Quiz 7 Practice Problems Flashcards
(100 cards)
1
Q

A

2
Q

A

3
Q

A

4
Q

A

5
Q

A

6
Q

A

7
Q

A

8
Q

A

9
Q
what is an epidural hemorrhage
A

10
Q
what is a Subdural hemorrhage
A

11
Q
what is a subarachnoid hemorrhage
A

12
Q
what is a stroke? and what are the two types?
A

13
Q

A
E. Subdural hematoma due to a torn bridging vein coursing from the cerebrum to a dural sinus
14
Q

A
E. Middle meningeal artery hemorrhaging into the epidural space
15
Q

A

16
Q

A

17
Q

A
D. Midbrain
18
Q

A
B. 2
19
Q
The eye close

A

20
Q
The eye open

A

21
Q
the spinal chord section

A

22
Q
the flashlight in the eye

A

23
Q
movie theatre

A

24
Q

A

25

A. CN II and CN III
26


27


28


29


30


31
Anatomical and clinical movements of the eye and the nerves that innervate the muscles of the eye
Dilator pupillary muscle is sympathetics
Sphinter pupillary is CN III
Superior Tarsal is Sympathetics
Levator papebrae superioris is CNIII
Orbicularis Oculi is CN VII
ophthalmic nerve is CN V

32
Multiple sclerosis (MS) is an autoimmune disorder that causes the formation of plaques, inflammation and destruction of myelin sheaths, formed by oligodendrocytes. Identify the nerve most likely affected by a patient with MS.
A.Abducens nerve
B.Greater petrosal nerve
C.Ophthalmic nerve
D.Oculomotor nerve
E.Optic nerve
F.Trochlear nerve
A.Optic nerve (CN II)
33
A 64-year-old man suffers a lesion to his left CN VI. Identify symptom(s) this patient would most likely present with.
A.Anesthesia of forehead
B.Anhydrosis
C.Double vision when looking left
D.Double vision when looking right
E.Eye is positioned down and out
F.Miosis (pin point pupil)
G.Mydriasis (blown/large pupil)
H.Ptosis
I.Vision problems
A.Double vision when looking left
34
A 52-year-old woman suffers a lesion to her left oculomotor nerve. Identify symptom(s) this patient would most likely present with.
A.Anesthesia of forehead
B.Anesthesia of lower lip
C.Anesthesia of mandibular teeth
D.Anesthesia maxillary teeth
E.Anesthesia of upper lip
F.Anosmia
G.Double vision when looking left
H.Double vision when looking right
I.Eye is positioned down and out
J.Miosis (pin point pupil)
K.Mydriasis (blown/large pupil)
L.Ptosis
M.Vision problems
N.Weakness in clenching jaw
A.Eye is positioned down and out
A.Mydriasis (blown/large pupil)
A.Ptosis
35
A 45-year-old woman complains of double vision when looking to the right but not to the left.
Identify the side of the brainstem that is most likely injured.
A.Medulla – left side
B.Medulla – right side
C.Midbrain – left side
D.Midbrain – right side
E.Pons – left side
F.Pons – right side
Pons - right side
CN VI
36

