abscess: neutrophils inside the crypt

Describe ulcerative colitis
- Location
- Extra-intestinal manifestations
- Prognosis
- Limited to colon and rectum
Common extra-intestinal manifestations of ulcerative colitis overlap with those of Crohn disease
- Migratory polyarthritis
- Sacroiliitis
- Ankylosing spondylitis
- Uveitis
- Skin lesions
- Pericholangitis
- Primary sclerosing cholangitis (2.5% to 7.5%)
Prognosis depends on severity of active disease and disease duration
What is seen here?

Ulcerative colitis
- Riable edematous mucosa
- Pancolitis and its response to treatment.
A: only scattered fragments of mucosa are left,
C-D: over time mucosa is being regenerated
Describe the morphology of ulcerative colitis
- Location
- Skip lesions?
- Extent of disease
- Gross features
- Complications
- Always involve rectum; then proximal extension
- No skip lesions
- Pancolitis: disease of the entire colon
- Small intestine normal, although mild mucosal inflammation of the distal ileum, backwash ileitis, may be present in severe cases of pancolitis
Grossly: colonic mucosa red and granular or with extensive, broad-based ulcers
- Abrupt transition between diseased and uninvolved colon
- Ulcers along the long axis of colon
- Pseudopolyp: isolated islands of regenerating mucosa
- Mucosal atrophy in chronic disease
- No mural thickening or strictures
Complications:
- Colonic dilation and toxic megacolon: risk of perforation
What is seen here?

Ulcerative colitis
Describe the histology of Ulcerative colitis
Similar to Crohn: inflammatory infiltrates, crypt abscesses, architectural crypt distortion, and epithelial metaplasia
- Inflammation diffuse, limited to mucosa and superficial submucosa
- Severe case: extensive mucosal destruction with ulcers that extend more deeply into the submucosa
- Involvement of muscularis propria: rare
Signs of healed disease:
- Submucosal fibrosis
- Mucosal atrophy
- Distorted mucosal architecture to almost normal in prolonged remission
No granuloma
What is seen here?

Ulcerative colitis
- Increased chronic inflammatory cells in lamina propria
What is seen here?

Ulcerative colitis
- Cryptitis: neutrophils in the crypt epithelial cells
What are the clinical features of Ulcerative colitis?
Treatment?
Relapsing disorder:
- Episodes of bloody diarrhea with stringy, mucoid material
- Lower abdominal pain, and cramps
- Temporarily relieved by defecation
- Duration of symptoms days to months
Initial attack can present as medical or surgical emergency
- > 50% patients have mild disease, all with one relapse in 10 year
- 30% require colectomy in the first 3 years after presentation
Colectomy cures intestinal disease, but not extra-intestinal manifestations
T/F: Colitis is associated with a risk of malignancy
True- depends on duration and extent of disease
- (2% after 10 years, 8.5% after 20 years, and 17.8% after 30 years of disease)
What should be considered in the management of pts with ulcerative colitis?
Early detection of malignancy: surveillance 8 years after disease initiation
- Major exception: patients with primary sclerosing cholangitis; enrollment in surveillance at the time of diagnosis
- Regular and extensive mucosal biopsy is expensive
Describe diverticular disease
- Genetic or acquired
- Prevalence
- Contributing factors
- Basic mechanism
- Acquired pseudo-diverticular outpouchings of the colonic mucosa and submucosa
- Rare under 30 yo; 50% are 60+ yo in Western population
- Multiple = “diverticulosis”
- Dietary differences: less common in Japan
- Increased intraluminal pressure due to increased peristaltic contractions, enhanced by low fiber diet -> decrease stool bulk, especially in sigmoid colon
Pathophysiology of diverticular disease?
Low fiber diet
- > Chronic constipation
- > Increased intraluminal pressure
(Combined with possible connective tissue disorders)
- > Muscular hypertrophy
- > Herniation of mucosa through the muscular wall

What is seen here?

Diverticulosis
Describe the morphology of diverticular disease
- Location
- Shape
- Histology
- Most common in sigmoid colon
- Small, flask-like outpouchings, 0.5 to 1 cm in diameter, along the taeniae coli
Histology:
- Thin wall of a flattened or atrophic mucosa - Compressed submucosa,
- Attenuated or absent muscularis propria
Obstruction -> inflammatory change: diverticulitis and peri-diverticulitis -> perforation -> pericolonic abscesses, sinus tracts, and peritonitis
What is seen here?

