Pathology of diabetes Flashcards
Describe the basic appearance of pancreatic tissue
Lobules of glandular tissue surrounded by fat

This is histology of a normal pancreas - where is the islet of Langerhans?


Identify the following features of the normal pancreas

Top 2 are B cells - that secrete insulin. about 2/3 of the islet is made of these
Bottom shows a capillary - where insulin, glucagon etc are drained away
Describe the aetiology and cause of type 1 diabetes
Aetiology isn’t really understood
Mutations in genes for Human leukocyte antigen - which is meant to help T cells recognise self/non-self
Mutation means autoimmune attack on pancreatic B cells - in which there is lymphocytic invasion of islets
What is insulitis?
Insulitis refers to the lymphocytic invasion of the islets of langerhans - which autoimmune attack in Diabetes type 1 causes
The effect of this is scarring of the islets - leading to shitey insulin production
What is shown here?
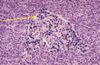
Lymphocytes in the islets (insulitis)
What are the potential aetiological triggers of diabetes type 1?
Environmental triggers?
Viral infection in which virus mimics B cell expression?
Chemicals?
Bacteria altered in gut in infancy?
All not well understood so we dont really know its basically just genes & environment
What is the effect of the destruction of B cells on the production of glucagon?
Destruction of B cells = < insulin & > glucagon
What causes diabtes type 2 to develop?
Aetiology not entirely known however it is caused through:
1) reduced tissue sensitivity to insulin (insulin resistance)
2) Inability to secrete very high levels of insulin
Basically - there is an inability for the B cells to meet an increased demand for insulin by the body
What is the main cause/risk factor for type 2 diabetes?
Being too thicc
Too much fat around the pancreas (pot belly) due to too much food intake and not enough exercise
Things like genes are relatively unimportant in causing it
Describe how obesity leads to type 2 diabetes?
- Obesity causes increased [fatty acid]blood due to leakage of overfull adipocytes
- Chronic high [fatty acids] means that insulin receptors lose their sensitivity to insulin - because it’s being released all the time
- Reduced sensitivity means more insulin is needed to elicit the same glucose uptake
- People with T2 diabetes develop this when their bodies can no longer cope with the increasing insulin demand
Why fatty acids actually cause this to happen isn’t really known either
What role does genetics play in determining whether or not someone with central adiposity (fat belly) will become diabetic?
There are many genes that control how much insulin is released, ie some cause lots of insulin release and some only cause some insulin release.
In people who become type 2 diabetic - the gene causing HIGH insulin release is variant, so only low amounts of insulin can be released
in summary - Implicated genes are for poor B cell ‘high end’ insulin secretion
Can only fat people can get type type II diabetes?
Nah fam
Slim person with tons of shitey genes can become type 2 diabetic even through modest raises in insulin
What role does genetics play in type 2 diabetes?
Multiple genes involved in causing inadequate ‘high level’ insulin secretion by B cells
However, these are not Human Leukocyte Antigen or adiposity genes
Overall, T2DM = multiple gene defects of pancreatic B cell insulin production which is unmasked by central adiposity
What is the most common cause of death for people with Diabetes?
Myocardial infarction
In patients with diabetes, what is the main reason why long term complications will arise?
Prolonged poor glycaemic control
What is the main long term complication in diabetes?
Damage to vessels - both large vessel disease and small vessel disease
In large vessels - DM accelerates the formation and growth of atherosclerosis
What is the effect of DM accelerating the growth of atherosclerotic plaques?
Manifests increased risk of:
- Coronary heart disease!
- Myocardial infarction
- Atherothrombotic stroke
There are many theories as to how Diabetes accelerates atherosclerosis
Explain how glucose molecules in the blood may account for this?
Basically - high [Glu] in DM means that some glucose molecules attach to Low density lipoproteins LDL
This prevents them from binding to their receptors in the liver = high [LDL] (hyperlipidaemia)
High [LDL] accelerates atheresclerosis
What effect can diabetes have on arterioles?
Can cause a net influx of molecules into the potential space between Endothelial cells and basal lamina of the arteriole
This means that molecules end up trapped in this space - leading to thickening of the arteriole
Arteriolar disease is also called hyaline change
The basal lamina can also become thickened

Arteriolar disease - associated with diabetes - causes ‘hyaline change’
What risks are associated with hyaline change?
Very damaging in kidney, peripheral tissues (foot), eyes and in arterioles supplying nerves
What main morbidities are people with diabetes at risk of developing in their life?
Amputation
End-stage renal disease
Blindness
What changes can occur in capillaries due to diabetes?
Increased connective tissue surrounding capillaries - eg in the glomerulus of the kidney
Formation of nodules of connective tissue (Kimmelstiel-Wilson lesion)
What mechanism causes the thickening of arterioles and small vessels caused by diabetes?
Trapping of albumin in the subendothelial space
Due to albumin binding to glycosylated collagen in basal lamina of capillaries. (only glycosylated collagen will bind to albumin)
This is reversible at first but if covalently bonded = irreversible.
If covalently bonded (irreversible) = Advanced Glycosylation End-products (AGEs)