CN III (right)
37
A patient presents with paralysis of the extraoccular eye
muscles. There is an abolition of the corneal reflex but there is
preservation of vision.
The most likely cause of this condition would be fracture of the:
A.foramen rotundum
B.petrous part of temporal bone (internal acoustic meatus)
C.superior orbital fissure (Rochon-Duvigneaud’s syndrome)
D.pterygopalatine fossa (Sluder’s syndrome)
E.maxillary sinus
C. superior orbital fissure (Rochon-Duvigneaud’s syndrome)
38
A patient presents with paralysis of the extraoccular eye
muscles. There is an abolition of the corneal reflex but there is
preservation of vision.
What other symptoms would this patient most likely present
with?
A.Anesthesia (loss of sensation) of the root of the nose, upper eyelid and forehead
B.Anesthesia (loss of sensation) of the upper lip and mouth
C.Anesthesia (loss of sensation) of the lower lip and mouth
D.Facial paralysis (Bell’s palsy)
E.Muscles of mastication paralysis
A.Anesthesia (loss of sensation) of the root of the nose, upper eyelid and forehead
39
1. Frontonasal dysplasia represents a spectrum of disorders characterized by widely spaced eyes, a midline facial cleft and absence of the tip of the nose (see photos). Recent work has implicated loss of function mutations in Alx3 homeobox transcription factors in this disorder. In mice, compound mutations in Alx3/Alx4 cause similar facial clefts. Based on this phenotype, discuss where you would anticipate Alx3 to be expressed in human development and what its normal function might be.
**Discussion****:** The tip of the nose is normally formed by fusion of the medial nasal prominences, with some contribution from the frontal prominence to the more cranial portions. Although in frontonasal dysplasia the face is abnormally wide and the eyes are far apart (suggesting excess production of tissue in the mid-face region), failure to form the _tip_ of the nose would argue that there has been a failure of normal medial nasal prominence fusion and/or a reduction in the amount of this tissue. Studies in mouse ([http://www.ncbi.nlm.nih.gov/pubmed/11641221](http://www.ncbi.nlm.nih.gov/pubmed/11641221)) indicate that both Alx3 and Alx4 are expressed in the medial nasal prominence. Loss of the Alx family of genes results in failure of neural crest migration into the facial prominences, resulting in these structures being both widely spaced and small. Consequently, the medial nasal prominences fail to fuse, resulting in a midline facial cleft.
40
. Although the palatine shelves fuse at the midline of the mouth, cleft lip and cleft palate are most frequently oblique, even in cases of bilateral clefts (see photo). Discuss why this is the case and what events are likely to have not occurred in formation of the face. In cases of bilateral cleft lip, would you anticipate cleft palate to be more or less likely than in the case of a unilateral cleft, and why?
The primary palate is a small wedge of tissue within the mouth that is formed from the medial nasal prominences—structures that also contribute to the philtrum. Failure of this region to fuse to the maxillary prominence is the most common cause of cleft lip. In severe cases, this cleft extends to the palate—but in all cases, it is a lateral cleft that does not extend into the tissue produced by the medial nasal prominence (i.e. it does not extend to the midline). In bilateral cleft lip, this failure has occurred on both sides, leaving tissue of the philtrum and primary palate suspended at the midline. In this case, it is highly likely that the cleft will extend to the primary palate within the mouth.
41
. Several craniofacial syndromes (Apert, Cruzon, Pfeiffer, Muenke) are due to stenosis, or premature fusion of the bones of the skull. Strikingly, all are caused by mutations in components of the Fgf signaling pathway, and are also associated with hand and foot defects—most commonly syndactyly (see image).
Interestingly (and perhaps incidentally), work in bat embryos has implicated sustained Fgf signaling in the development of bat wings compared to bat hind limbs or compared to mouse limbs (see image). In bat limb development, the forelimbs show elongation of the digits and retention of interdigit soft tissues. Based on this model, would you anticipate that the Fgf mutations seen in craniofacial syndromes reflect a gain of function or loss of function in the Fgf signaling pathway and why?
The connection between limb defects and craniofacial defects is not well understood. However, several studies suggest that the mutations seen in Apert syndrome as well as Pfeiffer and Muenke syndromes result in either enhanced affinity of the Fgf-receptor for its normal ligands or a loss of specificity (resulting in the receptor binding multiple ligands), both of which would enhance Fgf signaling. While cross-species comparisons are not always valid, these observations are consistent with the observed increased Fgf expression in the interdigit regions of bat forelimbs, which results in the retention of interdigit tissues and increased cell proliferation. How enhanced Fgf signaling results in stenosis is not clear, but increased proliferation and decreased cell death would be consistent with premature expansion/fusion of the bones of the skull.
42

Answer: D. At point A in this action potential, Vm has reached threshold potential and has triggered the opening of voltage-gated Na+ channels. The resulting Na+ influx is responsible for the rapid, self- perpetuating depolarization phase of the action potential.
43

