Myeloproliferative syndromes Flashcards
What are myeloproliferative disorders?
Myeloproliferative disorders most often represent a neoplastic proliferation of a marrow myeloid progenitor cell with differentiation to the mature form(s) (in contrast to the acute myeloid leukaemias, where maturation is very limited).
The normal control mechanisms governing the cell line(s) involved are no longer active, allowing accumulation of erythrocytes, platelets or leucocytes. Proliferation of mega- karyocytes produces growth factors causing a secondary overgrowth of fibroblasts (myelofibrosis).
Point mutations in which cell signalling gene have been implicated in myeloproliferative disorders?
JAK2 kinase
What are the main myeloproliferative disorders?
- Polycythaemia Rubra Vera
- Essential Thrombocythaemia
- Myelofibrosis
- CML
What is the main cell type proliferating in polycythaemia rubra vera?
RBCs
What is the main cell type that is proliferating in essential thrombocythaemia?
Platelets
What is the main cell type that is proliferating in myelofirbosis?
Fibroblasts
What is the main cell type with is proliferating in CML
White blood cells
What is polycythaemia rubra vera (PV)?
PV is a clonal stem cell disorder in which there is an alteration in the pluripotent progenitor cell leading to excessive proliferation of erythroid, myeloid and megakaryocytic progenitor cells. This usually corresponds with an increase in haemoglobin concentration and haematocrit.
What are secondary causes of polycythaemia?
- Hypoxia
- Increased EPO secretion
What are causes of hypoxia that cause secondary polycythaemia?
- High altitudes
- Chornic lung disease
- Cyanotic congenital heart disease
- Sleep apnoea
- Morbid obesity
- Heavy smoking

What are causes of increased EPO secretion that cause secondary polycythaemia?
- Renal cell carcinoma, Wilm’s tumour
- Hepatocellular carcinoma
- Adrenal tumours
- Cerebellar haemangioblastoma
- Massive uterine Leiomyoma
- Overadministration of EPO

What is relative polycythaemia?
Where the red cell volume is normal but there is a decrease in the plasma volume
What are causes of relative polycythaemia?
- Dehydration
- Burns
- Stress
- Spurious polycythaemia
What is the definition of polycythaemia?
Defined as an increase in haemoglobin, PCV and red cell count
What is the most accurate measure of polycythaemia?
Packed cell volume
What percentage of those with polycythaemia rubra vera have acquired mutations in JAK2 kinase gene?
95%
What is JAK2?
Cytoplasmic tyrosine kinase that transduces signals, especially those triggered by haematopoietic growth factors such as erythropoietin, in normal and neoplastic cells.

What symptoms might someone experience with polycythaemia rubra vera?
May be asymptomatic, or:
- Headaches
- Dizziness
- Tinnitus
- Visual disturbance
- Itch after hot bath
- Erythromelalgia
What are signs of polycythaemia rubra vera?
- Plethora
- Splenomegaly
- Gout
- Venous or Arterial Thrombotic signs - PE, Cardiac, DVT

Why do individuals with polycythaemia rubra vera get headaches?
Hyperviscosity
Why do individuals with polycythaemia rubra vera get plethora?
An excess of blood in a body part, usually used to describe a red, florid complexion
What are common causes of plethora?
- Chronic alcoholism
- Cushing’s disease
- Parenchymal lung disease
- Menopause
- Hyperthyroidism
- Mitral stenosis
- Polycythaemia
How would you investigate someone for potential polycythaemia rubra vera?
- Consider blood gas/SpO2?
- Bloods - FBC, U+E’s, PCV, urate, alk phosphatase, B12, EPO levels
- Bone marrow biopsy
- Cytogenetics
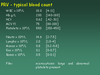
What might you find when investigating FBC in someone with Polycythaemia rubra vera?
- Increased RBC
- Increased Hb
- Increased Hct
- Possibly increased WCC and platelets