S1) Developing Medicines and Clinical Trials Flashcards
Identify the different stages in drug development as well as their associated duration
- Discovery research (4 years)
- Phase 1 (1 year)
- Phase 2 (2 years)
- Phase 3 (4 years)
- Regulatory review (1 year)
- Phase 4
Describe what is involved in the 4 years of discovery research in drug development
- Medicinal chemistry
- Biological testing
- Pharmacology
- Toxicology
Describe what is involved in the phase 1 of drug development
- Evaluates pharmacokinetics and safety with 50 healthy volunteers
- Lasts 1 year
Describe what is involved in the phase 2 of drug development
- Evaluates pharmacology in disease in 200 - 400 patients with target disease
- Lasts 2 years
Describe what is involved in the phase 3 of drug development
- Comparison with standard treatments
- Evaluates efficacy in target population and provides longer term safety data using 1000 - 3000 patients
- Lasts 4 years
Describe what is involved in the regulatory review in drug development
- Authority review of efficacy and safety
- Lasts 1 years
Describe what is involved in the phase 4 of drug development
- Monitoring for adverse reactions
- New indications or formulations in < 10 000 patients
Name the five processes which occur in discovery research in drug development
- Idea/concept phase
- Feasibility
- Target validation
- Identification of potential compounds (leads)
- Selection of candidate drug
What is involved in the idea/concept phase of discovery research in drug development?
- Therapeutic indication identified (disease approach)
- Potential molecular targets identified (mechanism approach)
- Assessment of medical/scientific/commercial opportunity
What is involved when considering the feasibility of discovery research in drug development?
- Model development
- Hypotheses generation
- Relevance to humans
- Screen evaluation
What is involved in the target validation of discovery research in drug development?
- Screens developed and validated
- Screening
- Hits (potential drugs) identified and evaluated
- Synthetic feasibility assessed (chemistry)
- Lead drug development and optimisation approach determined
What is involved when identifying potential compounds in discovery research in drug development?
- Potency and selectivity optimised
- PK and metabolism optimised
- Early assessment of toxicity
- Physical chemical properties and technical issues assessed
What is involved when selecting a candidate drugs in discovery research in drug development?
- Animal toxicology and preclinical safety pharmacology
- Toxicology studies (1 month/or longer) to support next phase
- Pre-formulation package and drug product supply
- Clinical and regulatory development plan & methodology studies
With reference to drug action, what does the statement ‘scientifically proven to work’ mean?
“It is better than the other treatment” i.e. more people receiving this treatment are cured than those on the other treatment

What is a clinical trial?
A clinical trial is any form of planned experiment which involves patients and is designed to elucidate the most appropriate method of treatment for future patients with a given medical condition
What is the purpose of a clinical trial?
The purpose of a clinical trial is to provide reliable evidence of treatment efficacy and safety
What is efficacy?
Efficacy is the ability of a healthcare intervention to improve the health of a defined group under specific conditions
What is safety?
Safety is the ability of a health care intervention not to harm a defined group under specific conditions
In order to be able to give a fair comparison of effect and safety, which three features must a clinical trial have?
- Reproducible – in experimental conditions
- Controlled – comparison of interventions
- Fair – unbiased without confounding
What are non-randomised clinical trials?
Non-randomised clinical trials involve the allocation of patients receiving a new treatment to compare with a group of patients receiving the standard treatment
What are the two disadvantages of non-randomised clinical trials?
- Allocation bias – by patient, clinician or investigator
- Confounding – known and unknown
What are the three steps involved in a randomised controlled trial (RCT)
- Definition of factors
- Conduct of the trial
- Comparison of outcomes
Identify the 6 factors which need to be defined in an RCT
- The disease of interest
- The treatments to be compared
- The outcomes to be measured
- Possible bias and confounders
- The patients eligible for the trial
- The patients to be excluded from the trial
What are the seven sub-steps in conducting a RCT?
⇒ Identify a source of eligible patients
⇒ Invite eligible patients to be in the trial
⇒ Consent patients willing to be in the trial
⇒ Allocate participants to the treatments fairly, i.e. without bias or confounding
⇒ Follow-up participants in identical ways
⇒ Minimise losses to follow-up
⇒ Maximise compliance with treatments
Which four questions might one ask when comparing outcomes in an RCT?
- Is there an observed difference in outcome between the treatment groups?
- Could the observed difference have arisen by chance, i.e. is it statistically significant?
- How big is the observed difference between the treatment groups, i.e. is it clinically important?
- Is the observed difference attributable to the treatments compared in the trial?
Provide 3 reasons for pre-defining outcome measures before the start of a clinical trial
- Prevent ‘data dredging’, ‘repeated analyses’
- Protocol for data collection
- Agreed criteria for measurement and assessment of outcomes
Identify three types of clinical outcomes and provide examples for each
- Patho-physiological e.g. tumour size, thyroxine level, ECG changes
- Clinically defined e.g. mortality, morbidity, disability
- Patient-focused e.g. quality of life, psychosocial well-being, satisfaction
Describe the timing of measurements in a clinical trial
- Baseline measurement of relevant factors – monitoring for inadvertent differences in groups
- Monitoring outcomes during the trial – monitoring for possible effect / adverse effects
- Final measurement of outcomes – comparing final effect of treatments in trial
What are the two advantages of random allocation?
- Minimal allocation bias – randomisation gives each participant an equal chance of being allocated to each of the treatments in the trial
- Minimal confounding – in the long run, randomisation leads to treatment groups that are likely to be similar in size and characteristics by chance
Blinding/masking is a method to ensure minimal allocation bias.
What are the two types of blinding?
- Single blind – one of patient, clinician, assessor does not know the treatment allocation
- Double blind – two of patient, clinician, assessor does not know the treatment allocation (usually patient + clinician/assessor)
(usually patient)
Identify five situations where blinding is difficult to achieve
- Surgical procedures
- Psychotherapy vs. anti-depressant
- Alternative medicine vs. Western medicine
- Lifestyle interventions
- Prevention programmes
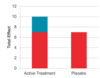
What is the effect of comparing with ‘no treatment’
The effect of comparing a ‘new treatment’ group with a group receiving no treatment is to leave one unsure as to whether any observed difference was due to the ‘new treatment’ or to the fact that the group was receiving care
What is the placebo effect?
The Placebo Effect – “even if the therapy is irrelevant to the patient’s condition, the patient’s attitude to his or her illness, and indeed the illness itself, may be improved by a feeling that something is being done about it”
What is a placebo?
A placebo is an inert substance made to appear identical in every way to the active formulation with which it is to be compared e.g. appearance, taste, texture, dosage regime, warnings, etc
What is the purpose of a placebo?
The aim of a ‘placebo’ is to cancel out any ‘placebo effect’ that may exist in the active treatment
The use of a placebo is a form of deception.
Hence, what are the ethical implications for this?
- A placebo should only be used when no standard treatment is available
- Participants in a placebo-controlled trial are informed that they may receive a placebo
What leads to losses to follow-up i.e. not every participant remains in the clinical trial?
- Their clinical condition may necessitate their removal from the trial (appropriate)
- They may choose to withdraw from the trial (unfortunate)
Suggest four ways that might help minimise losses to follow up in clinical trials
- Make the follow-up practical and minimise inconvenience
- Be honest about the commitment required from participants
- Avoid coercion or inducements
- Maintain contact with participants
What leads to non-compliance to treatment in patients?
- They may have mis-understood the instructions
- They may not like taking their treatment
- They may think their treatment is not working
- They may prefer to take another treatment
Suggest four ways that might help maximise compliance with treatments
- Simplify the instructions
- Ask about compliance
- Ask about effects and side-effects
- Monitor compliance e.g. tablet count, urine level, blood level
Explain how one might conduct an explanatory trial – ‘as-treated’ analysis
- Analyses only those who completed follow-up and complied with treatments
- Compares the physiological effects of the treatments
- Loses effects of randomisation → selection bias and confounding

