Rx Cardio Flashcards
What is the most common cause of mitral stenosis
Rheumatic heart disease
- d/t group A strept pharyngitis (S. pyogenes)
- Sx RHD- fever, carditis, migratory polyarthritis, chorea, erythema marginatum.
- RHD –> can lead to (many yrs later) chronic RHD, –> cause mitral stenosis.
- The pathogenesis of disease is related to molecular mimicry: Abs directed against strept Ags cross-react w/ host antigens on the cardiac valves.
The term pulmonary capillary wedge pressure is equivalent to
preload
When vignette says pt has multiple punctate lesion on arms, what is the 1st think you think of?
IV drug use!!!
Organisms associated with IV drug use?
- S. aureus
- Tricuspid valve Endocarditis
- Pnemonia
- Osteomyelitis
- S. pneumoniae
- Pneumonia
- Candida albicans
- Tricuspid valve endocarditis
- Osteomyelitis
- Pseudomonas
- Tricuspid valve endocarditis
- Osteomyelitis
- HTLV
- Adult T cell lymphoma (neoplasma of mature T cells)
Diseases
- Pneumonia
- S. aureus
- S.pneumoniae
- Tricuspid valve endocarditis (Don’t “TRI drugs”)
- S. aureus
- Candida albicans
- Pseudomonas
- Adult T-cell lymphoma
- HTLV
- Osteomyelitis
- Pseudomonas
- Candida
- S.aureus
- 24-yo m c/o fever, chills, night sweats, malaise, and fatigue that started 3 days ago.
- Past 24 hours, he has become SOB.
- G/A- shaking, pale.
- PE- temp 39.4°C (103°F), hypoxia to 88% on room air, B/L JVD. Decrbreath sounds at the bases of the lungs and systolic murmur tricuspid valve.
- Skin exam- mult punctate lesions on both forearms in various stages of healing from ecchymosis.
Diag?
Acute Bacterial Endocarditis
- Mult punctate lesions on arms in various stages of healing –> mean IV drug user
- S. aureus is most common bact pathogen isolated from these pts bc it is part of the skin flora and enters the blood at injection sites. Strep viridians for subacute
- Severe & sudden onset makes acute– high virulence (vs- subacute has more gradual onset– low virulence)
- New murmur also indications acute- bc acute is vegetations on previously normal valves (vs subacute- on abnormal or diseased valves)
- 67-yo m chest pain.
- pain started 3 hr ago when he was shoveling snow and resolved spontaneously on the ambulance.
- chest pain is “squeezing” rather than sharp. No similar episodes in the past.
- just finished eating a heavy meal (hamburger and fries) before shoveling snow.
- Pmhx- hyperlipidemia, hypertension, and GERD.
- He was otherwise healthy besides an upper respiratory infection 1 week ago.
- PE- no acute distress is noted. Temp normal, blood pressure is 160/80 mm Hg. HR is regular without murmurs. Lungs normal. No pedal edema.
- Labs- CK and troponin panel and EKG normal
Diag?
Most likely cause of rapidly resolving exertional chest pain in a pt with a hx of HTN and hyperlipidemia is stable angina secondary to coronary atherosclerosis.
-This patient’s normal EKG and undetectable cardiac biomarkers (troponins and creatine kinase-mb) further support this diagnosis.
What is most likely cause of rapidly resolving exertional chest pain in a patient with a history of hypertension and hyperlipidemia
stable angina secondary to coronary atherosclerosis.
Most common cause of stable angina
atherosclerosis (if pt hx HTN, hyperlipidemia)
-stable angina ( ≥ 70% occlusion), exertional chest pain resolves with rest of NG.
- tall, thin 25-year-old m w a hx of joint hyperflexibility c/o tearing chest pain that radiates to his back.
- BP is 90/45 mm Hg, his pulse is 123, and his RR 24.
