1. lung volume and test Flashcards
(18 cards)
what is compliance
when does low and high compliance occur
what is compliance ensued by
what can be a cause of increased and decreased compliance
stretchiness
low compliance- at high pressure, stiffer lungs
high compliance- low pressure (base is more compliant than apex)
elastic recoil
increased- stretchiness of lungs due to ageing
decreased- fibrosis, alveolar oedema
what is needed for efficient lung ventilation
high compliance
surfactant to reduce surface tension
what type of tests are needed to be assesed and for which conditions?
mechanical condition: pulmonary fibrosis
resistance to airways: asthma
diffusion across alveolar membrane: pulmonary fibrosis
what are lung volumes dependent on

elastic properties and muscles of chest wall

Tidal volume
volume of air entering and leaving the lung with each normal breath
Inspiratory reserve volume (IRV)
Expiratory reserve volume (ERV)
extra volume of air inspired above the normal tidal volume with full force
extra volume of air expired by forceful expiration at the end of normal tidal expiration
Vital capacity (VC)
maximum amount of air expelled from the lungs after first filling the lungs to a maximum then expiring to a maximum (TV+IRV+ERV)
Volumes not measured using spirometry
Residual volume (RV) - volume of air remaining in the lungs after the most forceful expiration
Functional residual capacity (FRC) - amount of air that remains in the lungs at the end of normal expiration (ERV+RV)
Total lung capacity (TLC) - the maximum volume of air the lungs can hold (VC+RV)
forced vital capacity
FEV1.0
total volume of air exhaled
volume expired in the first second. Typically >70% FVC
FVC and FEV1.0 are defined as a ratio - FEV1.0/FVC
Lung function test - Functional residual capacity
how is this done?
- Residual air cannot be directly expired into the spirometer
- FRC (or TLC or RV) are measured using helium dilution or nitrogen washout

lung function test nitrogen washout procedure
- Patient inspires 100% O2
- Expires into the spirometer system
- Procedure repeated until N2 in lungs is replaced with O2
- FRC calculated from exhaled N2 and estimated alveolar N2
Restrictive deficit:
- Lung expansion is compromised - alterations in lung parenchyma, disease of the pleura or chest wall
- Lungs do not fill to capacity hence they are less full before expiration
- E.g. pulmonary fibrosis and scoliosis curve compresses lungs
- FVC is reduced, but the FEV1.0. is relatively normal
- The FEV1/FVC also remains relatively normal/increased
Obstructive deficit:
- Characterised by airway obstruction
- If airways are narrowed, lungs can still fill to capacity
- Resistance is however increased on expiration
- E.g. asthma, chronic obstructive pulmonary disease (COPD)
- FEV1.0 will be reduced, but FVC will be relatively normal.
- A low FEV1.0/FVC will be recorded
what does a vitalograph measure?
Measures the ability to move air out of the lungs FVC and FEV1.0
red restrictive
orange obstructive

millers prediction quadrant

what curve do you use in PEF
flow-volume curve
- Deep breath in - TLC Deep and fast breath out -RV
- Expiration ¯ lung volume - airways become narrower
- Flow falls and ceases at RV
- TLC - PEF: effort dependent - effort increases flow rate
- PEF - RV: effort independent - effort does not increase flow rate
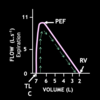
flow volume loops
Yellow- normal
Restrictive red- normal peak flow only the volume reduced
Orange- obstruction: total TLC, able to move air from larger but not smaller areas so scooping: cannot get area of the lung retain lots of air
RV more air as cannot expire completely a less stretchy

Gas transfer - Diffusion conductance
- Measure how easily carbon monoxide crosses from alveolar air to blood
- The patient inhales a single breath of dilute carbon monoxide followed by a breath-hold of 10 seconds
- The diffusion capacity is calculated from the lung volume and the percentage of CO in the alveoli at the beginning and the end of the 10s breath-hold
- Clinical relevance - e.g. in fibrosis of the lungs where gas diffusion is compromised


