S3) Cardiac Arrhythmias Flashcards
What is an arrhythmia?
- An arrhythmia is a heart condition arising due to disturbances in pacemaker impulse formation and/or contraction impulse conduction
- It results in a rate and/or timing of myocardial contraction that is insufficient to maintain normal CO
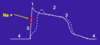
Describe the movement of ions in the fast cardiac action potential


Describe the effect of drugs blocking Na+ channels on the fast cardiac action potential

- Marked slowing conduction in tissue (phase 0)
- Minor effects on action potential duration (APD)
Describe the effect of beta blockers on the fast cardiac action potential

Diminish phase 4 depolarisation and automaticity

Describe the effect of drugs blocking K+ channels on the fast cardiac action potential

Increased action potential duration (APD)

Describe the effect of calcium channel blockers on the fast cardiac action potential

- CCBs decrease inward Ca2+ currents resulting in a decrease of phase 4 spontaneous depolarization
- Effect plateau phase of action potential

Describe the movement of ions in the slow cardiac action potential


Outline the mechanisms of arrhythmogenesis due to abnormal impulse generation

Outline the mechanisms of arrhythmogenesis due to abnormal conduction

Describe the two possible actions of anti-arrhythmic drugs in terms of abnormal generation
- Decrease the phase 4 slope (in pacemaker cells)
- Raises the threshold
Describe the two possible actions of anti-arrhythmic drugs in terms of abnormal conduction
- Decrease conduction velocity (phase 0)
- Increase ERP
Why are anti-arrhythmic drugs used?
Anti-arrhythmic drugs are used to:
- Decrease conduction velocity
- Change the duration of ERP
- Suppress abnormal automaticity
What are the different types of anti-arrhythmic drugs?
- Class I: Na+ channel blockers
- Class II: beta-adrenergic blockers
- Class III: K+ channel blockers (prolong repolarisation)
- Class IV: Ca2+ channel blockers
Describe the actions of the different types of class I anti-arrhythmic drugs
- Class IA – Moderate phase 0
- Class IB – No change in phase 0
- Class IC – Marked phase 0

Provide two examples of Class IA anti-arrhythmic agents
- Procainamide
- Quinidine
How are Class IA anti-arrhythmic agents administered?
- Oral preparation
- IV preparation
Describe the four effects of Class IA anti-arrhythmic agents on cardiac activity
- Decrease conduction – ↓ phase 0 of the action potential (Na+)
- Increase refractory period – ↑ APD (K+) and ↑ Na+ inactivation
- Decrease automaticity – ↓ slope of phase 4, fast potentials
- Increase threshold (Na+)
Describe the effects of Class IA anti-arrhythmic drugs on the ECG
- ↑ QRS
- ± PR
- ↑ QT

Describe the uses of Class IA anti-arrhythmic drugs
- Quinidine: maintain sinus rhythms in atrial fibrillation and flutter, prevent recurrence, Brugada syndrome
- Procainamide: acute IV treatment of supraventricular and ventricular arrhythmias
Identify 5 side-effects of Class IA anti-arrhythmic drugs
- Hypotension (reduced CO)
- Proarrhythmia e. g. Torsades de Points (↑ QT interval)
- Dizziness & confusion
- Gl effects (common)
- Lupus-like syndrome (esp. procainamide)
Provide two examples of Class IB anti-arrhythmic drugs
- Lidocaine
- Mexiletine
How are Class IB anti-arrhythmic agents administered?
- Lidocaine: IV preparation
- Mexiletine: oral preparation
Describe the five effects of Class IB anti-arrhythmic agents on cardiac activity
- Fast binding offset kinetics
- No change in phase 0 in normal tissue (no tonic block)
- APD slightly decreased (normal tissue)
- ↑ increase threshold (Na+)
- ↓ phase 0 conduction in fast beating or ischaemic tissue
Describe the effects of Class IB anti-arrhythmic drugs on the ECG
- No effects in normal / fast beating / ischaemic
- ↑ QRS

Describe the uses of Class IB anti-arrhythmic drugs
- Acute use in ventricular tachycardia (esp. during ischaemia)
- Not used in atrial arrhythmias or AV junctional arrhythmias
Identify 3 side-effects of Class IB anti-arrhythmic drugs
- Less proarrhythmic than Class 1A
- CNS effects: dizziness & drowsiness
- Abdominal upset
Provide two examples of Class IC anti-arrhythmic drugs
- Flecainide
- Propafenone
How are Class IC anti-arrhythmic agents administered?
- Oral preparation
- IV preparation
Describe the four effects of Class IC anti-arrhythmic agents on cardiac activity
- Very slow binding offset kinetics (>10 s)
- Substantially ↓ phase 0 (Na+) in normal
- ↓ automaticity (↑ threshold)
- ↑ APD (K+) and ↑ refractory period (esp in rapidly depolarising atrial tissue)
Describe the effects of Class IC anti-arrhythmic drugs on the ECG
- ↑PR
- ↑QRS
- ↑QT