PE- drop of 21 mm Hg in his systolic blood pressure during inspiration. Also distended neck veins and distant heart sounds.
Marfans syndrome –> which caused aortic dissection (sudden onset chest pain radiating to back) –> which caused cardiac tamponade
- Dissecting aortic aneurysm: sudden onset chest pain radiating to back. Mediastinal widening on CXR
- Cardiac tamponade
- Becks triad: hypotension, incr JVP, distant heart sounds
- EKG- Diffuse low voltage QRS
- Pulsus paradoxus = decr ampl of systolic BP by > 10 mmHg during inspiration
- Incr HR
- Floppy mitral valve
- Marfan EKG –> RA or RV collapse –> severe decr ventricular filling and CO –> oscillating QRS ampls
Sudden cardiac death in the setting of an MI is most commonly caused by ____?
Arrhythmias- in particular ventricular fibrillation (VF).
Pt sudden onset chest pain radiating to back with hx marfans
Diag?
Aortic dissection (longitudinal intimal tear forming a false lumen)
- 25-yo primigravid f for checkup.
- lightheadedness when she lies down in bed at night.
- BP is 120/70 mm Hg while she is sitting upright and 90/50 mm Hg while in the supine position.
- PE- shows a uterus consistent in size with 36 weeks’ gestation and edema in the lower extremities.
Diag?
IVC compression
The pt presentation of supine hypotension and peripheral edema in late pregnancy points to IVC compression. IVC compression is common in women during the third trimester of pregnancy. The enlarged uterus compresses the IVC on the right side, decreasing venous return to the heart. This reduction in preload reduces stroke volume, thereby reducing cardiac output.
-Because MAP = CO × TPR, an acute decrease in either of these parameters will reduce BP. Pregnant women can avoid this problem by placing a pillow under the right hip or by lying on the left side to remove the weight of the gravid uterus from the IVC.
Pregnant f w/ IVC compression
Tx?
-Because MAP = CO × TPR, an acute decrease in either of these parameters will reduce BP. Pregnant women can avoid this problem by placing a pillow under the right hip or by lying on the left side to remove the weight of the gravid uterus from the IVC.
Nitroprusside MOA
vasodilate by incr NO in vascular SM –> incr cGMP and SM relax
- can cause CN- poisoning bc releases Nitroprissode in body –> incr NO and incr CN-
- use for HTN emergencies (extremely high bp, headave, N/V)
What toxicity can you get from Sodium Nitroprusside
Cyanide tx
Bc in body nitroprusside –> incr NO and incr CN-
Sx of cyanide tox?
nonspecific signs and symptoms such as headaches, confusion, seizures, vomiting, arrhythmias, cherry-red–colored lips and mucous membranes, and later the development of cyanosis
Mechanism
-Cyanide has a high affinity for binding the ferric ion (Fe3+) in mitochondrial cytochrome C. Binding of cyanide to cytochrome C causes inhibition of mito cytochrome C oxidase, the last step in the ETC. This halts OxPhos and forces the body to switch to anaerobic metabolism for ATP production, leading to a lactic acidosis and a shortage of ATP. A small amount of cyanide also binds to the ferrous ion (Fe2+) in hemoglobin, forming a compound that cannot deliver oxygen to the tissues.
What causes inhibition of mitochondrial cytochrome C oxidase
Binding of cyanide to cytochrome C
Another name for digitalis
Digoxin
Digoxin MOA
Direct inhibition of Na/K ATPase –> which indirectly inhibits Na+/Ca+ exchanger –> incr intracellular Ca2+ –> positive inotropy (contraction)

