Session 9 Flashcards
Consider the role of infections in chronic health conditions
[*] Chronic diseases cause a change in the structure or function of affected tissues/organs which may have the potential for changing the interaction between the patient and micro-organisms (NB: some patients are predisposed).
[*] This may be subsequently and further affected by changes caused by the altered presence of microorganisms and the consequences of treatment e.g. with antibiotics and steroids.
[*] Chronic diseases Congenital
- Genetic
- Developmental
[*] Acquired
- Vascular
- Infective
- Traumatic
- Autoimmune
- Metabolic
- Inflammatory
- Neurological
- Neoplastic
- Degenerative
- Environmental
- Idiopathic
[*] Improvements in healthcare are leading to increasing numbers of people with chronic illnesses living for longer.
[*] Many chronic illnesses predispose to infection, often of a specific and predictable pattern
[*] Planned changes in the delivery of healthcare in England will see many of these patients being cared for in the community (primarily cared for by GPs)
[*] Successful management of chronic illnesses need to include management of these infections.

Describe the pathogenesis and clinical consequences of CF
[*] Pathogenesis of CF
- Autosomal recessive
- Very common genetic disorder in this country
- Defect in CF transmembrane conductance regulator genes in exocrine glands
- Range of different mutations
- Most common mutation is ΔF508 (deletion of phenylalanine at position 508)
[*] Clinical consequences of CF
- Defects in CFTR leads to defects in Cl- transmembrane transport
- Mucus becomes dehydrated and thick causing blockage in small ducts in the lungs => bronchiectasis
- Lung colonisation and infection with a procession of different organisms
- Lung damage, antibacterial and steroid treatment

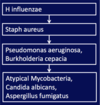
What organisms are found in CF infections? And why is CF so common?
- H influenza – non capsulated virus strain which only causes local disease (doesn’t spread) – normally in first few months.
- Staph aureus – around ages 2-3 years
- Pseudomonas aeruginosa and Burkholderia cepacia (environmental organisms found in the water supply) – can be life threatening as patients are very vulnerable, organisms can be very difficult to treat (antibiotic resistant). Pseudomonas aeruginosa produces a mucoid biofilm, which protects against phagocytosis against macrophages. Treatment requires a combination of antibiotics.
- Atypical Mycobacteria (any mycobacteria that isn’t TB), Candida albicans, Aspergillus fumigatus
[*] Why is CF so common?
Frequency of CF gene carriage in different populations
- European 1 in 25
- Hispanics 1 in 46
- Africans 1 in 65
- Asians 1 in 90
? Heterozygosity provides resistance to cholera, typhoid or TB?
In vitro interactions between CFTR protein and cholera toxin, Salmonella Typhi intracellular entry but no in vivo demonstration of benefit.
Describe COPD and infections
- Chronic inflammatory response to inhaled irritatns, primarily mediated by neutrophils and macrophages.
- Breakdown of lung tissue (emphysema) and small airways disease (obstructive bronchiolitis) creating problems with breathing
- Increased mucus production

Describe Diabetes and Infection
[*] Diabetes and infections (can be community or hospital acquired)
Hyperglycaemia and acidaemia impair
- Humoral immunity
- Polymorphonuclear leukocyte and lymphocyte functions
Diabetic microvascular and macrovascular disease results in poor tissue perfusion and increased risk of infection
Diabetic neuropathy causes diminished sensation resulting in unnoticed skin
[*] Sensory neuropathy, atherosclerotic vascular disease and hyperglycaemia all predispose to an increased risk of skin and soft tissue infection (especially the feet)
[*] Causative organisms include:
- Staph aureus (folliculitis (infection of the hair follicles in the skin), cellulitis)
- Group A Beta-haemolytic Streptococcus (cellulitis)
- Polymicrobial including Staph aureus, Beta-haemolytic streptococci, Enterobacteriaceae and various anaerobes => Diabetic foot ulcers and necrotising fascitisi.
- A co-infection of aerobe and anaerobe working together causes more and more tissue damage.
Describe Diabetes and ENT infections
Malignant or necrotizing otitis externa
- Pseudomonas aeruginosa
- Infection starts in the external auditory canal and spreads to adjacent soft tissue, cartilage and bone. Patients typically present with severe ear pain and otorrhoea (ear discharge, pus)
Rhinocerebral mucormycosis
- In patients with poorly controlled diabetes, especially those with diabetic ketoacidosis.
- Mould fungi
Organisms colonize the nose and paranasal sinuses, spreading to adjacent tissues by invading bone vessels and causing soft tissue necrosis and bony erosion.
Describe Diabetes and Urinary Tract infections
- Neurogenic bladder due to diabetic neuropathy leads to defects in bladder emptying
- Increased risk of asymptomatic bacteriuria and pyuria, cystitis and upper urinary tract infection.
- Enterobacteriaceae (e.g. E coli, Kliebsella and other coliforms), Pseudomonas aeruginosa

