W8 - Circulatory control (2.12, 2.13) Flashcards
What is AVDO2?
Average values.
arteriovenous O2 difference = 50 ml/l
- cO2 in art. blood = 200 ml/l
- cO2 in ven. blood = 150 ml/l
varies if O2 demands changed
Which mechanisms regulate the circulation?
- local control
- hormonal, humoral regulation (slow)
- reflex regulation (fast)
⇒ act by influencing Q and P
How is the circulalation controlled locally?
- Bayliss-effect (= autoregulation)
- metabolic regulation
- endothelium-mediated regulation
What is the Bayliss effect?
Where can it be seen?
blood flow is kept constant if perfusion pressure is changed in physiol. range (50 - 150 mmHg)
- in small art./arterioles (abundant SMC)
- ↑P → ↑d → ↓R
↓P → ↓d → ↑R

What is the mechanism of the Bayliss effect?
What does it constitute?
↑P → mechanosens. cation channels open in resp. to stretch → depolarization → L-type Ca2+ channels open → Ca2+ influx → constriction of SMCs → ↓d → ↑R
= myogenic tone
Which mechanisms constitute the basal/resting tone of a blood vessel?
How are they modulated?
- myogenic tone (mainly): influenced in response to stretch, high PO2, and Ca2+
- sympathetic tone
How does the resting tone in vessels differ?
- low in veins
- high in arteries
Which blood vessels are regulated locally by metabolites?
What is the consequence?
smooth m. of terminal arterioles/metarterioles + precapillary sphincters
→ functional hyperemia
Which metabolites can induce functional hyperemia?
Explain.
↑ function of organ → ↑ metabolism → ↑ local metabolites → vasodilation/relaxation of SMCs → ↑Q
- ↓pO2
- ↑pCO2
- lactic acid (→ ↓pH)
- adenosine
- ↑[K+]

When does reactive hyperemia occur?
Explain.
occurs after blood flow is stopped for a short time
⇒ extra Q lasts long enough to repay almost exactly the tissue O2 deficit that has accrued during the period of occlusion
→ peak flow + duration of reactive hyperemia proportional to duration of occl.
cells produce metabolites although Q interrupted, incr. metabolites cause vasodilation after orig. P restored

Describe endothelium-mediated regulation.
List vasodilators and -constrictors.
capillary endothelium is able to produce several vasoactive compounds that influence vessels w/ vascular SM
vasodilators: PGI2, NO
vasoconstrictors: angiotensin II, endothelin
What are the effects of PGI2 (= prostacyclin)?
- inhibit platelet adherence + aggregation
-
relaxation of VSMCs = vasodilation
prod. from arachnidonic acid, released in response to shear stress → activates Gs → ↑[cAMP] → PKA → phosphorylation of MLCK → ↓ constriction

Which substances cause the release of NO from the capillary endothelium?
↑ metabolism → ↑[metabolites] → ↓R → ↑Q
→ ↑ shear stress
- ACh
- bradykinin
- serotonin
- substance P
- histamine

What are the effects of NO?
- inhibits platelet aggregation, induces disaggregation
-
relaxation of VSMCs
produced from L-arginine by NO synthase → ↑[cGMP] → PKG → phosphorylation of MLCK → ↓ constriction

What happens during retrograde vasodilation?
propagation of vasodilation to upstream arterioles via gap junctions, which causes the entire tissue region to receive more flow
What is the difference btw hormonal regulation and local regulation by metabolites?
List some vasoconstrictors.
hormones → direct effect on VSMCs
- NE
- angiotensin II
- vasopressin
- serotonin
- endothelin
How does norepinephrine affect the vessel diameter?
When is it secreted?
hormonal regulation
secreted in response to symp. innervation, and by adrenal gland
binds to α1 → Gq → ↑[Ca2+]
How is angiotensin II produced?
secreted in response to decr. MAP → ↓ renal perfusion pressure
renin catalyzes angiontensinogen to angiotensin I, then converted to angiotensin II by ACE in the lungs
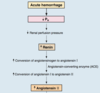
Which meds decrease the MAP by acting upon the renin-angiotensin-aldosterone system?
- ACE inhibitor: (e.g. captopril) blocks conversion of angiontensin I to angiotensin II
- angiotensin receptor (AT1) antagonist: (e.g. losartan) blocks action of angiotensin II at receptor
What are the effects of angiotensin II?
hormonal regulation
- stimulates synthesis + secretion of aldosteron
- ↑ Na+-H+ exchange in proximal convoluted tubule, ↑ Na+ reabsorption, contraction alkalosis
- ↑ thirst → ↑ water intake
- vasoconstriction of arterioles: binds to AT1R → Gq → ↑TPR, ↑MAP
⇒ normal MAP