pt has ST-segment elevation MI and COPD
-prescribed drug that acts by decreasing slope of phase 4 cariac pacemaker cells.
Which drug?
A cardioselective beta-1 blocker (ex- metoprolol)
-nonselective beta blocker is contraindicated bc COPD
β-Blockers beginning with the letters A through M are usually (but not always) β1 selective and primarily affect sympathetic input at the heart
Does NE cause tachy or brady?
Because norepinephrine acts with greater affinity for a-adrenergic receptors than ß-adrenergic receptors, this reflex bradycardia in response to a1-mediated vasoconstriction outweighs any ß1-mediated increase in heart rate, resulting in a net decrease in heart rate.
Which part of the jugular venous tracing should be absend in a pt with A-fib?

A-wave (“A- for atrial contraction)
Pt has supraventricular arrhythmia, started on new drug, now has hyperthyroid sx
-Which drug did pt start?
Amiodarone (type III antirhythmic = K+ channel blockers)
-Amiodarone is lipophilic and has class I,II,III,IV effects (so that’s why so many AEs)
Other AEs:
- pulmonary fibrosis
- hepatotox
- corneal deposits
- blue/grey skin deposits –> photodermatitis
- Neuro effects
- Constipation
- CV effects (brady, heart block, HF)
Amiodarone MOA
=type III antiarhythmic = K+ channel blockers
- block K+ channels –> longer effective refractory period and longer AP
- Whenever there is a K+ block–get QT prolong –> torsades
78 yo m
- chest pain and tightness on exertion, sx resolve w/ rest
- Auscultation heart and R sternal border– hear crescendo-decrescendo murmur (audio)
–> what condition?
Aortic stenosis– which is most commonly d/t age-relateed calcification
Most common cause of aortic stenosis
Age related calcifications
medication for refractory hypertension, which can lead to rebound hypertension urgency if it is abruptly stopped.
Clonidine (alpha-2 agonist)
- Pt has v-fib
- dr gave defillibration, then epi, still no improvement. What is next step?
If defibrillation fails to convert to sinus rhythm, epinephrine is given followed by amiodarone, according to the advanced cardiovascular life support (ACLS) protocol.
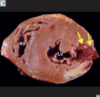
Diag?

Acute aortic dissection
In the image, note the presence of a dissection flap separating the aorta. The ascending aortic dissection is classically felt more as chest pain, whereas descending aortic dissection tends to be more classically felt as back (interscapular) or abdominal pain.
Most feared complication of aortic dissection
rupture into any body cavity, including the pericardial, pleural, or peritoneal spaces. Pericardial tamponade, leading to obstructive shock, is the cause of death in two-thirds of patients with rupture of a proximal aortic dissection. Hemorrhagic shock secondary to rupture is another common cause of death in patients with both proximal and distal aortic dissections.
- 67-yo f c/o 1-day hx of dizziness.
- The dizziness is present while she is sitting and on standing. During the interview, she experiences two episodes of near-syncope.
- Taking a medication for “heart troubles” but says she cannot remember its name.
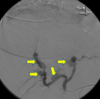
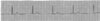
PE: reveals a frail woman in mild distress. BP 126/61 mm Hg, HR 210. Normal cardiac auscultation. Results of an ECG are shown in the image.
Diag?

Torsades de pointes
presents with dizziness and syncope, and she has hx of heart disease. The ECG demonstrates a pattern characteristic of torsades de pointes (TdP). Clinically, the rapid rate of TdP can manifest as palpitations, dizziness, and lightheadedness, as experienced by this patient. A variety of medications, including antiarrhythmics, antibiotics (eg, macrolides), antipsychotics (eg, haloperidol), antidepressants (eg, tricyclic antidepressants), and antiemetics (eg, ondansetron) can cause TdP.
-Given this patient’s history of “heart troubles,” she is most likely taking an antiarrhythmic that can cause torsades de pointes, such as the class 1A antiarrhythmic, quinidine.
- 45-yo f c/o 1-week hx of fever and passage of black stools.
- Pmhx: melena, long-term use IV drugs, prostitution, and long periods without medical care.
- PE: cachexia, diffuse abdominal pain, and tender erythematous nodules on her skin.
- V/S: temp of 38.7°C (101.6°F), BP of 170/110 mm Hg, R of 12/min.
- Labs: positive for hepatitis B surface antigen and hepatitis B core antibody. Neg for antineutrophil cytoplasmic antibodies
- Angiography of the renal arteries is performed, with relevant portions highlighted by the arrows (see image).
Diag?
Diag?
Polyarteritis Nodosa
- tender erythematous skin nodules, abdominal pain, renal insufficiency, and HTN. She has systemic signs and evidence of multisystem involvement, including GIT and renal symptoms
- (-) ANCA, making ANCA-positive vasculitis much less likely. ANCA-(+) vasculitis incl microscopic polyangiitis, granulomatosis with polyangiitis (Wegener), and eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome).
What type of hypersensitivity is polyarteritis nodosa?
Type III (IC-Ag/Ab)
What do you see in an EKG in pt w/ hyperkalemia
peaked T waves and a widened QRS interval and sinus bradycardia.

