Long term complications of diabetes Flashcards
When can complications occur in diabetes type 1 and type 2?
Complications can be present at the time of diagnosis in type 2 diabetes
Complications can occur as early as 5 years after a diagnosis of type 1 diabetes.
What is the effect of worsening glycaemic state on the risk of complications?
Increase with worsening glycaemic state/control

What is the difference between microvascular complications and macrovascular complications?
Macrovascular means it involves large blood vessels meaning the sizeable arteries in the body
Microvascular refers to capillaries n shit
What are the different types of macrovascular complications?
Coronary vascular disease
Cerebrovascular disease
Peripheral arterial disease
What are the different types of microvascular complications?
Retinopathy
Nephropathy
Neuropathy
What is the effect of diabetes on the risk of developing CVS disease?
Increases relative risk of getting CVDs such as MI, heart failure, stroke
What specific pathology thing most commonly causes macrovascular complications in diabetes and why?
Atherosclerosis
Diabetes causes dyslipidaemia (which includes stuff like hypercholesterolaemia)
Go look at cardio notes for plaque formation n shit
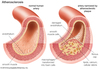
Identify the parts of this atherosclerotic plaque

Describe the features (specific levels of stuff) of dyslipidaemia seen in diabetes?
HDL cholesterol is lower
Triglycerides are higher
LDL cholesterol in form of small dense particles which are worse
Aside from dyslipidaemia - what other features in diabetes contribute to atherosclerosis
(think Virchow’s triad thing)
Endothelial dysfunction
Hypercoagulability of blood
What are the effects of atherosclerosis in diabetes?
Ischaemic cerebrovascular disease - strokes
Ischaemic heart disease - angina, MI
Heart Failure - related to coronary disease and abnormal cardiac myocyte glucose handling
Peripheral vascular disease (formation of ulcers etc)
How is macrovascular disease prevented?
Through good diabetes control
Blood pressure control
Lipid control
Smoking cessation, weight loss, exercise
(basically just avoiding risk factors)
Diabetic retinopathy is the most commonly diagnosed diabetes-related complication
Describe what happens to the eye as it develops
Initially in Non-proliferative stage:
- Retinal capillary dysfunction
- Platelet dysfunction
- Blood viscosity abnormality
Then moves to proliferative stage:
- Retinal ischaemia
- new blood vessel formation
- vitreous haemorrhage
- retinal tears/detachment
How is proliferative diabetic retinopathy treated?
laser photocoagulation
Describe the impact of diabetic retinopathy
20 years after diagnosis - 100% of people with Type 1 diabetes and 60% of those with Type 2 diabetes will have some form of retinopathy (mild-to-severe)
What other eye conditions does diabetes increase the risk of?
Cataracts
Glaucoma
What is nephropathy?
Deterioration of the proper functioning of the kidneys
Many causes - of which diabetes is a big boi
Describe how nephropathy in diabetes may develop
Diabetic patient develops Microalbuminuria - leak of protein (albumin) starts
This leads to:
- Glomerular basement membrane changes
- mesangial tissue proliferation
- “glomerular hypertension”
Progressive renal impairment - note kidneys do not shrink when the disease progresses
Describe the preventative measures for diabetic nephropathy
Urine albumin screening
Diabetes control
Renin-angiotensin system blockade - ACE inhibition, angiotensin receptor blockade, renin inhibition
Hypertension control
How would diabetic neuropathy present?
Diabetic patient with onset of Sensory/motor/autonomic symptoms and signs
Sensory neuropathy:
- Loss of sensation
- Paresthesia
- May lead to ulcers
Autonomic neuropathy:
- GI symptoms
- Cardio symptoms (blood pressure fluctuations in diabetic patient)
What is charcot foot?
condition causing weakening of the bones in the foot that can occur in people who have significant nerve damage (neuropathy)