What is the effect of aldosterone?
Where is it synthesized + secreted?
by adrenal cortex
→ ↑ Na+ reabsorption in renal coll. ducts, hence ↑VECF, ↑Vblood + ↑MAP
Describe the effects of vasopressin.
When is it released
released from post. pituitary in response to hypovolemia in atria
- binds to V2R → Gs → kidney function, H20 reabsorption
- hormonal regulation of vessel diameter
- *binds to V1R → Gq (therapeutically important)**
How does serotonin influence the vessel diameter?
normally via endoth.-med. pathway, but also as hormone
activates Gq
What is the difference btw hormonal regulation and local regulation by metabolites?
List some vasodilators.
hormones → direct effect on VSMCs
- E
- ANP
- PGI2
How does epinephrine affect the vessel diameter?
When is it secreted?
hormonal regulation
secreted from adrenal gland
- in low conc.: bind to β2 → Gs → ↑[cAMP] → vasodilation (only in sk. m., heart, liver)
- in high conc.: also binds to α1 → [α1] >> [β2] → vasoconstriction
How does ANP affect the vessel diameter?
hormonal regulation
prod. by atria when ↑Pv
binds to guanylyl cyclase → ↑[cGMP] → PKG → phosphorylation of MCLK → vasodilation
- inhibits renin secretion
- causes incr. secretion of Na+ and water
Differentiate btw types of receptors that are able to affect the blood pressure.
- high pressure receptors (baroreceptors): respond to changes in art. blood pressure
- low pressure receptors (baroreceptors): control the effective circulating volume → indirect effect on BP
- chemoreceptors dedicated to regulate respiration, secondary neural regulation of BP
What are the 2 most important mechanisms to regulate arterial blood pressure?
Differentiate btw short-term and long-term regulation.
- fast acting baroreceptor reflex in high pressure system (in sinus caroticus, arcus aorticus)
- slow acting baroreceptors in high pressure system → RAS-mechanism

Why is the baroreceptor reflex so important?
Where can high pressure baroreceptors be found?
respond to immediate changes in art. BP to fire APs dependent on the degree of activation (cf. own card)
mainly in sinus caroticus and arcus aorticus
How does the frequency of fired AP changes in response to step/static changes in arterial blood pressure?
frequency-modulated signals
- the faster the change in BP, the higher the fired AP frequency
- hence slower AP frequency for static blood pressure increases
⇒ work best in physiological range
(range dependent on location of receptor)

Describe differences btw high pressure baroreceptors.
located in regions of high BP (arteries)
in sinus caroticus:
- respond to lower pressures (50 - 200 mmHg)
- transmit signal via Hering’s nerve and n. glosspharyngeus to ncl. solitarius
in arcus aorticus:
- respond to higher pressures (100 - 200 mmHg)
- transmit signal via n. vagus to ncl. solitarius

How does the NTS affect blood pressure?
NTS receives signals from fast response baroreceptors
→ medullary cardiovascular center
2 parts:
- vasomotor area
- cardioinhibitory area
What is the function of the vasomotor area?
sympathetic function
- receives inhibitory neurons from NTS
→ when stimulated: vasodilation - otherwise producing tonic output → vasoconstriction
= vascular component of baroreceptor reflex
What is the function of the cardioinhibitory area?
parasympathetic function
- receives excitatory interneurons form NTS/ncl. dorsalis vagi
→ when stimulated: ↓ HR
= cardiac component of baroreceptor reflex

How is the heart innervated?
- symp. innervation: SA, AV node, ventricular muscle
- parasymp. innervation: SA, AV node
Define vasomotor tone.
= sympathetic tone
continuous partial constriction of blood vessels is caused by sympathetic firing of efferent fibers from the vasomotor center (0.5 - 2 Hz)
→ contributes to resting tone of 100 mmHg,
(can be lowered by local anesthesia and incr. by NE injections)

Which vessels are innervated sympathetically?
Describe.
-
resistance vessels: arteries + arterioles
(many α1, few β2) -
capacitance vessels: veins + venules
(many α1)
⇒ capacitance vessels show higher response to symp. innervation, constricted at a lower stimulation frequencies
BUT: respond less to vasodilator metabolitese

What is the pressor response?
When is it activated?
activated when blood pressure reduced in high pressure system = baroreceptor reflex
- in upright position (+ vasoconstr. of skin, sk. m.)
- severe hemorrhage (++ vasoconstr. in viscera, kdiney)
- heat stress (+ skin vasodilation)
⇒ ↑ vasomotor activity
⇒ heterometric heart regulation (↑ inotropy), homometric heart regulation (↑ lusitropy + inotropy)
<span>lusitropy = relaxation → </span>↑HR, inotropy = contractility <span>→ </span>↑stroke vol.
Explain the adaptation of high P baroreceptors.
baroreceptors adapt to sustained hypertension by decreasing the firing rate back to a lower level
→ “normal” firing rate