Answer: C. The rapid depolarization phase is terminated at point B by the inactivation of the voltage-gated Na+ channels and the opening of the voltage-gated K+ channels. The latter results in the efflux of K+ from the cytosol into the extracellular fluid and repolarization of the cell membrane.
44
Which of the following electrical events is characteristic of inhibitory synaptic interactions?
A) A neurotransmitter agent that selectively opens ligand-gated chloride channels is the basis for
an inhibitory postsynaptic potential
B) Because the Nernst potential for chloride is about −70 mV, chloride ions tend to move out of
the cell along its electrochemical gradient
C) A neurotransmitter that selectively opens potassium channels will allow potassium to move into
the cell
D) An increase in the extracellular sodium concentration usually leads directly to an inhibitory
postsynaptic potential
Answer A. Opening of ligand-gated chloride channels and movement of chloride ions into the cell leads to hyperpolarization of the membrane. Neither increasing the extracellular sodium concentration nor the movement of potassium into the cell leads to hyperpolarization of the membrane.
45
3) Which of the following statements concerning the mechanoreceptive receptor potential is/are true?
A) Increase in stimulus energy results in an increase in receptor potential
B) When receptor potential rises above a certain threshold action potentials will appear in the
neuron attached the receptor
C) Number of action potentials generated in the neuron attached to the receptor is proportional to
receptor potential
D) All of the above are correct
Answer D. The receptor potential is defined as the membrane potential of the neuronal receptor. Once the threshold for activation is reached the number of action potentials generated will increase in proportion to the strength of the stimulus until a plateau is reached.
46
4) Transmission of the electrical signal from the dendrites to the soma of a neuron occurs by which of the following?
A) Calcium channels
B) An action potential propagation
C) Electrotonic conduction
D) Synaptic transmission
Answer C. Dendrites have few voltage-gated sodium channels. As such the capability of these structures in generating action potentials is extremely limited. Therefore, the transmission of the electrical signal in the dendrite is via a non action potential mechanism, electrotonic conduction.
47
When a muscle is suddenly stretched, a signal is transmitted over 1a sensory fibers from muscle spindles. Which of the following statements best describes the response elicited by these spindle afferent signals?
A) Contraction of the muscle in which the active spindles are located
B) Relaxation of the muscle in which the active spindles are located
C) Contraction of muscles antagonistic to those in which the active spindles are located
D) Relaxation of intrafusal fibers in the active spindles
Answer A : When a muscle is stretched, signals traveling over Ia sensory fibers will lead to contraction of the muscle in which the active spindles are located. At the same time, the antagonist muscles will be inactivated. The intrafusal fibers in the spindle do not go slack due to the tonic activation of gamma motor neurons by supraspinal systems.
48
Case 1 A 4-year old boy with cerebral palsy and epilepsy is receiving physical therapy in the clinic of Shriner’s Hospital. He develops a seizure that does not resolve and requires treatment for status epilepticus. Diazepam is an appropriate treatment. What patient and drug information would you like before selecting a dose and route of administration for diazepam?
Key Points ! Because intravenous administration of diazepam may be difficult in this patient, alternative administration routes should be considered. Oral administration is impractical in this patient who is seizing. !
The suitability of the rectal route for administration requires knowledge of both the degree of bioavailability (absorption, first-pass elimination) and the time-course of absorption.
Rectally administered diazepam is 90% bioavailable (e.g. well-absorbed, minimal first-pass elimination) and reaches therapeutic concentrations within 10 minutes. Especially if IV placement is challenging, the time to seizure cessation can be similar between intravenous and rectally administered diazepam. !
Intranasal midazalom has also been shown to be an effective means of halting seizures in pediatric patients.
49
