Urology Flashcards
What are some local clinical features of urological problems in children?
- Pain
- Changes in urine
- Abnormal voiding
- Mass
- Visible abnormalities
What is an inguinal hernia?
Herniation into the inguinal canal and potetntially scrotal sac, and is usually caused by a persistently patent processus vaginalis
99% are indirect hernias

What percentage of inguinal hernias are direct?
1%
How does an inguinal hernia present?
- Lump in the groin - which may extend into the scrotum
- Intermittent - visible during straining
-
Pain - if incarcerated - painful lump
- Intestinal obstruction
- Strangulation of testes
Who is more likely to develop an inguinal hernia; boys or girls?
Boys - 9:1
How would you manage an inguinal hernia?
-
< 1 year
- URGENT referral
- Repair - no place for observation
-
> 1 year
- Elective referral and repair
-
Incarcerated
- Reduce and repair on same admission
What is a hydrocele?
Due to a patent processus vaginalis which allows fluid to collect around the tesicle in the tunica vaginalis or within the cord
Same concept as a hernia, but passageway is much narrower

What guides the testes as they migrate down into the scrotum embryologically?
Mesenchymal gubernaculum

How would you distinguish a hydrocele from a inguinal hernia?
- Can you get above the swelling?
- Hydroceles normally tranilluminate
- Tend to be bluish in colour

How would you manage a hydrocele?
- Conservative - normally closes on it’s own
- Surgical - if it persists beyond 2 years
What is cryptorchidism?
Undescended testis
The abscence of one or both testes from the scrotum
Any testis that cannot be manipulated into the bottom half of the scrotum
What types of cryptorchidism are there?
- Retractile - Can pull down, but retract - strong chremasteric reflex - dartos muscle
- True cryptorchidism - Properly undescended
- Ectopic - wrong line of descent
- Ascending Testis
What are risk factors for developing cryptorchidism?
Prematurity
How would you investigate a suspected undescending testis?
-
Examination
- Warm room + Warm hands
- Testis may be felt in the scrotum/may need to be delivered
- Palpable testis - may be felt in the groin
What could be the cause of an impalpable testis?
- In the inguinal canal but cannot be identified
- Intra-abdominal
- Absent
- Atrophic
What is the difference between a retractile and undescended testis?
Retractile can be manipulated into the scrotum with ease and without tension
Activation of cremaster muscle pulls the testis up
How would you manage an undescended testis?
Orchidopexy
Why are orchidopexies performed to treat undescended testicles?
- Cosmetic
- Reduced tisk of torsion/trauma
- Fertility
- Risk of malignancy - greater if bilateral/intra-abdominal
What is an absolute indication for circumcision?
Balanitis Xerotica Obliterans
Lichen sclerosis of the penis
What are relative indications for circumcision?
- Balanoprosthitis
- Religious
- UTI
What are complications of circumcision?
- Bleeding
- Meatal stenosis
- Fistula
- Cosmetic
What is torsion of the testis?
Occurs when the spermatic cord (from which the testicle is suspended) twists, cutting off the testicle’s blood supply

What age range does testicular torsion occur most commonly in?
Post pubertal
How does testicular torsion present?
- Severe pain - may be localised to groin or lower abdomen
- Redness
- Swelling
What increases the risk of testicular torsion?
- Undescended testis
- Clapper bell testis - testis lying transversely on its atachement to the spermatic cord

How should you manage testicular torsion?
Treated ASAP - oterhwise very high risk of loss of testicle
- Scrotal exploration
- Testicular fixation - both testicles
What is the differential diagnosis for an acute scrotum?
- Torsion testis/torsion appendix testis
- Epididymitis
- Trauma
- Haematocele
- Incarcerated inguinal hernia
What is torsion of appendix testis?
The testicular appendage (hydatid of morgany), which is a mullerian (paramesonephric) remnant usually located on the upper pole of the testis. Torsion occurs when this becomes twisted

How does torsion of the appendix testis present?
- Pain - evolves over days
- Blue dot - seen through scrotal skin

