Radiography Flashcards
Describe the 3 radiation protection principles.
Justification- must do more good than harm.
Optimised- ALARP- As low as reasonably practiciple
Limitation- individual dose limits are used to ensure no one has an unacceptable exposure.
What is the inverse square law and why is it relevant to radiographs?
The X-ray follows this law.
That the further away from the source, the intensity of the x-ray reduces.
What is the pattern of attenuation?
This is how we produce a radiographic image using the pattern produced by the interaction of x-rays with matter.
Compare the ways that an x-ray can be absorbed?
Full absorption (e.g. amalagam showing up white on an x-ray)
Partial absorption and scatter- individual components of the beam change direction.
Name this type of radiograph

Bitewing
Name this type of radiograph
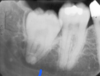
Periapical
Name this type of radiograph?

Occlusal. There are 2 types:
- True - cross sectional
- Oblique- image receptor is put in the occlusal plane.

Name this type of radiograph

Panoramic
Name this type of radiograph

Cephalometric
Name and describe the two legislations in the uk for radiation.
IRR17- for the general public and occupational exposure (those paid to be exposed to radiation)
- Employer must (register for x-rays, consult a radiation protection advsier and ensure radiation risk assessments are carried out)
- Controlled areas must be defined & local rules for that area.
IRMER- For Medical exposure of patients and those not paid for exposure (e.g. patient’s parents)
- Patient identifcation procedures
- Staff entitlement procedures
- procedures to provide information.
- 4 roles (referrer/ practioner/ operator/ employer.)
- Clinical evaluation.
How often and why do we test radiographic equipment?
To ensure It :
- is working correctly
- Is administering the expected dose level.
We test it:
- Every 3 months by a staff member
- Every 1-3 years by specialist staff.
What is the ideal projection geometry and why can we not achieve it?
These are the principles we want for achieving a good image:
- That the image receptor and object are in contact- cannot fully contact as the tooth is supported by bone.
- That the x-rays are a parallel beam- x-ray beam is divergent so cannot be parallel.
- That the image size is indentical to the object size- we can’t do this because the divergent beam causes mangification.
what is paralleling.
Where the image receptor and object are parallel but not touching.
The central ray is perpendicular to the long axis of the tooth.
Outer rays are at slight angles (the x-ray is divergent)

What is the FSD?
The focus to skin distance. This helps us line up the x-ray beam with the patient.
What FSD do we use for Radiography and why?
We use a long FSD to reduce magnification.
The longer FSD makes the x-ray beam near parallel compared to the diverging x-ray beam of a short FSD.
e.g. 20cm

What is rectangular collimation?
A device that reduces the dose of the x-ray and allows us to control the shape and size of the x-ray beam.
What is the blue film holder used for?
Anterior teeth.
What is the yellow film holder used for?
Posterior teeth
What is the red film holder used for?
Bitewings.
What are the 3 components of a film holder?
Bite block
Beam aiming device
Image receptor support

Compare the curve of Spee and the curve of Monsoon?
Curve of spee is the upward slope of the teeth as seen in a radiograph
Curve of monsoon is that the buccal cusps of molars are slightly higher than the palatal cusps.
What is the bisecting angle technique?
When the receptor and the object are touching but not parallel.
They are touching at the crown & far apart at the apex.
What are the soft tissue checkpoints for a maxillary occlusal radiograph?
Alatragus line should be paralell to the floor

What is the horizontal angle we want for radiographs?
90* to the line of the arch.


