What is the function of low pressure baroreceptors?
Where can they be found?
detect “fullness” of vascular system
⇒ respond to increases in blood volume (transfusion)
-
in low pressure system
= in venae cavae, sinus venarum cavarum

Differentiate btw fiber types of atrial low pressure baroreceptors.
What is their function?
- type A: fire during diastole → monitor HR
- type B: fire during systole → monitor rising atrial volume
⇒ ↑ HR + hormonal regulation

What is the Bainbridge reflex?
reason for ↑ HR in response to incr. blood volume detected by low-pressure baroreceptors
↑ blood volume → ↑ venous return → stimulation of low-pressure baroreceptors via atrial stretch → ↑ HR by acting upon SA node via n. vagus
opposes to how the highpressure baroreceptors decrease the HR in response to high P. However, this is completely logical because atrial pressure needs to be low in order to receive blood from the veins, while arterial pressure needs to be high to pump to the brain

As a summary..
Describe the overall effects of atrial stretch detected by low-pressure baroreceptors.
- ↑HR (Bainbridge reflex)
- vasodilation in kidney → incr. GFR/excretion of Na+ and water
- ↓ secretion of ADH → less fluid retention
- ↑ secretion of ANP → decr. Na+ reabsorption
⇒ diuresis
What is the difference btw high and low pressures baroreceptors?
high pressure baroreceptors:
- incr. stretch lowers heart rate
- attempt to lower art. blood pressure via general vasodilation
low pressure baroreceptors:
- incr. stretch raises heart rate
- attempt to decr. blood volume (hence BP) via vasodilation in kidney + hormonal responses
What happens during the Valsalva maneuver?
large breath w/o exhaling → ↑ intrathoracic pressure
- ↑ tension of lung mechanoreceptors → ↓ vagal activity
- ↑ right atrial pressure → ↓ venous return → ↓ CO → ↓BP → baroreceptor reflex
⇒ ↑ HR
NOTE: initial compression of thoracic aorta causes elev. BP, hence decr. HR

What is the function of chemoreceptors?
- increase ventilatory drive by detecting pO2, pCO2, pH
- also: changes BP through changes of para-/symp.output
Explain the function of peripheral chemoreceptors.
Where can they be found?
Characteristics.
primarily sensitive to low [O2], but also high [CO2]/low pH
= glomera carotica near bifurcation of common carotic aa., glomera carotica in arcus aorticus
- pos. drive on vasomotor centers → vasoconstriction in sk. muscle/splanchnic vasc.
- pos. drive on cardioinhibitory centers → ↓HR
vasoconstriction to redirect blood to brain

Explain the function of central chemoreceptors.
Where can they be found?
sensitive to low pH/high [CO2],
responsible for resting breathing rhythm
= in formatio reticularis of medulla
↓ cerebral blood flow → ↑[CO2] → ↓pH → pos. drive on vasomotor center → incr. symp. outflow → vasoconstriction → ↑TPR → blood redirected to brain
What is the protecting reflex of chemoreceptors?
In which blood pressure range does it mainly happen?
Graph.
incr. chemoreceptor sensitivity at BP < 60mmHg
→ emergency situations (hypoxia, acidosis, hypercapnia)
hypercapnia = CO2 retention

Explain the intrinsic cardiovascular response.
if BP drops to 40-60 mmHg (+ holding breath)
→ peripheral chemoreceptors activated in response to hypoxia, acidosis, hypercapnia
⇒ vasoconstriction + bradycardia
incr. perfusion P in per. tissue + heart slows down to prevent all O2 rushing into the tissue (according to Ben lol)

How is the complex cardiovascular/respiratory response different from the intrinsic cardiovascular response.
if BP drops to below 40 mmHg + breathing possible
→ additionally central chemoreceptors activated in response to hypercapnia
⇒ reflex tachycardia
for better understanding: no vasoconstriction bc incr. alveolar constr. raises pH, no direct effect of central chemorec. on BP, cf. figure

Which reaction is described by the Cushing reflex?
illustrates how chemoreceptors work
↑intracranial pressure → compression of cerebral blood vessels → cerebral ischemia + ↑ cerebral PCO2
↑symp. outflow → ↑BP
⇒ high-P baroreceptors → ↑parasymp. outflow → ↓HR
What is the function of Bezold-Jarisch reflex?
temporary bradycardia + hypotension to protect the heart in case of O2 deficiency (e.g. during myocardial ischemia, infarction)
triggered by chemo-, mechanoreceptors in left ventricular wall
due to decr. vasomotor + incr. cardioinhibitory acitivity


