Rectal Tears / Rectal Prolapse Flashcards
Rectal tears mostly affect _____, while rectal prolapse is mostly a problem of _____.
Rectal tears mostly affect horses, while rectal prolapse is mostly a problem of ruminants.
What are the different causes of rectal tears?
- Iatrogenic
- Spontaneous (post-foaling)
- Other (enema, meconium extraction with forceps, etc)
TRUE/FALSE
Rectal tears post foaling are evidence of dystocia.
FALSE
Iatrogenic rectal tears usually occur on the ____ part of the rectum.
DORSAL
How are rectal tears diagnosed?
- Sudden release of pressure
- Sudden ability to palpate abdominal organs distinctly (rare)
- Blood on sleeve
What drugs/methods are used to stop rectal contractions while confirming rectal tears with your bare hand (gross)?
- Epidural
- Xylazine
- Butorphanol
- Buscopan
- Lidocaine Enema or gel
Other than palpating with your poor gloveless hand, what are other ways to confirm rectal tears?
- Speculum examination of rectum to visuaize mucosa
- CBC or abdominocentesis (changes may not be seen right away)
How can you prevent rectal tears?
- Copious lubrication
- Adequate restraint: Sedation if necessary
- Muscle relaxant: Buscopan (Small dose ~ 3 mL; 60 mg)
- Don’t try to palpate beyond your reach
GRADE IT: Rectal Tears
Tissue Affected:
- Mucosa
- Submucosa

Grade 1
GRADE IT: Rectal Tears
Tissue Affected:
- Muscular layer disrupted
- Mucosa and submucosa may prolapse into defect and provide site for fecal impaction

GRADE 2
GRADE IT: Rectal Tears
Tissue Affected:
All except serosa

GRADE 3A
GRADE IT: Rectal Tears
Tissue Affected:
- All except serosa
- Mesorectum and retroperitoneal tissue

GRADE 3B
GRADE IT: Rectal Tears
Tissue Affected:
- All layers into abdomen
- May be associated with prolapse of small colon or small intestine through defect
*Horse can develop sepsis/peritonitis in relation to this tear

GRADE 4
Location of Rectal Tears:
- Most tears are ____ & ____.
- Usually _____cm from anus
*Distance from anus not a good indicator of tear location
relative to retroperitoneal ref lection and abdominal
cavity
- Most tears are dorsal & longitudinal
- Usually 15 to 55 cm from anus
Idiopathic tears may simply present as ____ and pass
unnoticed for some time because tear is not suspected.
Idiopathic tears may simply present as colic and pass
unnoticed for some time because tear is not suspected.
Signs of Rectal Tears:
- May be ______ in Grade 1
- ________ and _______within a few hours in more serious cases
- Feces may be ______ initially
- May be asymptomatic in Grade 1
- Peritonitis and toxic shock within a few hours in more serious cases
- Feces may be hemorrhagic initially
What is the initial treatment in severe cases showing signs septic shock and peritonitis?
- Flunixin
- Intravenous fluids
- Antibiotics (Penicillin, gentamicin, metronidazole)
What are initial treatment options for rectal tears?
- Treat septic shock and peritonitis
- Reduction of rectal motility
- Epidural anesthesia to allow gentle removal of feces
- Gentle packing of rectum
- Referral
What is the purpose of gently packing the rectum for initial treatment of rectal tears?

- Protect tear
- Prevent contamination of abdomen
- Prevent conversion of Grade III to Grade IV
Non-Surgical Treatment: Grade I or II
- _______ and ______ sufficient for Grade I
- ______ alone may be sufficient for the smallest lesions
- Soften feces with______
- Antibiotics and Flunixin sufficient for Grade I
- Observation alone may be sufficient for the smallest lesions
- Soften feces with Mineral oil / bran mashes / green grass / moistened pellets - not preferred by Gilbert because increased chance of leaking and more difficult to evacuate than pellets
Non-Surgical Treatment: Grade III
______ & Frequent manual removal of feces via ______.
What is a disadvantage to the latter method?
Peritoneal lavage & Frequent manual removal of feces via Epidural catheter
Epidural = labor intensive
TRUE / FALSE
Grade III rectal tears must be treated surgically.
FALSE
Often respond to non surgical treatment, which is also
cheaper
What are the different methods of surgical repair of rectal tears?
- Direct suture repair
- Temporary indwelling rectal liner
- Loop colostomy
Describe rectal tear repair using direct suture repair.
- Fresh, clean lesion close to anus
- Epidural
- Stay sutures in anus (split anus dorsally if necessary)
- Prolapse tear: -Hold with multiple Allis tissue forceps, Staple with TA90 & Oversew with simple continuous suture
- Alternatively, suture blindly
- (Lesions usually not accessible via midline celiotomy)
- (Laparoscopic repair has been described)
________ repair of rectal tears protects tear and allows it to heal spontaneously. It may also be used with or without direct suture
Temporary, indwelling rectal liner
Describe the Temporary, indwelling rectal liner technique of rectal repairs.