Explain how one might conduct an pragmatic trial – ‘intention-to-treat’ analysis
- Analyses according to the original allocation to treatment groups, regardless of compliance/completion
- Compares the likely effects of using the treatments in routine clinical practice
- Preserves effects of randomisation → minimal selection bias and confounding

Clinical trials should normally be analysed on an ‘intention-to-treat’ basis.
Why is this?
- ‘As-Treated’ analyses tend to give larger sizes of effect
- ‘Intention-to-Treat’ analyses tend to give smaller and more realistic sizes of effect
What is the principle of collective ethic?
Collective ethic – all patients should have treatments that are properly tested for efficacy and safety
What are the principles of individual ethic?
- The principle of beneficence
- The principle of non-maleficence
- The principle of autonomy
- The principle of justice
Explain collective ethic in terms of randomised controlled trials
Collective ethic – RCTs aim to properly test treatments for efficacy and safety
Explain individual ethic in terms of randomised controlled trials
- RCTs do not guarantee benefit
- RCTs may result in harm
- RCTs allocate treatment by chance
- RCTs place burdens and confer benefits
Which issues should be considered for a clinical trial to be ethical?
- Clinical equipoise
- Scientifically robust
- Ethical recruitment
- Valid consent
- Voluntariness
What is clinical equipoise?
Clinical equipoise is when there is reasonable uncertainty or genuine ignorance about the better treatment or intervention (including non-intervention)
Which 8 features make a trial scientifically robust?
- Addresses a relevant issue
- Asks a valid question
- Has an appropriate study design and protocol
- Has the potential to reach sound conclusions
- Can justify the use of the comparator treatment or placebo
- Has acceptable risks of possible harm compared to anticipated benefits
- Has provision for monitoring the safety participants
- Has arrangements for appropriate reporting and publication
Identify two issues with ethical recruitment
- Inappropriate exclusion
- Inappropriate inclusion
In terms of ethical recruitment, provide two scenarios demonstrating inappropriate exclusion
- People who differ from an ideal homogenous group e.g. non-White people, women, co-morbidities (usually elderly)
- People who are difficult to get valid consent from e.g. immigrants, mentally ill, children, prisoners
In terms of ethical recruitment, provide two scenarios demonstrating inappropriate inclusion
- Participants from communities that are unlikely to benefit e.g. AIDS drugs trials in LEDCs
- Participants with a high risk of harm with respect to potential benefits
- e.g. pregnant women*
- Participants likely to be excluded from analysis e.g. a small sub-group of Chinese
Describe the six steps involved to attain valid consent
⇒ Knowledgeable informant
⇒ Appropriate information (verbal, written, freedom to opt out)
⇒ Informed participant
⇒ Competent decision-maker
⇒ Legitimate authoriser
⇒ Signed consent form as evidence of valid consen
What is voluntariness?
Voluntariness is a pre-requisite for consent to be valid, i.e. the decision should be free from coercion or manipulation
Perceived coercion or manipulation invalidates consent as much as actual coercion or manipulation.
Provide some examples of coercion
- Non-access to ‘best’ treatment
- Lower quality of care
- Disinterest by clinician
Perceived coercion or manipulation invalidates consent as much as actual coercion or manipulation.
Provide some examples of manipulation
- Exploitation of emotional state
- Distortion of information
- Financial inducements
What is the purpose of a research ethics committee?
- Research governance
- Financial management
- Resource implications