How would you manage torsion of the appendix testis?
-
Scrotal exploration
- Can’t always tell it’s not testicular torsion
- If blue dot is present + Pain is controlled -> no need for surgery
Which is more common; torsion of the testis or torsion of the appendix testis?
Torsion of the appendix testis
What age group does torsion of the appendix testis most commonly affect??
Prepubertal boys
How does a UTI present in infants?
- Fever
- Vomiting
- Lethargy and irritability
- Poor feeding/faltering growth
- Jaundice
- Septicaemia
- Offensive urine
- Febrile seizure (> 6months)
What is the definition of UTI in a child?
Clinical signs PLUS
- Pure growth bacteria > 105
- Pyuria - pus cells
- Systemic upset
- OR mixed growth bacteria, no pyuria, no systemic symptoms
Up to what age do UTI’s occur more commonly in boys than girls?
Up to 3 months
What are the organisms most commonly implicated in urinary tract infections in children?
- E.coli (85%)
- Klebsiella
- Proteus
- Pesudomonas
- Strep Faecalus
What is the most common organism found in boys with UTI?
Proteus
What can UTIs colonised by proteus predispose to?
Development of phosphate stones
How do children present with UTI’s?
- Dysuria/Frequency/Urgency
- Abdominal pain/loin tenderness
- Fever +/- rigors
- Lethargy and anorexia
- D + V
- Offensive, cloudy urine
- Febrile seizure
- Recurrence of enuresis
What investigations would you do if you suspected a UTI in a child?
- Dipstick and Culture/Microscopy
- Abdominal US
- Assess for reflux
What threshold on bacterial culture needs to be reached before UTI can be diagnosed?
>1x105 CFU/ml - 90% probability
What is bacteriuria?
The presence of bacteria in urine but not if bacteria’s presence is due to contamination during urine sample collection.
Bacteria often indicate a urinary tract infection, although bacteriuria can also occur in prostatitis.
May be asymptomatic - can cause scarring, increased BP and CKD
What is chronic pyelonephritis?
Histological/radiological diagnosis with juxtaposition of a cortex scar and dilated calyx.
Can cause hypertension and renal failure
If you took a catheter or suprapubic urine sample, what would be diagnostic of UTI?
Bacterial growth of a single organism per millilitre
On dipstick, if you saw positive leucocytes and nitrites in the context of suspected UTI, how would you interepret?
Regard as UTI if clinical symptoms present
On dipstick, if you saw leucocyte negative and nitrite positive in a child with suspected UTI, how would you interpret this?
Treat as UTI if clinical symptoms
Depends on urine culture
On dipstick, if you saw lecuocyte positive and nitrite negative in a child with suspected UTI, how would you interpret this?
Start treatment for UTI if clinical symptoms
Diagnosis depends on urine culture
On dipstick, if you saw leucocyte and nitrite negative in a child with suspected UTI, how would you interpret these results?
UTI unlikely - repeat or send urine for culture if clinical history suggests UTI
What is vesicoureteric reflux?
Developmental anomaly of the vesicoureteric reflux. The ureters are displaced laterally and enter directly into the bladder rather than at an angle

What can cause VUR?
- FH
- Neuropathic bladder
- Urethral obstruction
- UTI - temporary VUR
Why is VUR associated ureteric dilatation important?
- Urine returning to bladder from ureters after voiding means bladder does not empty properly
- Kidneys may become infected - especially if there is intrarenal reflux
- Bladder voiding pressure is transmitted to the renal papillae which may contribute to renal damage if voiding pressures are high
How can UTIs in children cause Kidney complicatons?
Bacteria can move into the kidney and lead to scarring. Scarring of the kidney can be associated with high blood pressure and kidney failure.
How would you investigate for VUR?
- Abdominal US
- Renal US - renal size/scarring
- DMSA scan - function
- MAG3 Scan
- MCUG Scan - gold standard
What is a DMSA Scan?
Detects functional defects, such as scars or areas of nonfunctioning renal tissue, but very sensitive.
Need to wait at least 2 months after UTI to avoid diagnosing false scars

What is a MAG3 renogram?
Dynamic scan, isotope-labelled substance MAG3 excreted from the blood into the urine.
Measures drainage, best performed with high urine flow so furosemide often given
In children old enough to cooperate (>4 years), scan during micturition is done to identify VUR

What is a micturating cycstourethrogram (MCUG)?
Contrast introduced into the bladder through urethral catheter.
Can visualise bladder and urethral anatomy. Detects VUR and urethral obstruction
REQUIRES CATHETERISATION

What is the best way of excluding reflux?
MCUG
However, if DMSA is negative, then MCUG is almost always negative
What are the different grades of VUR?
- Grade I - incomplete filling of upper urinary tract
- Grade II - Complete filling +/- slight dilatation
- Grade III - Ballooned calyces
- Grade IV - Megaureter
- Grade V - Megaureter + hydronephrosis