Describe the uses of Class IC anti-arrhythmic drugs
Wide spectrum use:
- Supraventricular arrhythmias (fibrillation and flutter)
- Premature ventricular contractions (caused problems)
- Wolff-Parkinson-White syndrome
Identify 4 side-effects of Class IC anti-arrhythmic drugs
- Proarrhythmia and sudden death (esp chronic use)
- Increase ventricular response to supraventricular arrhythmias (flutter)
- CNS effects
- GI effects
Provide two examples of Class II anti-arrythmic agents
- Propranolol
- Bisoprolol
How are Class II anti-arrhythmic agents administered?
- Propranolol: Oral, IV
- Bisoprolol: Oral
Describe the two effects of Class II anti-arrhythmic agents on cardiac activity
- ↑ APD and refractory period in AV node to slow AV conduction velocity
- ↓ Phase 4 depolarisation (catecholamine dependent)
Describe the effects of Class II anti-arrhythmic drugs on the ECG
- ↑PR
- ↓HR

Describe the uses of Class II anti-arrhythmic drugs
- Treating sinus and catecholamine-dependent tachycardia
- Converting re-entrant arrhythmias at AV node
- Protecting the ventricles from high atrial rates (slow AV conduction)
Identify 2 side-effects of Class II anti-arrhythmic drugs
- Bronchospasm
- Hypotension
Don’t use in partial AV block or heart failure
Provide an example of a Class III anti-arrythmic agents
Amiodarone
How are Class III anti-arrhythmic agents (amiodarone) administered?
- Oral preparation
- IV preparation
Describe the four effects of Class III anti-arrhythmic agents on cardiac activity (amiodarone)
- ↑ refractory period and ↑APD (K+) ↓ phase0 and conduction (Na+)
- ↑ Threshold
- ↓ Phase 4 (β block and Ca2+ block)
- ↓ Speed of AV conduction
Describe the effects of Class III anti-arrhythmic drugs on the ECG (amiodarone)
- ↑ PR
- ↑ QRS
- ↑ QT
- ↓ HR

Describe the uses of Class III anti-arrhythmic drugs (amiodarone)
Very wide spectrum: effective for most arrhythmias
Identify 6 side-effects of Class III anti-arrhythmic drugs (amiodarone)
- Pulmonary fibrosis
- Hepatic injury
- Increase LDL cholesterol
- Thyroid disease
- Photosensitivity
- Optic neuritis (transient blindness)
Provide two examples of Class IV anti-arrythmic agents
- Verapamil
- Diltiazem
How are Class IV anti-arrhythmic agents administered?
- Verapamil: oral/IV preparation
- Diltiazem: oral preparation
Describe the three effects of Class IV anti-arrhythmic agents on cardiac activity
- Slow conduction through AV (Ca2+)
- ↑ Refractory period in AV node
- ↑ Slope of phase 4 in SA to slow HR
Describe the effects of Class IV anti-arrhythmic drugs on the ECG
- ↑ PR
- ± HR (depending on BP response and baroreflex)

Describe the uses of Class IV anti-arrhythmic drugs
- Control ventricles during supraventricular tachycardia
- Convert supraventricular tachycardia (re-entry around AV)
Identify 2 side-effects of Class IV anti-arrhythmic drugs
- Asystole (if β blocker is on board)
- Some GI problems
Caution when partial AV block, hypotension, decreased CO or sick sinus present
How can adenosine be administered?
Rapid IV
Describe the mechanism in which adenosine functions
- Binds α1 receptors and activates K+ currents in AVN & SAN
- ↓ APD, hyperpolarization → ↓HR
- ↓ Ca2+ currents – ↑ refractory period in AVN
Describe the effect of adenosine on cardiac activity
Slows AV conduction
Describe the uses of adenosine
- Convert re-entrant supraventricular arrhythmias
- Hypotension during surgery
- Diagnosis of CAD
Describe the mechanism in which digoxin functions
- Enhances vagal activity (↑K+ currents, ↓Ca2+ currents, ↑refractory period)
- Slows AV conduction and slows HR
Describe the use of digoxin
Digoxin is used in treatment to reduce ventricular rates in atrial fibrillation and flutter