Diverticular disease
Clinical features of diverticular disease?
- Most patients asymptomatic
- Often an incidental finding
- 20% have intermittent cramping, continuous lower abdominal discomfort, constipation, distention, and a sensation of never being able to completely empty the rectum
- Rarely regress in early stage of development
- More common: number increases and become large
- Symptomatic improvement with high-fiber diet
- When diverticulitis occurs, it most often resolves spontaneously and rare patients need surgery
What are polyps?
- Any localized projection above the surrounding colonic mucosa
- Most common in colon
- Most bengin
- Intestinal polyps: Non-neoplastic or neoplastic
- The most common neoplastic polyp: adenoma with potential to become malignant
Describe neoplastic polyps
- What types of tumors occur int he colon
- What is the most common neoplastic polyp
- Any neoplastic mass lesion in GI tract
- Carcinoid tumors, stromal tumors, lymphomas, and even metastatic carcinoma
- The most common neoplastic polyps: adenomas
- Benign polyps… majority of colorectal adenocarcinomas
Describe adenoma
- Shape
- Gender
- Sessile or pedunculated
- Equal genders
- 50% of adults in Western world by age 50 - Surveillance colonoscopy by age 50
- If family history: screen 10 years before the youngest age at which a relative was diagnosed
- Less common in Asia; increasing frequency
- ADENOMA = MILD DYSPLASIA
Describe the morphology of adenoma
- 0.3 to 10 cm in diameter
- Histologic hallmark: nuclear hyperchromasia, elongation and stratification
- Tubular, tubulovillous, or villous based on architecture
- Tubular adenoma: small, pedunculated polyps with small rounded, or tubular glands
- Villous adenoma: larger and sessile with slender villi
- Tubulovillous adenoma: mixture of tubular and villous
- Invasion more in villous adenoma
What is seen here?

Normal colonic mucosa (pedunculated tubular adenoma); the rest of crypts are darker

What is seen here?

Villous adenoma
Describe adenocarcinoma of the colon:
- Epidemiology
1 malignancy of the GI tract
Epidemiology
- 15% of all cancer-related deaths (2nd to lung cancer)
- Incidence peak: 60-70 yrs of age, fewer than 20% before 50
- Males > females
- Most prevalent in US, Canada, Australia, New Zealand…
Describe the pathogenesis/molecular events for development of cancer in the colon?
- Genetic and epigenetic abnormalities
- Two distinct genetic pathways:
- APC/β-catenin pathway, associated with WNT and the classic adenoma-carcinoma sequence
- Microsatellite instability pathway, associated with defects in DNA mismatch repair
- Stepwise accumulation of multiple mutations
- Epigenetic events, the most common one methylation-induced gene silencing, may enhance progression
Adenoma-carcinoma sequence?

Describe the morphology of tumors in the proximal vs. distal colon
- Tumors in proximal colon often polypoid, rarely cause obstruction
- Carcinomas in distal colon: annular with “napkin-ring” constrictions and luminal obstruction
- Both: grow into bowel wall: palpable firm mass
Right- and left-sided cancer have similar microscopic features
- Invasion: a strong stromal desmoplastic response
- Poorly differentiated tumor: few glands
- Some mucin production: poor prognosis
What is seen here?

Glands with necrotic material inside
What is the clinical presentation of colon cancer
- Endoscopic screening for adenomas
- Cecal and other right-sided colon cancers: fatigue and weakness due to iron deficiency anemia
- Iron deficiency anemia in an older man or postmenopausal woman is GI cancer until proven otherwise
- Left-sided tumors: occult bleeding, changes in bowel habits, or cramping/discomfort left lower quadrant
What is the prognosis of colon carcinoma?
- Poorly differentiated and mucinous tumors: poor prognosis
- Two most important prognostic factors: depth of invasion and lymph node metastases
- Patients with small numbers of metastases do well for years following resection of distant tumor nodules
- Clinical and molecular heterogeneity of colorectal carcinomas
- Metastases: regional lymph nodes, lungs and bones
- The most common site of metastases: liver