How would you empirically treat a child (>1 month - 18 years) with lower UTI or cystitis?
Oral Trimethorpim or Cefalexin
3 days

How would you empirically treat suspected pyelonephritis in a child less than 6 months old?
IV Cefotaxime or Ceftriaxone
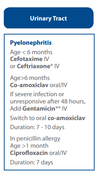
How would you emprically treat a pyelonephritis in a child > 6 months?
Oral/IV Co-amoxiclav +/- Gentamicin, then switch to oral co-amoxiclav
7 days duration

What would you use in treating a pyelonephritis in a child > 6months of age who is penicillin allergic?
Oral/IV ciprofloxacin

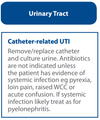
How would you empirically treat a catheter related UTI in a child?
Remove catheter
Antibiotics only if evidence of systemic infection
What would indicate an upper UTI/pyeloneprhitis in a child?
Bacteriuria and fever >/= 38oC, or
Bacteriuria + loin pain/tenderness even if fever is <38oC
How could you reduce the risk of children getting UTIs?
- High fluid intake -> increased output
- Regular voiding
- Complete bladder emptying
- Prevention of constipation
- Good perineal hygeine
- Antibiotic prophylaxis
How would you manage a child with VUR?
- Conservative - Voiding advice, constipation, fluids
- Antibiotic prophylaxis - Trimethoprim (2mg/kg nocte)
- STING (submucosal Teflon injection) - if it doesn’t resolve on conservative management + Mild/moderate with symptoms
- Ureteric reimplantation - severe reflux
What is PUJ obstruction?
Pelvi-ureteric junction (PUJ) obstruction/stenosis, also known as ureteropelvic junction (UPJ) obstruction/stenosis, can be one of the causes of an obstructive uropathy.
Can be congenital or acquired with a congenital PUJ obstruction being one of the commonest causes of antenatal hydronephrosis without VUR
How would you manage PUJ obstruction?
- PNUS (Post Natal Ultrasound)/Renography
- Surgery
What can cause antenatal hydronephrosis?
- VUR (Vesico-Ureteric Reflux)
- VUJ obstruction (Vesico-ureteric Junction Obstruction)
- Posterior urethral valves
- Multicystic kidney (MCDK)
- Duplication anomalies
- PUJ obstruction (Pelvi-ureteric Junction Obstruction)
What is hypospadias?
Urethral meatus on the ventral aspect of the penis
Thought to arise from failure of development of the ventral tissues of the penis, in particular uretheral closure

What are the three typical features of hypospadias?
- A ventral urethral meatus (variable position)
- Ventral curvature of the shaft (chordee)
- Hooded prepuce

What is phimosis?
Pathologically non-retractile foreskin

What is balanoposthitis?
Single attack of redness and inflammation of the foreskin, sometimes with purulent discharge
Responds rapidly to warm bath and antibiotics

What is pyuria?
The presence of pus in the urine, typically from bacterial infection.
Defined as the presence of 6-10 or more neutrophils per high power field of unspun, voided mid-stream urine
What is daytime eneuresis?
Lack of bladder control during the day in a child old enough to be continent (>3-5 years of age)
What can cause daytime enuresis?
- Lack of attention to bladder sensation
- Detrusor instability
- Bladder neck weakness
- Neuropathic bladder
- UTI
- Constipation
- Ectopic ureter
How would you investigate daytime enuresis?
- Urine microscopy and culture
- Ultrasound
- Urodynamic studies
What is secondary (onset) enuresis?
Loss of previously gained continence
What can cause secondary enuresis?
- Emotional upset
- UTI
- Polyuria from diuresis in diabetes or renal concentrating disorder
How would you investigate secondary enuresis?
- Urine dipstick - infection, glycosuria, proteinuria
- Early morning urine osmolality sample
- Ultrasound of renal tract
When should a DMSA scan be performed?
4–6 months following the acute infection - should be used to detect renal parenchymal defects.
What should be the first line imaging used for checking for VUR in a child with atypical/recurrent UTIs?
Abdo ultrasound. This can be followed by DMSA after 3 months

Should a child with a first UTI have an abdominal ultrasound as part of their investigaitons?
- No - if child was symptomatic and had response within 48 hrs to treatment
- Yes - if <6 months, atypical or recurrent infecton
What are features of an atypical UTI in a child?
- Seriously ill/septicaemia
- Poor urine flow
- Abdominal or bladder mass
- Raised creatinine
- Failure to respond to treatment with suitable antibiotics within 48 hours
- Infection with non-E. coli organisms


