Squamous cell carcinoma, Bowen's, actinic keratosis and keratoacanthoma Flashcards
Define squamous cell carcinoma.
Proliferation of atypical, transformed keratinocytes in the skin with malignant behaviour.
It ranges from in situ tumours (also known as Bowen’s disease) to invasive tumours and metastatic disease.

How common is SCC of the skin?

- 2nd most common non-melanoma skin cancer worldwide, secondary to BCC.
- Tropical Australia has the highest incidence of all types of skin cancer, with incidence of SCC of around 1/100 for the white population
What are the causes/RFs of squamous cell carcinoma?
- Fair skin
- Sun exposure
- Living near equator
- Ionising radiation
- Burns
- Previous psoralen and UV-A light therapy
- Hereditary skin conditions
- Actinic keratosis (thiazide diuretics and cardiac drugs may predispose to this)
- Environmental toxins - arsenic, tar, HPV
- Immunocompromise
- Old age and male sex
- Red tattoo ink
- Smoking
Where are SCCs most commonly found?
Most commonly detected on head and neck (84%) and extensor upper extremities (13%)
What is the typical presentation of SCC?
Often present with multiple actinic keratoses (AK).
- Growing tumours - tend to grow over time but keratoacanthomas may grow rapidly.
- Bleeding
- Crusting
- Evidence of sun damage to skin
- Tender/itchy non-healing wound caused by trauma
- Erythematous papules/plaques, may be thin and flesh coloured
- Dome-shaped nodule (keratoacanthoma)
- Exophytic, fungating, verrucous nodules or plaques - verrucous carcinoma
- Constitutional symptoms

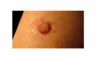
This 80-year-old man (a retired army officer who spent 30 years in the Far East) presents with the lesion shown. What is the diagnosis and treatment?

SCC
Erythematousm superficial erosion, no keratinal scale, rolling of edges (this is more common in a BCC but the history of onset here makes it SCC), painful.
Poorly differentiated because well differentiated ones produce keratin.
Treatment:
- Surgery with appropriate reconstruction
- Radiotherapy - not chemosensitive and too big for excision alone.
What investigations would you do for a suspected SCC?
Biopsy - shows full thickness keratinocyte atypia (in Bowen’s disease this is confined to the epidermis and intact BM but may become an invasive tumour)
Other: if suspected metastasis:
- FBC - check bone marrow involvement
- CT/MRI/PET/ LFTs/ CXR
Can you distinguish between actinic keratoses and SCC?
Because AKs and SCCs are on a spectrum, it is often difficult to clinically distinguish between the two. In general, SCCs tend to be symptomatic and are thicker, larger, more indurated than AKs.

What is the difference between the superficial scale on an SCC and a BCC?
SCC - You should always take off the scale (in hyperkeratotic lesions) when examining. It will bleed and be tender and painful. You need to take a punch biopsy for diagnosis from the naked lesion.
BCC - when scale is taken off, you would just see a superficial lesion with no bleeding.

When does an SCC make keratin?
When it is well differentiated
Poorly differentiated SCCs will look eroded and not make keratin. Below.
Which of the following are relevant prognostic factors for SCC?
- Size of the lesion
- Age of the patient
- Sex of the patient
- Cervical lymph node involvement
- Heavy smoking
- Cervical lymph node involvement
- Size of the lesion
Which of the following are useful in preventing SCCs?
- Sun cream
- Broad brimmed hats
- Solar swim suits
- Vitamin D tablets
- 5 – fluorouracil cream
Sun protection is the key. Fluorouracil is used to treat solar keratoses.
- Sun cream
- Broad brimmed hats
- Solar swim suits
How do you manage SCC?
- 2WW referral - they spread by blood and lymphatics
- Incisional biopsy
- SCCs are radiosensitive so may be good for radiotherapy
- CT if metastasis suspected
What is the difference between AK and Bowen’s disease?
AK - pre-cancer, some mutations but not enough - usually treated by cryotherapy, lasers or chemical peeling
Bowen’s - SCC in situ (i.e. within epidermis) - usually treated by excision, Mohs’, topical 5-FU etc

Describe the appearance of AK.
- skin-coloured, yellowish, or erythematous,
- ill-defined, irregularly shaped,
- small, scaly macules or plaques
- localised to sun-exposed areas of the body
- have the potential to progress into SCC





