Viral Infections of the Skin Flashcards
What are the two types of Herpes Simplex (HSV) and where are they typically found?
• what percentage of adults have abs to these?
HSV-1
• Perioral, Lips, Oral Cavity
• 85% of adults have antibodies to this virus
HSV-2
• Genital
• 20-25% of adults have abs to this
HSV
• How is it spread? when do you realize you got it?
• Where does it go?
• When can you get infected?
Spread via SKIN to SKIN contact and symptoms appear 3 to 7 days after exposure. It spreads most often via sensory nerves to Ganglia where the infection can be latent.
Infection can happen during Recurrences and during Asymptomatic Viral Shedding
What type of genome does HSV have?
HSV has a dsDNA genome
How does a primary Herpes Simplex infection feel?
• compare a recurrent infection to this.
Primary Infection:
• Pain, Burning, Tingling, Fever, Mailase, LAD
Recurrent Infection:
• Milder
What are some Triggers of HSV?
- Fever
- Sun exposure (cold sores)
- Stress
**What are some key features that you need to look for in Herpes Simplex Infections?
- Monomorphous Vesicles with an ERYTHEMATOUS BASE (very important for differentiating it from other conditions)
- punched out (cookie cutter si
milarity) erosions and crusted papules
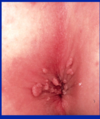
What key feature is seen here?
• what is this?

Erythematous Background to cookie cutter pustules
This is Herpes Simplex I most likely
What type of herpes is this?

Genital Herpes = HSV-2
HSV-1 shown below on lips (crusty)

Somone presents with this lesion. What do you do to confirm the diagnosis?
• what are you looking for?
- Open a fresh vesicle to do a Tzanck Smear and you’re looking for **multinucleated giant cells to confirm the dx
- You can also do aViral Culture or PCR**

You need to culture HSV to confirm the Dx. Until cultures come back what else could be in your differential?
Impetigo (top) Aphthous Stomatitis (middle) Syphilitic Chancre (bottom)

A person got a Tzank smear that showed this?
• significance?

They have Herpes
How do you treat HSV?
• Mild?
• Severe?
Mild HSV:
• Topical Antiviral
Moderate to Severe HSV:
• Systemic Antiviral (oral or IV)
Herpes Zoster (VZV)
• what is it?
• What are the chances of getting this?
• Who is at the greatest risk of getting this?
Herpes Zoster = Shingle => Reactivated VZV
Risk of Reactivation is 20-30%:
• People over 60 and the Immunosuppressed are at extremely high risk
Where does Varicella (herpes) Zoster Virus hide?
• what is the genome like for this virus?
• what are some triggers?
VZV sits latent in the dorsal root ganglion its a dsDNA virus
Triggers:
• Trauma
• Stress
• Fever
• Radiation
• Immunosuppression
How does someone typically present with a Herpes Zoster reactivation?
Often they have pain, itching, and burning before the lesions appear (may in their back etc.)aka PRODROME. When lesions do appear they are dermatomal (b/c this virus lives in nerves). Most often this occurs on the TRUNK.
What location can VZV reactivate in that is particularly dangerous?
• what are some associated complications?
• How often does this happen?
Trigeminal Nerve Reactivation -> Happens in 10-15% of cases
V1 Opthalmic Distribution Reactivation:
• Nasociliary Branch
• BLINDNESS
V2 and V3:
• Facial Palsy
• Tinnitus, Vertigo, Deafness
Why should you be worried when someone has Shingles and you see vesicles at the tip of their nose?
This is Hutchinson’s Sign. It indicates that the reactivation is in the V1 branch of trigeminal and blindness could be a complication.
How long does it take Shingles to Resolve?
• are there any long-term consequences?
Takes 3-5 weeks to resolve typically
Postherpetic Neuralgia occurs 5-20% of the time (mostly in people over 40)
What characteristics let you know that this is Herpes Zoster (shingles)?

Single Dermatome affected
See below for opthalmic nerve reactivation of VZV

What is a key way to differentiate Herpes Simplex from Herpes Zoster?
Herpes Zoster STAYS in a DERMATOME, Simplex does not stay in a dermatome. Simplex is also less painful.
How would you confirm the diagnosis of Herpes Zoster?
- *Tzanck Smear** (mutinucleated giant cells)
- *Viral Culture** (not practicle for VZV)
- *PCR**
What is the treatment for Shingles?
• What can you do to prevent it? how effective is this?
Shingles
• Treat withing 72 hours with Oral Antiviral
• Pain Meds needed
Prevention:
• Vaccine for all people 60 years and older
• Decreases risk by 1/2 and neuralgia by 2/3
Molluscum Conatgiosum
• genomic structure
• Transmission
• duration of infection
Molluscum Contagiosum = POX VIRUS
• Large dsDNA virus with CYTOPLASMIC inclusions
Transmission:
• Skin to Skin or autoinoculations/fomites
Duration:
• Infection may resolve completely in Months to Years
What does Molluscum Contagiosum look like?
• common locations?
Key Features of MC:
• Pink to Skin colored 2-10mm DOME-SHAPED WAXY PAPULES
• ± central umbilication (important feature but not always present)
Commonly found on:
• Chest, Face, Extremities