A 27 year-old man with spina bifida develops an infection of his intraventricular-peritoneal shunt and requires antimicrobial therapy with vancomycin. He has impaired renal function due to prior vesicoureteral reflux. Vancomycin exhibits time-dependent bacteriocidal activity with persistant effects. It is eliminated primarily by glomerular filtration of unchanged drug and has a typical elimination half-life of 6 hours. Vancomycin is associated with nephrotoxicity. How would you adjust vancomycin dosing for this patient? How will you monitor therapy?
Renal impairment will decrease the clearance rate of renally eliminated drugs. Dosing interval and/or dose should be adjusted to decrease the rate of drug delivery while maintaining appropriate therapeutic concentration-time profiles of the drug. Referencing clinical guidelines and pharmacist consultation is appropriate.
In this case the purpose of drug monitoring is both to ensure adequate therapeutic levels as well as to prevent toxic effects. After dose adjustments, the new steady state drug concentration should be reached within four drug half-lives; trough levels should be drawn just prior to administration of the next dose.
50
A 39 year-old woman with mild hypothyroidism has been maintained on her current dose of levothyroxine for five years. Her most recent thyroid stimulating hormone (TSH) level is now somewhat elevated and suggests subtherapeutic levothyroxine levels. Further questioning reveals that the woman was concerned about potential bone mineral loss with aging, so she began taking an oral calcium supplement 5 months ago. A calcium associated DECREASE in which of the following is the most likely explanation for the change in this patient’s levothyroxine level?
A. Bioavailability
B. Clearance
C. Elimination rate
D. First-pass hepatic metabolism
E. Volume of distribution
A Bioavailability
Levothyroxine absorption from the gastrointestinal tract is sensitive to a number of dietary interactions. Recommendations are that it be taken on an empty stomach 30-60 minutes before breakfast to ensure consistent day-to-day absorption and bioavailability. • Remember that while absorption and bioavailability are not the same thing, absorption contributes to bioavailability. • If a change in elimination of levothyroxine were suspected as the cause for sub-therapeutic levothyroxine levels it would need to be because calcium caused an INCREASE in clearance and elimination rate. • Similarly, if first-pass hepatic metabolism of levothyroxine were suspected as the cause for sub-therapeutic levothyroxine levels it would need to be because calcium caused an INCREASE in in this process.
51
A morbidly obese 63 year-old man with congestive heart failure and atrial fibrillation will receive digoxin therapy. Digoxin has a narrow therapeutic window with the potential for dysrhythmias at elevated plasma levels. Despite its relatively large volume of distribution, digoxin is not concentrated in fat tissue. What would be the most likely anticipated plasma drug levels if digoxin dosing were based on this patient’s total body mass?
A. Sub-therapeutic drug levels
B. Supra-therapeutic drug levels
C. Therapeutic drug levels
B. Supra-therapeutic drug levels
• Since digoxin does not concentrate in fat tissues, adjusting the dose upward to account for this patients increased weight due to fat is likely to cause supra-therapeutic digoxin drug levels. It is therefore not recommended to adjust digoxin dosing based on weight.
52
A 46 year-old man with alcoholic cirrhosis and ascites is receiving diuretic therapy with furosemide. In healthy patients, furosemide has a volume of distribution of 7.7 liters and is 99% protein bound. Hypoproteinemia in this patient results in an increase in furosemide volume of distribution. Which of the following is the most likely affect that the increased volume of distribution will have on drug elimination?
A. Change from 1st-order to 0-order kinetics
B. Change from 0-order to 1st-order kinetics
C. Decreased clearance
D. Decreased half-life
E. Increased clearance
F. Increased half-life
F. Increased half-life
• While an increase in volume of distribution would decrease the elimination rate constant and thus increase the half-life of the drug, it would not be expected to have an effect on elimination kinetics.
A change in the volume of distribution would not be expected to change the clearance of furosemide. However, other organ system dysfunction caused by the liver (and probably kidney) disease could affect clearance.