What are some signs of hyperkalemia?
ascending flaccid muscle paralysis, arrhythmias
-EKG: widened QRS and peaked T waves
What determines prognosis/ severity of tetrology of fallot?
Degree of pulmonary stenosis
- A baby girl, born 2 weeks ago
- baby seems to be “purple,” especially her fingers and toes
- She looks increasingly blue when she is crying.
- baby has had difficulty feeding and is at the 20th percentile for weight.
- PE: harsh systolic murmur at the left upper sternal border.
Diag?
Tetrology of fallot (see pulm infundibular stenosis)
- bc worsening cyanosis w/ agitation, and difficult feeding — these activities req more oxygen
- also cyanosis is early– so must be one of 5 Ts
Cardio AE of lithium exposure in utero
Ebstein anomaly
= displacement of tricuspid valve leaflets downward into RV (“atrialization” of RV)
Which drug exposure in utero causes neutral tube defects?
valproic acid (anticonvuslant)
What does alchol exposure in utero cause?
increases the risk for septal defects, including Eisenmenger syndrome, in the fetus.
What does carbamazepine exposure in utero cause
Cleft palate
carbamazepine is antiepileptic)
- 17-yo m
- BP is 210/130 mmHg in the left arm. BP in the right arm is 205/128 mmHg.
- normal S1 and S2 heart sounds without any murmurs, gallops, or rubs.
- Clear lungs. No peripheral edema is noted. Muscle strength is a 5/5 in all extremities. Distal pulses are all 2+.
- BP in the right thigh is 105/60 mm Hg.
Diag?
Coarctation of aorta
- large difference between the brachial and tibial blood pressures
- Coarctation of the aorta is a congenital narrowing of the aorta near the site of the ligamentum arteriosum (as illustrated in the diagram). The mechanical obstruction leads to a higher blood pressure proximal to the narrowing to maintain sufficient pressure distal to the coarcted segment.
- The result may be severe hypertension in the head, upper torso, and upper extremities and hypotension in the lower extremities.
- Compl: An ascending aortic dissection is most closely associated with isolated systemic HTN, as seen in this patient

Failure of the aorticopulmonary septum to spiral causes which disease?
Transposition of the great vessels

2 conditions highly associated with coarctation of the aorta?
- Turner (short stature, a webbed neck, streak ovaries, and primary amenorrhea. The genetics is XO)
- Bicuspid aortic valve
Juxtaductal vs postductal coarctation of aorta
Juxta ductal = distal to the origin of the left subclavian artery and opposite the ductus arteriosus. If the left subclavian artery is involved, juxtaductal coarctation of the aorta can result in a small left arm because of compromised blood flow. assoc w/ turners
post ductal is not assoc w/ turners, and will have upper extremity signs and sx
- 12-yo f
- generalized aching pain in both of her knees 2wk ago, which have since moved to her right shoulder & elbow and today is in both wrists.
- was sick with a sore throat just 1 mo ago but recovered completely.
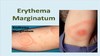
- PE: redness of the skin with pink rings on the torso and inner surfaces of the limbs.
Diag
Rheumatic fever
- Jones criteria
- Red skin with pink rings on torso (erythema marginatum)
- joint pain that migrates (migratory polyarthritis)
- Pancarditis
- SubQ nodules
- Syndenham chorea
- Incr serum ASO titers
- Mitral stenosis 20 years later
- Murmur = opening snap then delayed low pitch/ rumbling diastolic murmur
- LA >> LV pressure
- D/t group A strept (pyogenes)
- See aschoff bodies on myocardial tissue bx
Which conditions cause a holocystolic murmur
- Mitral or tricuspid regurg: high pitched blowing murmur
- Mitral– loudest at apex. usually d/t ischemic heart disease (post-MI), MVP, LV dilation
- Tricuspid- loudest at tricuspid valve. Caused by RV dilation
- Rheumatic fever and IE— cause mitral or tricuspid regurg
- VSD: harsh murmur, best heard at tricuspid area
- PDA: continuous “machine-like” murmur
harsh, blowing II/VI holosystolic murmur, best heard at the left sternal border
Diag?
VSD
The start of the aorta sits (ant/post) to the pulmonary artery
post

