Session 3: Acute Sepsis Flashcards
Apply the infection model to a patient presenting with an acute Infection
The case: a 19-year old female student presents acutely unwell to the ED. Acute sepsis is part of the differential diagnosis. ED has a ‘sepsis bundle’ for urgent management of acute sepsis.
The history:
- fit and well until last then non-specifically unwell, temperature and chills
- This morning felt acutely unwell with fever, severe headache, nausea, weakness, general muscle aches, abdominal pain and eye pain on exposure to light (photophobia).
On examination:
- Pale, cool extremities
- Temp 39.5oC, pulse 110/min, BP 80/50mmHg
- Respiratory rate 35/min
- Widespread purpuric (non-blanching – not changing under tumbler) rash noted
- Neck stiffness is noted
- Mentally alert, GCS 15
- Immediately recognized as severe sepsis + probable meningitis
Meningococcal meningitis: the likely diagnosis
Define Bacteraemia, Septicaemia, Sepsis, Severe Sepsis and Septic Shock
- Bacteraemia is the presence of bacteria in the blood (+/- clinical features)
- Septicaemia is a clinical term meaning generalized sepsis, suggestive of a bloodstream infection
- Sepsis is the systemic response to infection and can be defined as: SIRS + Documented or Presumed infection
- Severe Sepsis = SIRS + organ dysfunction or organ hypoperfusion
- Hypotension, decreased urine output (due to impaired renal function)
- Septic shock = severe sepsis + persistently low blood pressure despite administration of intravenous fluids (significant medical emergency)
What urgent investigations need to be done if sepsis is suspected?
- Full blood count, Urea and electrolytes (looking at metabolic activity in terms of ions and urea). Look for signs of sepsis with raised white cell count and raised neutrophils.
- EDTA bottle for PCR
- Blood sugar
- Liver function Tests
- C-reactive protein (CRP): an acute phase protein raised in acute infections. The protein is produced by the liver. NON-SPECIFIC indicator of inflammation and infection.
- Clotting studies
- Blood gases
What is SIRS?
Systemic Inflammatory Response Syndrome (SIRS): a response to a non-specific insult e.g. ischaemia, trauma, infection etc
Two or more of:
- Temperature <36oC or >38oC
- Heart rate >90/min
- Respiratory rate: >20/min (or PACO2 <4.3kPa)
- WBC <4x109/L or >12x109/L
NB: Temperature, heart rate and respiratory are bedside examinations
Describe how microorganisms trigger the inflammatory cascade
Endotoxin binds to macrophages => Cytokines: Tissue Necrosis Factors and Interleukins e.g. TNF-alpha and IL-1 [LOCAL] {to stimulate inflammatory response to promote wound repair and recruit reticuloendothelial system) => Cytokines released into circulation [SYSTEMIC] {stimulating Growth Factor, macrophages and platelets. Goal is homeostasis} => Homeostasis NOT Restored {Cytokines lead to activation of humoral cascades and reticuloendothelial system – CIRCULATORY INSULT}

Explain about Sepsis and Coagulation
- Cytokines initiate production of thrombin and thus promote coagulation
- Cytokines also inhibit fibrinolysis
- Coagulation cascade leads to microvascular thrombosis and hence organ ischaemia, dysfunction and failure.
- Microvascular injury is the major cause of shock and multiorgan failure.
What is meant by phagocytosis?
In the blood stream or at the inflammatory site, the neutrophil comes into contact with invading microbes. The encounter initiates phagocytosis of the target. The neutrophil sends out extensions of its plasma membrane called pseudopodia which progressively enclose the particle into a phagosome inside the cell and an arsenal of cytotoxic chemicals and enzymes destroy it. This is known as phagocytosis.
What is the Sepsis 6?
- Deliver high flow oxygen
- Take blood cultures and other cultures, consider source control
- Administer empirical (best guess) IV antibiotics
- Measure serum lactate
- Start IV fluid resuscitation
- Commence accurate urine output measurement
Describe antibiotic treatment for sepsis
- an agent is likely to be active against the pathogens that cause meningitis in this age group (different in neonates and the elderly).
- An agent that penetrates into the CSF
Empiric choice is CEFTRIAXONE (3rd generation cephalosporin with broad spectrum activity + reaches blood in good concentration)
What are possible life-threatening complications of sepsis?
- Irreversible hypotension (life threatening particularly to blood, brain and kidney)
- Respiratory failure
- Acute kidney injury (renal failure)
- Raised intracranial pressure -> may lead to a long term impairment of CNS function
- Ischaemic necrosis of digits/hands/feet
How would you confirm the diagnosis of sepsis?
Blood culture (growing the bacteria to confirm and identify the bacteria causing the infection – takes at least 24 to 48 hours) PCR Lumbar puncture (if safe):
[*] Culture of cerebrospinal fluid (CSF)
[*] PCR of CSF
Describe examination of the CSF sample
- Lumbar puncture only performed after checking contraindications
- Urgent transport of CSF to laboratory (Glucose and protein estimation in biochemistry as different changes in response to different infections, microscopy and culture in microbiology)
- Appearance: turbidity and colour
- Microscopy WBCs, RBCs
- Gram stain
- Referral for PCR
Describe features of Neisseria Meningitidis
- Bacterial pathogen Neisseria meningitides is gram negative diplococcus and spread by direct contact with respiratory secretions (with either someone who is infected or someone who is colonized)
- Most people are harmlessly colonized (asymptomatic)
- In the unlucky few, rapidly progressive and potentially fatal disease if not recognized and treated promptly
Describe the mechanism of action of Neisseria Meningitidis
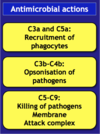
In this situation it attaches to the mucosa in the nasopharynx
- Endotoxins of lipopolysaccharides triggers inflammation
- Pilus enhances attachment
- Polysaccharide capsule promotes adherence to host and prevents phagocytosis from phagocytes within the host. Capsule is slippery
Numerous serogroups (e.g. A, B, C, W-135) based on the polysaccharide capsule antigen (evades immune response by preventing phagocytosis).
Outer membrane acts as an endotoxin

Describe the features of Meningococcal Disease
Up to 25% young adults may be carriers
Spread by aerosols and nasopharyngeal secretions
Acquisitions -> clearance, carriage or invasion
In England 1000 cases/ yr mainly Group B
Fatality rate ~10%
Elsewhere Group A predominates ‘meningitis belt’ across Africa
Describe the two types of prevention of Meningococcal Disease
Prevention 1. Vaccination
- Meningococcal C conjugate vaccine (introduced in the UK in 1999 and lead to dramatic decrease in Group C disease)
- ACWY vaccines available for immunocompromised patients and travel protection
- Serogroup B vaccine not yet in routine because the capsule is poorly immunogenic and similar to neural tissue (very difficult to introduce as a vaccine) however a vaccine has been developed after screening candidate proteins from genome studies and could be introduced into the UK within the next few years
Prevention 2: antibiotic prophylaxis
- Meningitis is a notifiable disease
- Cases reported to the local Health Protection Unit of Public Health England
- Close contacts (household, student accommodation) can be given antibiotic prophylaxis and considered for vaccination, all to try and clear any carriage of the organism to prevent invasion.