53
Fancying herself an expert in pharmacokinetics, the 39 year-old woman with hypothyroidism looks up the Clinical Pharmacology of levothyroxine on rxlist.com and notices that the elimination half-life is approximately 7 days. She decides to experiment with once-weekly dosing of her medication. Which of the following best describes the necessary dose adjustment and effect on plasma drug concentration variability as a result of changing to onceweekly levothyroxine dosing?
A. 7 times the daily dose, increased plasma concentration variability
B. 1/7th daily dose, increased plasma concentration variability
C. 7 times the daily dose, decreased plasma concentration variability
D. 1/7th daily dose, decreased plasma concentration variability
E. no change, no change
A. 7 times the daily dose, increased plasma concentration variability
• To achieve the same steady state concentration of levothyroxine, the patient would need to maintain the same overall rate of drug administration by giving 7X the daily dose but only once per week.
The longer interval and larger dose will cause higher peak drug concentrations and lower trough concentrations
54


55


56
Facial Nerves V and VII explain the course and how they overlap!!!!

57


58


59


60


61


62


63


64
A patient suffers injury to the mandibular branch of the trigeminal nerve (CN V-3) during a dental procedure. Identify symptom(s) this patient would most likely present with.
A.Anesthesia of forehead
B.Anesthesia of lower lip
C.Anesthesia of mandibular teeth
D.Anesthesia maxillary teeth
E.Anesthesia of upper lip
F.Anosmia
G.Double vision when looking left
H.Double vision when looking right
I.Eye is positioned down and out
J.Miosis (pin point pupil)
K.Mydriasis (blown/large pupil)
L.Ptosis
M.Vision problems
N.Weakness in clenching jaw
A.Anesthesia of lower lip
B.Anesthesia of mandibular teeth
C.Weakness in clenching jaw
65
A patient suffers a lesion to the nerve within her right stylomastoid foramen inhibiting the function of this nerve.
A. What nerve is effected by this lesion?
B. Will this lesion effect general sensation of the head (if so which part) or
motor function to the head (if so which part)?
C. Will taste be effected by this lesion? Why or why not?
D. Will this patient have any trouble crying on the right side? Why or why not?
E. Will parotid gland function be effected by this lesion? Why or why not?
F. During the physical examination you conduct the pupillary reflex … what
do you expect to observe in your patient?
G. During the physical examination you conduct the corneal reflex … what do
you expect to observe in your patient?
A. What nerve is effected by this lesion? Facial nerve proper
B. Will this lesion effect general sensation of the head (if so which part) or
motor function to the head (if so which part)? BM mm facial exp
C. Will taste be effected by this lesion? Why or why not? No
D. Will this patient have any trouble crying on the right side? Why or why not? No
E. Will parotid gland function be effected by this lesion? Why or why not? No
F. During the physical examination you conduct the pupillary reflex … what
do you expect to observe in your patient? Normal reflex
G. During the physical examination you conduct the corneal reflex … what do
you expect to observe in your patient? No reflex
66
A summary of Cranial Nerves:

67
Table summary of CNs

68
A 55 year-old man takes a baby aspirin once daily for cardiovascular event prevention. In anticipation of surgery for wide local excision of a melanoma on his neck, his surgeon has asked him to discontinue his aspirin. Aspirin has a plasma half-life of approximately three hours; it impairs platelet aggregation by irreversibly acetylating a serine residue on cyclooxygenase and thus inhibiting thromboxane A2 synthesis in platelets. How far in advance of his surgery should the patient discontinue his aspirin in order to have return of platelet aggregation capacity?
This is an example of a drug that exerts its effect both allosterically and on an enzyme instead of a receptor.
The plasma elimination half-life and effect half-life of a drug are not necessarily the same. The duration of effect of a drug depends on both its pharmacokinetic and pharmacodynamic properties.
Because aspirin irreversibly inhibits cyclooxygenase, its effect half-life is much greater than its plasma half-life. The effect half-life of aspirin correlates more closely to platelet half-life.
Cessation of aspirin therapy 7-10 days should allow return of platelet function.
69
The personal physician to a 49 year-old musician with disordered sleep decides to administer intravenous boluses of lorazepam along with a continuous infusion of propofol to help his client sleep. Lorazepam and propofol are both allosteric modulators that enhance the function of GABAA receptors. The patient develops respiratory depression and dies. What pharmacodynamic and pharmacokinetic factors could have contributed to this patient’s death?
Administration of multiple drugs that affect the same receptor may have complex results depending on the strength of the bonds, the location of binding, and the intrinsic activity of the drugs.
Drugs with low therapeutic indices like propofol have a narrow range between the effective and toxic or lethal concentrations.
Concentration-time relationships for a single bolus dose of a drug may not always be useful for designing continuous infusion dosing regimens.
70
1. A physician is considering beta-blocker therapy for a 63 year-old man with coronary artery disease who also suffers from chronic obstructive lung disease. Beta-1 receptor blockade decreases heart rate and contractility. Beta-2 receptor stimulation causes bronchodilation. Which of the following might be the most appropriate therapy for this patient?
A. Administration of a non-selective beta blocker
B. Administration of a beta-1 selective beta blocker
C. Administration of a beta-2 selective beta blocker D. Avoidance of all beta blockers
B. Administration of a beta-1 selective beta blocker
## Footnote
Reducing heart rate and contractility and thus cardiac work are therapeutic goals in coronary artery disease management. This can be accomplished with beta-1 adrenergic receptor blockade.
This patient also suffers from chronic obstructive pulmonary disease likely from a long-standing smoking history. He may have a bronchospastic component to his disease, and may even use a bronchodilating agent that activates beta-2 receptors. Blocking beta-2 receptors with a non-specific beta blocking drug could worsen his pulmonary symptoms.
71
Consider the figure below. Which of the following best describes curve B?
## Footnote
A. A partial agonist compared to Drug A
B. Administration of Drug A in the presence of an irreversible antagonist
C. Administration of Drug A in the presence of an allosteric antagonist
D. Administration of Drug A in the presence of a non-competitive antagonist E. All of the above
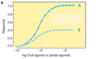
E. All of the above
Key Points
In this case curve B depicts a lower maximal response compared to curve A. The half-maximal response occurs at approximately the same concentration.
Administration of the same agonist in the presence of a non-competitive antagonist (irreversible or allosteric) could account for this concentration-effect relationship.
This shape of curve could also be seen if B were a partial agonist compared to A.
72
A 42 year-old woman develops a pulmonary embolus and begins therapy with warfarin. Through drug monitoring and dosage adjustment, the patient is determined to require approximately two-thirds the dose of the average patient to maintain therapeutic drug levels; after that point, her therapeutic course is uneventful. Which of the following terms best describes this patient’s drug response to warfarin?
A. Hyperreactive
B. Hyporeactive
C. Idiosyncratic D. Tachyphylactic E. Tolerant
A. Hyperreactive
## Footnote
Key Points
This case of a patient who is hyperreactive compared to normal populations is a pharmacogenetic example of genetic contribution to differences in drug responses within the population.
This patient likely carries one of the VKORC1 or CYP2C9 polymorphisms that result in increased sensitivity to the anticoagulant effects of warfarin.
73
A 25 year-old female presents to the clinic with maxillary tooth pain and tenderness to the skin of her upper lip. She also complains of purulent nasal discharge and congestion for the past 12 days. Identify the nerve most likely affected resulting in these symptoms.
CN V-1
CN V-2
CN V-3
CN VII