Describe Down’s Syndrome and Infection
An otherwise healthy person with Down’s Syndrome will probably not suffer many more serious infections than his or her siblings and will respond to vaccination.
Stereotypical belief that Respiratory tract infections (viral and bacterial) more common in young people with Down’s Syndrome
- ? Due to true immunodeficiency or to other factors e.g. altered mucus secretion or the structure of the mouth and airways
Describe Laboratory findings in Down’s Syndrome
[*] Laboratory observations in Down’s Syndrome – are they clinically relevant?
Humoral immunity
- Decreased neutrophil and monocyte function (chemotaxis, phagocytosis and the oxidative burst)
- Normal numbers of neutrophils and monocytes
- Lowered (in infants) or raised (in adults) immunoglobulin levels, in spite of normal B lymphocyte numbers
- Normal or raised levels of serum IgA and secretory IgA in older Down’s Syndrome children and adults
- Lowered specific antibody responses upon immunisation
- Normal or raised levels of C3, C4 and C5
Cellular Immunity
- Altered distribution of T cell populations e.g. lower CD4/CD8 ratio but normal T cell numbers. ?abnormal thymic function?
- Lowered T cell function including the response to specific antigens and some mitogens
- Altered T cell intracellular signalling
- Abnormal cytokine production
- Lowering of some but not all NK cell functions but increased numbers of NK Cells.
Describe the role of Pseudomonas aeruginosa as an important organism in cystic fibrosis
[*] Most Pseudomonas strains are environmental organisms that can cause opportunistic infections in a healthcare environment.
[*] Pseudomonas aeruginosa (gram negative bacilli) is widespread in the environment, but rare in the flora of healthy individuals. Its carriage increases with hospitalization.
[*] Most places such as sink-traps, drains and flower vases can harbour Pseudomonas.
[*] Pathogenesis
- Produces cytotoxins and proteases (e.g. exotoxins A and S, haemolysis and elastase)
- Isolates from patients with Cystic Fibrosis produce a polysaccharide alginate that protects from opsonisation, phagocytosis and antibiotics in microcolonies.
- Alginate, pili and outer membrane protein mediate adherence
- Alginate production is associated with hypersusceptibiltiy to antibiotics, lipopolysaccharide deficiency, non-motility and reduced exotoxin production.
[*] Clinical Syndromes
- Chronic pulmonary infection in cystic fibrosis
- Septicaemia which has a high mortality and is a particular threat to neutropenic patients
- Rapidly progressive corneal infection and otitis externa
- Colonization of burns, followed by septicaemia
- Ecthyma gangrenosum, a destructive skin complication of bacteraemia
- Osteomyelitis, septic arthritis and meningitis
[*] Laboratory Diagnosis
- Culture on selective media containing cetrimide, irgasin and naladixic acid.
- Identification by biochemical testing
- Typing by pulse-field gel electrophoresis or multilocus sequence typing (MLST)
[*] Treatment: organisms are often resistant therefore treatment is guided by susceptibilities.
[*] Despite active research there is no effective vaccine available

