Mycobacteria Flashcards
(26 cards)
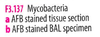
Direct examination of mycobacteria
Gram stain: typically invisible; gram+ rods ultrastructurally
Visible by acid-fast (Ziehl-Neelsen, Kinyoun) or by auramine rhodamine fluorochrome
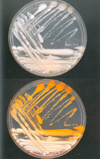
Mycobacteria culture
- Gold standard
- More sensitive than nucleic acid amplification tests
- Needed for susc testing
- Cultured on liquid broth and solid media
- Grows faster on broth (e.g., Middlebrook)
- In broth, organism can be assessed for cording, which is characteristic of M TB
- Solid medium egg based (e.g., Lowenstein-Jensen) or agar based Middlebrook needed for some orgs; helps detect mixed infection
Full identification of mycobacteria isolated in culture
- nucleic acid hybridization probes
- multiplex PCR
- growth characteristics and biochemistry:
- first classified as a rapid grower of slow grower
- further subclassified based on temperature preference and pigmentation (nonchromogen, scotochromogen, or photochromogen)
- finally classified according to series of biochemical tests that take days to weeks
Important Mycobacterial species in the lung
MAC, M TB, M kansasii, M xenopi, M abscessus
Important Mycobacterial species in the lymph node
MAC, M TB, M scrofulaceum, M haemophilum
Important Mycobacterial species in the skin and soft tissue
M fortuitum, M chelonae, M abscessus, M marinum, M ulcerans, M haemophilum
Important Mycobacterial species in GI tract
M TB, MAC
Mycobacterium tuberculosis
- key characteristics
- clinical features
- slow growth
- flat, dry, white, wrinkled colonies on solid media
- prefers 37 degrees
- cording in broth
- NAP sensitivity
- nonchromogenic
- Clinical features
- tuberculosis can be causes by
- M tuberculosis
- M microti
- M bovis
- M africanum
- M canetti
- Spread by respiratory droplets or aerosols
- primay infection = pulmonary and then may undergo
- spontaneous eradication
- undergo resolution (latency), forming tubercles (caseating granulomas) in upper lobes
- produce active disease
- reactivation presents as active disease
- may be pulmonary or extrapulmonary: kidneys, bone, GI, meninges
- tuberculosis can be causes by
Adjunctive diagnostic tests for M tuberculosis
-
Pleural effusion
- Smear
- culture
- NAAT
- Adenosine deaminase (ADA) test
- Gastric aspiration for those without adequate respiratory specimen
-
tuberculin skin test (TST/PPD): positive may signify
- active TB
- latent TB
- nontuberculous mycobacteria infection
- vaccination with BCG
- False negative 2/2 anergy can occur in HIV
- IFN-gamma release assays: T cells from person with TB release IFN-gamma when stimulated in vitro to ESAT-6 and CFP-10
- Arysulfatase separates fast growing mycobacteria (M fortuitum and chelonae are pathogenic and positive while M phlei and M smegmatis are not positive or pathogenic)
Nontuberculous mycobacteria
Isolation does not necessarily indicate infection
Mycobacterium avium complex
- M avium and M intracellulare
- infection in immunocompromised and immunocompetent
- Amongst immunocompetent, 3 forms of disease:
- heavy smokers with upper lobe cavitary disease, resembles classical Tb
- “Lady Windermere syndrome” seen in elderly women with weak cough; akin to colonization
- Hypersensitivty reaction to MAC after exposure to hot tub water contaminated with organisms
- MAC is most common cause of scrofula
- In culture, slow growing and may be pigmented or nonpigmented
M kansasii
- Infection resembles Tb in patients with immunosuppression or underlying pulmonary disease such as pneumoconiosis
- Slow growing photochromogen
M marinum
Associated with wound exposure to fresh water fish tanks or salt water, and causes localized cutaneous infection (fishtank granuloma)
M ulcerans
indolent, necrotizing, ulcerating cutaneous lesions (Buruli ulcer)
M leprae
- disease
- geographic distribution
- diagnosis
- stain
- Leprosy (Hansen disease)
- Hawaii, Texas, Louisiana (harbored by armadillos)
- cannot be cultured on artificial media
- best seen with Fite stain on tissue bx