- Make liner by gluing palpation sleeve or similar to rectal prolapse ring
- Ring is 5 cm diameter, 7.5 cm long
- Place dacron loops through holes
- Caudal midline celiotomy
- Secure liner oral (“upstream”) to the tear
Anesthetized horse, dorsal recumbency
- Assistant passes lubricated ring, guided by surgeon to cranial to tear
- Ring secured with tight circumferential suture
- Incorporate circumferential suture into individual sutures through all layers of colon and Dacron loops in ring
- Bury circumferential suture with Lembert pattern
- Cross tie: Prevent cranial movement of sleeve when horse lies down
- Circumferential suture cuts through colon and allows passage of ring and liner in 9 – 12 days
- By then apposed colon edges have healed

What approache is taken when repairing rectal tears via indwelling liners?
Ventral midline celiotomy
When repairing rectal tears with an indwelling liner, circumferential suture is buried with a ______ pattern.
Lembert
The indwelling liner of rectal tear repair should pass in ____ days.
9-12 days
What techniques of rectal repair are pictured?
Which is preferred?

Loop colostomy is preferred to end-colostomy because it is easier to perform, easier to reverse.

The following are indications to repair a rectal tear via _____.
- Grade IV; +/- Grade III
- Tear > 25 % of rectal diameter
- Tear > 50 cm from anus
Loop colostomy
What approach is used in a loop colostomy?
High left flank, low left flank, ventral midline

Describe post op care and complications of loop colostomies.
Post care: cradle (prevent self-mutiliation)
Complications
- Dehiscence
- Infection
While palpating a valuable broodmare for diagnosis of pregnancy you feel a slight “give” in the rectum above your hand. There is a small amount of blood on your hand. Careful digital exploration reveals a 2 cm dorsal partial thickness tear. You advise the owner to:
A. Destroy the mare immediately before she suffers.
B. Cross tie the mare; administer banamine and antibiotics; watch carefully.
C. Send the mare immediately for surgery at a referral clinic.
D. Turn mare out in a large pasture.
B. Cross tie the mare; administer banamine and antibiotics; watch carefully.
What are some sequelae to Grade III/IV rectal tears?
- Cellulitis
- abscess
- toxemia
- laminitis
- intestinal adhesions
- stricture
- diverticulum
- fistula
What is the prognosis / survival rate for rectal tears based on grade?
- Grade I - 93 %
- Grade II - 80 %
- Grade III - 70 %
- Grade IV- 6%
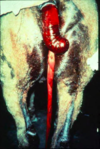
What is this?

Rectal Tear
TRUE/FALSE
Rectal prolapse may affect any breed, sex or age but more commonly affects older feedlot cattle.
FALSE
Affects younger feedlot cattle
Describe the pathogenesis of rectal prolapse.
- Abdominal/pelvic cavity vs. anus
- Decreased sphincter tone
- Constipation, diarrhea, colitis, cystitis, dystocia
- Excessively short tail cropping of sheep
- Altered pressure gradient
Classify the Rectal Prolapse!
Only mucosa projects through anus

TYPE 1
Classify the Rectal Prolapse!
Prolapse of all layers of rectum

Type II
Classify the Rectal Prolapse!
Small colon intussuscepts into rectum

Type III

Classify the Rectal Prolapse!
Rectum / colon intussusception through anus

Type IV

What are the most common types of rectal prolapse?
Types I & II
On palpation of rectal prolapse, ______ are continuous with anus.
_____ has palpable depression (“Trench”) inside rectum.
On palpation of rectal prolapse, Types I – III are continuous with anus
Type IV has palpable depression (“Trench”) inside rectum.
How can rectal prolapse be managed?
- Eliminate predisposing factors
- Eliminate straining
- Soothe mucosa
- Resolve prolapse
What are the benefits of a Caudal epidural anesthesia when managing rectal prolapse?
Caudal epidural anesthesia
- Resolves straining (temporarily)
- Allows evaluation
- May facilitate repositioning / replacement
- May allow surgery
What are teh treatment options for rectal prolapse?
- Replacement and purse string suture
- Perirectal injection of iodine?
- Submucosal resection
- Stair step amputation / Amputation after through- and-through sutures
Type ___ rectal prolapse must be treated with celiotomy, resection, anastamosis.
Type IV
Describe the treatment of rectal prolapse via replacement & puse string suture.
- Caudal epidural
- Clean prolapse: Hypertonic solution, Glycerol
- Lidocaine jelly
- Reduce prolapse
Purse string suture:
- Umbilical tape
- Tighten to allow 2-3 fingers
- Remove after 1 week
A rectal prolapse that is necrotic, ulcerated, traumatized mucosa, and healthy underlying tissue should be treated with ______.
Submucosal resection
Describe the surgical technique of submucosal resection treatment of rectal prolapse.
- Epidural and hypertonic solution
- Insert flexible tubing, fix with needles (cross-pin)
- Make two circumferential incisions, just through mucosa, at ends of tissue to be removed
- Connect with longitudinal incision to same depth
- Remove collar of damaged tissue by blunt dissection (ligate individual vessels)
- Anchor tissue with 4 simple interrupted sutures (monofilament, absorbable)
- Complete apposition with continuous suture for each quadrant

_____ correction of rectal prolapse causes reduced risk of stricture formation.
Stair step amputation
Describe the technique of stair step amputation surgical repair of rectal prolapse.
- Circumferential incision: Preserve inner mucosa and submucosa; Create plane toward caudal aspect of prolapse
- Make incision through inner layer of mucosa
- Flap inner mucosa over outer and suture as for submucosal resection

This is a type _____ rectal prolapse.
Type IV
TRUE / FALSET
Rectal prolapse in a sheep always requires amputation of at least some portion of rectum.
TRUE??
Prognosis of rectal prolapse:
- Types I & II
- Types III & IV
- I & II: Good
- III & IV: guarded (vascular damage to small colon)
What is an alternative to purse string suture repair of rectal prolapse?
Perirectal injection of iodine (causes scar tissue formation and permanent purse string)


