Skin Cancer (non-melanoma) Flashcards
(53 cards)
What are the layers of the Epidermis?
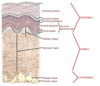
What are the layers of the dermis?

What are the layers of the hypodermis?

Where should melanocytes be located?
Basal Layer

Diagnosis?
• key features?

Basal Cell Carcinoma
• Pearly appearance
• Teleangectasias
• Ulcerated
What cancer is shown here?
• what are the key histologic features?

Basal Cell Carcinoma
KEYS:
• This is a blue tumor on H and E (because these are progenator cells we expect them to have big active nuclei)
• Nodular appearance is very important (especially when differentiating from melanoma)
• Pallisades of blue nuclei that CLEFT AWAY from the surrouding tissue
What pathway and gene is often altered in this cancer?

Basal Cell Carcinoma often has mutations in the PTCH gene in the sonic hedgehog path.
What cancer is this?
• what feature puts patients at the greatest risk of metastasis?

• Squamous Cell Carcinoma (take note of keratin pearls)- if this is found in the EAR or LIP there is a high risk of metastasis.

What group has a rising incidence of Skin Cancer of all types?
Young Females due to tanning bed use
What is the most common neoplasm in the US?
Basal Cell Carcinoma
What is the role of the altered gene that is frequently implicated in this cancer?

PTCH gene is commonly involved in Basal Cell Carcinoma development (thats what makes vismodegib and sonetigib good in BCC tx). This is a TUMOR SUPPRESSOR GENE because it prevents constant activation of the smoothened (SMO) receptor
What risk factors put patients at the greatest risk for Basal Cell Carcinoma?
RISK:
• Chronic but Intermittent UV exposure
• fair complexion
• hx of Sunburns (blistering)
• Family Hx
• Immunosuppression
What is the most common risk factor implicated in the development of Basal Cell Carcinoma?
• Role of immunosuppression in BCC vs. SCC?
- Chonic Intermittent UV exposure like that encounter by people that go on vacations and get sunburned
- Immunosuppression increased incidence 10x in BCC but still immunosuppressed pts. are more likely to get SCC
What is this?
• what would you expect to see on histology?

BCC
Histology will show blue, nodular, pallisading basal cells that cleft away from surrounding tissue

What are the key features of the Skin cancer shown here?

Basal Cell Carcinoma

Note: Clefting is aka Retraction Artifact
Also there are several subtypes of BCC:
• Nodular
• Superficial
• Pigmented
• Morpheaform
• Micronodular
• Cystic
• Infiltrative
What is seen on the left and right in these pictures?

The are BOTH Basal Cell Carcinomas
Left: Superficial Basal Cell Carcinoma
Right: Nodular Basal Cell Carcinoma

What is shown here?

Basal Cell Carcinoma (nodular subtype)
• well circumscibed with pearly rolled border and central erosion with telangiectasias
What is this?

BCC - with prominent telangiectasias
What is this?

SUPERFICIAL BCC - note its more patchy, flat and broad, but still has telangectasias and a semi-pearly quality
What is this?

Superfical BCC
What is this?
• what subset of patients is this most likely to happen in?
BCC - note that this is abnormal in that it’s hyperpigmented. This is more likely to happen with a darker skin tone.
Only 20% of people get basal cell carcinomas before age 50. Under what age should you really start to worry about something genetic?
• what genetic defect would you be worried about?
• PTCH tumor suppressor gene in the SHH pathway can be mutated via an inherited defect that predisposes people to Basal Cell Carcinomas
What is is called when people have inherited mutations in their PTCH1 gene?
• How is this inherited?
• what manifestation do we see?
• What are these patients at risk for other than BCC?
Gorlin Sydrome aka Basal Cell Nevus Syndrome is associated with mutations in the PTCH1 gene. These patients often get BCC’s in their twenties with musculoskeletal defects like JAW CYSTS.
RISKS:
• Medulloblastoma
• Fibrosarcoma
• Basal Cell Carcinoma




