74
The Five Paranasal Sinuses

75
In addition to rhinorrhea and nasal congestion, the same patient also presents with watery eyes and anosmia. Identify the most likely reason the patient has “watery eyes” and “anosmia”.
Block the nasolacrimal duct and affect the CNI
76
A 4 year old female presents to the clinic with pain and swelling behind her left ear. What structure is inflamed? How could a sinus infection be associated with this finding?
The Mastoid antrium and mastoid air cells could be inflamed, and this could be from a sinus infection that has traveled into the nasal cavity and then up the opening of the pharyngotympanic tube!
77
Would these lesions affect taste, lingual sensation, or both:
- mandibular nerve
- chorda tympani nerve
- proximal lingual nerve
- distal lingual nerve
Mandibular nerve: Lingual sensation
Chroda tympani: Taste
Proximal lingual nerve: Lingual sensation
Distal lingual nerve: Both
78
A 45-year-old woman presents with paralysis of muscles of facial expression on her right side with ipsilateral loss of taste on the anterior surface of her tongue.
Where do you suspect the lesion to be occurring?
Right internal acoustiic meatus
79
The path of CN VII: Facial nerve proper

80
The path of CN VII: chorda Tympani nerve

81
The path of CN VII: Greater petrosal nerve

82
A 45-year-old woman presents with paralysis of muscles of facial expression on her right side with ipsilateral loss of taste on the anterior surface of her tongue.
What additional findings may you suspect?
Dryness of eyes
Dry mucous membranes in nasal cavity/palate
Dry mouth
Hyperacusis
83
45-year-old woman presents with paralysis of muscles of facial expression on her right side with ipsilateral loss of taste on the anterior surface of her tongue.
What additional findings would you suspect if a CN VII schwannoma in the internal
acoustic meatus is the cause of her
problems?
Hearing Loss
Vertigo (balance problems)
84
Imaging of a 56-year-old man shows a tumor compressing the nerves traversing the right hypoglossal canal. Identify the symptom(s) from the following list that the patient could be presenting with as a result of this condition. Explain why.
Difficulty saying “La, La, La, La, La”
Tongue deviates to side upon protrusion
85
A 44-year-old male presents with the following deviation of his tongue during a physical examination (see photo). Imaging reveals a tiny stroke in his brainstem.
Identify the most likely location for this lesion.
Right Side Medulla
86
A 60 year old man suffers a stroke. Using a tongue blade, the left side of the patient's palate is touched, which results in a gag reflex with the left side of the palate elevating more then the right, and the uvula deviates to the left.
What nerve is most likely affected by this stroke?
What muscle is most likely affected?
What level of the brainstem is most likely affected? L or R?
What nerve is most likely affected by this stroke? CN X (vagus n.)
What muscle is most likely affected? Levator veli palatini m.
What level of the brainstem is most likely affected? L or R? Right
general sensory innervation to palate:
CN V-2 (greater and lesser palatine nerves)
87