- A baby boy is delivered to a healthy mother.
- 1 hr after delivery, the infant is pale, cold extremities, breathing rapidly with subcostal retractions.
- The newborn is started on supplemental O2, but his color does not improve. -BP 70/50 mm Hg, pulse 176/min, and R 59/min.
- ECG: an aorta sitting anterior to the pulmonary artery. There is no atrial septal defect and only a very small ventricular septal defect.
Diag?
Transposition of great vessels
-normally pulmonary artery should be anterior to aorta

How to prevent death in baby with transposition of great vessels
Need a way to mix oxygenated and deoxygenated blood.
- PDA: Give PGE in order to keep the ductus arteriosis open.
- VSD
- Patent foramen ovale

Name the cutaneous skin finding found in rheumatic heart disease
Erythem marginatum
- kinda looks like lyme disease
- JONES criteria
= a nonpruritic, macular, annular, erythematous eruption that occurs in a minority of patients with acute rheumatic fever. Rheumatic fever is a consequence of pharyngeal infection with group A Strept, usually in childhood.
Myocardial bx
What does histo show?
Diag?
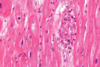
Rheumatic Heart Disease

Valsalva menuever accentuates wich murmur?
MVP
- makes earlier onset/click murmur
- MVP murmur = last systolic crescendo murmur w/ midsystclick
late diastolic murmur preceded by an opening snap
Mitral stenosis
-get from rheumatic heart disease – d/t untreated group A strept pharyngitis (not d/t IE)

A 25-yo m c/o feeling faint during weekly game of basketball for 1 mo.
- last week he became SOB, and almost passed out while playing fetch with his dog.
- brother passed from drowning while swimming
- PE: soft S4 gallop can be auscultated at apex, and mild systolic ejection murmur is noted at the L lower sternal border. This murmur decreases in intensity when he squats, and increases w/ Valsalva maneuver.
- CXR- normal size heart
Hypertrophic CM
- Murmur = systolic ejection murmur (also see w/ aortic stenosis) but here at L sternal border and aortic stenosis at aortic valve
- valsalva increases intensity of murmur
- familial, so see family hx (AD)
- Presents
- Syncope during exercise –> lead to sudden death (in young athletes)
- see S4
- LV hypertrophy
- Tx: beta-block or non dihydro CCBs (ex verapamil)

Tx for HCM
- Beta block (ex atenolol) – bc reduces contractility and lowers HR –> incr ventricular filling
- Non-dihydro CCBs (ex verapamil)-

late diastolic murmur and a diminishing S1 sound are heard
Mitral stenosis
- opening snap then rumbling (low pitch) diastolic murmur
- d/t rheumatic heart disease
In what condition do you see anitschow cells?
rheumatic heart disease
-has catepillar nu
Pathologic features of RHD include Aschoff bodies, which contain multinucleated giant cells and large Anitschkow cells.
RHD –> lead to mitral stenosis, which is characterized by a late diastolic murmur and diminished S1 sound.

- 4 yo m
- harsh, blowing holosystolic murmur, best heard at the left sternal border
VSD
- most common congenital anomaly
- also tricuspid regurg around this area
Its harshness can be a rough indicator of size; they are inversely proportional. The murmur of smaller VSDs sounds harsher than larger ones

Blowing early diastolic murmur
aortic regurg
Aortic regurg can progess to ___?
L HF
- orthopnea
- dyspnea
- B/L crackles
- 81 yo m
- several months dyspnea on exertion and fatigue
- viral URI recently
- PE: low ampl carotid pulse
diag?
Aortic stenosis
- murmur = crescendo-decrescendo systolic ejection murmur
- pulsus parvus et tardus = carotid pulses weak
- can lead to (SAD) Syncope, Angina, Dyspnea. (L-HF?)
- d/t age related calcification (of valve cusps) in older pts (>60yo)

- IV drug user
- “blowing” systolic heart murmur is heard that is loudest at the left lower sternal border
diag?
tricuspid regurg
While tricuspid regurgitation may be caused by right ventricular dilatation, the tricuspid valve is also the most common site of infective endocarditis in intravenous drug users. In these patients, infected venous blood (most often with S. aureus) returns to the right side of the heart, and seeds the tricuspid valve.
Pt has pyelonephritis –> that lead to acute kidney injury (AKI)
What do you see on ECG?
Peaked T waves
-AKI can make the kidneys unable to properly secrete K+ in the urine, leading to hyperkalemia. Untreated, hyperkalemia can lead to ECG changes, most notably peaked T waves (shown below)

Which post MI complication happens 2–7 days after an MI
Papillary muscle rupture

Which post MI complication happens 3-14 days after an MI
ventricular free wall rupture
-then LV failure is a late sequelae of post MI comp
Which post MI complication happens 3-5 days after an MI
IV septal rupture
When do you see “U” waves in ECG?
Marked hypokalemia
-d/t conditions that result in the overstimulation of RAAS. Oversecretion of aldosterone leads to increased secretion of K+ into the urine, leading to hypokalemia.
- 9-yo f has arrhythmia that started while she was sitting in class.
- was diagnosed at birth with a disorder that predisposes her to arrhythmias.
- An ECG is obtained (see tracing)
diag?

Wolff-Parkinson-White (WPW) syndrome
- The patient presents with an arrhythmia, and her history indicates she was diagnosed at birth with a disorder that predisposes her to arrhythmias. It is likely that she has WPW
- WPW is characterized by an atrioventricular (AV) accessory tract that bypasses the AV node and goes straight from the atrium to the ventricle (see figure below).
- Characteristic ECG findings include a short PR interval, long QRS interval, and up-sloping”delta wave” of the early QRS complex.
What does EKG show?
3rd degree heart block
-can get heard block from lyme disease

Granulomatous inflammation of myocytes is the mechanism of injury causing _______
restrictive or dilated cardiomyopathy in sarcoidosis.
-Cardiac sarcoidosis should be considered in an otherwise healthy young or middle-aged person with cardiac symptoms, or a pt w/ known sarcoidosis who develops arrhythmias, conduction disease, or CHF. Diag depends on evidence of the multisystem features of sarcoidosis, and bx showing noncaseating granulomas
- 35 yo f
- presents with SOBon activity, swollen legs, a recent URI, crackles on his lungs bilaterally, S3 gallop.
- CXR below
Diag?

Dilated cardiomyopathy –> CHF
- most likely cause of the patient’s DCM is viral myocarditis following his URI several weeks before. Myocarditis causes DCM from autoimmune attack.
- characterized by dilation and impaired contraction of one or both ventricles.
- DCM is autoimmune damage to cardiac myocytes
- Causes: alcohol abuse, myocarditis, ischemic disease, HTN, HIV infection, connective tissue disease. It may also be idiopathic, or doxorubicin (chemo agent)
- In about 30% to 50% of patientss, DCM is caused by gene mut

Etiology of Hypertrophic CM
mutations in sarcomere genes, such as the β-myosin heavy chain
-is an autosomal dominant condition assoc with asymmetric ventricular wall enlargement. It can lead to sudden death in young athletes.
-smoker, HTN-non compliant, DM
Autopsy heart below
Diag?

Systemic HTN (not pulm HTN)
- In this image, the LV is much thicker than expected, suggesting concentric hypertrophy of the myocardium. Also, this thickness is symmetrical, confirming the finding of hypertension. (Aortic valve and mitral valve insufficiency –> eccentric hypertrophy and a dilated LV)
- LV concentric hypertrophy can be a compl of long-standing HTN. The result is diastolic dysfunction, since the incr muscle mass in the LV prevents appropriate relaxation during diastole.
- Systemic HTN results in an incr afterload, putting more strain on the LV as it pumps out blood against an incr pressure. Therefore, the LV undergoes concentric hypertrophy and incr its muscle mass to maintain a normal EF against an incr afterload.
-has tachy, palpitations, lightheadedness
Diag?

Wolf parkinson white
- ECG shows intermittent tachycardia along with wide QRS complexes associated with relatively short PR intervals and slurring upstroke of the initial parts of the QRS complexes.
- caused by Atrioventricular bypass tract (a conduction pathway from atria to ventricle (ie, an accessory pathway, known as the bundle of Kent))

Effect of digoxin on starling curve
-below is normal starling curve

Digoxin, a positive inotrope, shifts the curve up and to the left because increased contractility increases the stroke volume.