88
Damage of the lingual nerve before it is joined by the chorda tympani in the infratemporal fossa would most likely result in loss of:
a. general sensation to the anterior two thirds of the tongue
b. general sensation to the posterior one third of the tongue
c. secretion of the submandibular gland
d. taste sensation from the anterior two thirds of the tongue
e. taste sensation from the posterior one third of the tongue
A. general sensation to the anterior two thirds of the tongue
- Lingual nerve comes from CN V-3 and does general sensation for anterior 2/3 of tongue
- Chorda tympani (from CN VII) not affected since lesion is prior to joining, so taste and secretions from submandibular and sublingual glands are intact
- posterior 1/3 of tongue: taste and general sensation from CN IX
89
A 52-year-old man with ankylosing spondylitis underwent bilateral stapedectomy as a result of progressive hearing loss. The procedure resulted in a substantial improvement in the patient’s hearing. However, the right chorda tympani nerve was injured during the surgery. Identify symptoms from the following list that the patient present with as a result of this injury. Explain why.
Xerostomia (dry mouth)
Ageusia (ant 2/3 tounge)
90
The middle nasal concha is part of what bone?
a. Ethmoid bone
b. Maxilla
c. Palatine bone
d. Sphenoid bone
e. Vomer
Ethmoid bone
## Footnote
- superior and middle nasal conchae are part of ethmoid bone
- perpendicular plate also part of ethmoid bone and forms superior part of nasal septum
- vomer is its own bone and forms posteroinferior part of nasal septum
- inferior nasal concha is its own bone
- palatine bone is its own bone and forms the posterior part of hard palate
91
A 23-year-old man comes to you complaining that he can't stop crying, i.e. tears regularly run down the right side of his face. You suspect that one of the lacrimal ducts on the right side of the face is blocked. You look into an endoscope to see if the nasolacrimal duct is blocked. Into which part of the nasal cavity would you most likely look to see the opening of the duct?
a. Hiatus semilunaris
b. Inferior meatus
c. Middle meatus
d. Sphenoethmoidal recess
e. Superior meatus
Inferior Meatus
## Footnote
- nasolacrimal duct drains into inferior meatus
- hiatus semilunaris is in the middle meatus, where frontal sinus , anterior ethmoid air cells, and maxillary sinus drain
- superior meatus receives drainage from posterior ethmoid air cells
- sphenoethmoidal recess is superior to superior nasal concha and receives drainage from sphenoid sinuses
92
A 38-year-old patient complained of acute dental pain. The attending dentist found penetrating dental caries (dental decay) affecting one of the mandibular molar teeth. Which nerve would the dentist need to anesthetize to work on that tooth?
The inferior Alveolar
## Footnote
- inferior alveolar is branch of CN V-3, which does general sensation to mandibular teeth
- lingual nerve: branch of V-3. general sensation to tongue.
- buccal nerve: branch of V-3. general sensation from skin of cheek and cheek’s oral mucosa (vs. buccal nerve branch from VII—motor to buccinator and other muscles of facial expression)
- mental nerve: branch of V-3, from inferior alveolar nerve. general sensation to chin skin and lower lip.
- nerve to mylohyoid: branch of V-3. motor to mylohyoid and anterior belly of digastric.
93
The pharyngeal tonsils (aka adenoids) may become inflamed and in serious cases need to be removed. Where would the physician most likely look to find them during surgery?
Dorsal surface of the tongue
Pharyngeal recess
Piriform recess
Roof of the nasopharynx
Tonsillar fossa

94


95


96


97


98
Innervation of the Larynx

99


100




