Module 10: The Immune System Flashcards
Where does lymph return to the blood
via the left and right subclavian veins
Lymph Nodes: Definition and Function
- highly organized small organs less than 1inch in length
- optimize pathogen and lymphocyte interactions
- they are concentrated regions of B-cells and T-cells
- become swollen with infection when lymphocytes proliferate
- Function:
- filtration: macrophages to clean up debris
- i_mmune activation_: lymphocytes to search for pathogens and infection
Tonsils: Location and Function
- 5 total:
- pharyngeal tonsils: posterior wall of the nasopharynx
- palatine tonsils: boundary between soft palate and pharynx
- lingual tonsil: base of the tongue
- Function:
- contain lymphocytes that destroy and remove pathogens that enter through air and food
Appendix: Location and Function
- Location:
- at the beginning of the large intestine
- Function:
- contains high concentration of lymphoid follicles
- protect against harmful bacteria in intestines
- lymphocyte source for intestines
Spleen: Location and Function
- blood-rich, soft organ in the LUQ
- Function:
- contains lymphocytes that initiate immune responses to antigens in the blood (blood borne pathogens)
- removes debris and old blood cells and platelets from the blood
- stores RBC breakdown products
- stores platelets and WBCs
Thymus: Location and Function
- Location:
- bilobed developmentally regulated organ in the mediastinum
- Function:
- matureation of T-lymphocytes
- most active during childjood, it stops growing during adolescence and then gradually atrophies
Innate Immunity: Definition and the Natural Barriers
- Definition:
- composed of natural barriers to pathogen invasion and a general inflammatory response that prevents further infection and promotes healing
- Natural Barriers:
- physical
- epithelial cells of the skin and external surfaces
- frequent turnover to replace dead cells and remove bacteria
- epithelial cells of the skin and external surfaces
- biochemical
- secretions meant to trap or destroy microorganisms
- ex: mucus, perspiration, saliva, tears, earwax
- Antimicrobial molecules:
- small peptides secreted by epithelia cells and found in granules of leukocytes that disrupt cell membrane of bacteria
- ex. cathelicidins, defensins
- small peptides secreted by epithelia cells and found in granules of leukocytes that disrupt cell membrane of bacteria
- secretions meant to trap or destroy microorganisms
- microbiome
- good bacteria that compete with bad bacteria for nutrients and block pathogen adherence
- physical
Pathogen: Definition and Examples
- A pathogen is a disease producing micro-organism such as:
- bacteria: living, single-celled microorganism that can reproduce or grow on their own
- viruses: non-living DNA or RNA wrapped in protein that takes over host cells to reproduce
- fungi: living, single or multicellular organisms
- parasites: large group of the creppy crawlies!
- prions: proteins gone bad…
Antigen: Definition
- antigens are any molecule or partial molecule from a pathogen
- cell proteins, carbohydrates, lipids that are part of bacterial cell structure
- bacterial released toxins
- other large, complex “non-self” molecules
Immunogen: Definition
- an antigen that invokes an immune response
- ex. cell proteins and toxins = excellent immunogens
Inflammation Definition and Cardinal Signs
- inflammation is a cascade of events intitated when body tissues are damaged
-
Cardinal Signs
- Redness
- Heat
- Swelling
- Pain
- visible within seconds of injury
Vascular Changes with Inflammation
- vasodilation that causes increased permeability
- deliver leukocytes, plasma proteins, and biochemical mediators to site of injury
Migration to Tissue Injury Site in Inflammation
- migration: cells attracted to site of injury due to inflammatory mediators
- margination: cells move along the wall of the blood vessel
- diapedesis: cells pass through the blood vessel walls to injured tissue
- phagocytosis: cells engulf pathogens and debris at site of injury
Diapedesis
diapedesis: cells pass through the blood vessel walls to injured tissue
Tissue Response and Inflammation
- tissues responses to mediators and cellular changes:
-
to prevent infection:
- dilution of toxins
- activation of plasma protein systems
- phagocytosis of pathogens and debris
-
to prevent spread:
- clotting system activation
- activate adaptive immune reponse
-
begin the healing process
- removal of dead cells, products via lymph, etc.
-
to prevent infection:
Purulent Exudate
- exudate = “pus”
- fluid at site of injury with white blood cells, proteins, microbial debris, and cellular debris
- this is a sign of infection
Transudate
- clear fluid at site of injury which is mainly water filtrate from the blood
- less likely to be infected
3 Plasma Protein Systems in Inflammation
- Complement system
- classic pathway
- lectine pathway
- alternative pathway
- Clotting System
- Kinin System
Plasma Protein Systems: The Complement System
- Activated by 3 general mechanisms:
- Classic Pathway
- Lectin Pathway
- Alternative Pathway
- it is a cascade of molecules released that have many functions in the immune system
- 30 plasma proteins (C1-C9…), made by hepatocytes in the liver, and immune cells
- “complement” or enhances phagocytic and antibody responses
- Attracts Phagocytes: through production of opsonins and chemotaxins
-
Increases Inflammation:
- some of the C proteins are anaphylatoxins
- they cause Mast Cells and Basophils to degranulate→release of histamines → INFLAMMATION
- increased vascular permability
- smooth muscle contraction
- bronchoconstriction
- they cause Mast Cells and Basophils to degranulate→release of histamines → INFLAMMATION
- some of the C proteins are anaphylatoxins
- Forms the Membrane Attack Complex: destroys pathogen directly by putting a large channel in the membrane of the pathogen that disrupts osmotic balance and causes the cell to swell and burst

Membrane Attack Complex
- formed in the complement system of plasma protein system
- Membrane Attack Complex: destroys pathogen directly by putting a large channel in the membrane of the pathogen that disrupts osmotic balance and causes the cell to swell and burst
- pathogen lysis
Complement System Activation
- Classic Pathway: activated by antigen-antibody complex
- Lectin Pathway: activated by lectins binding to specific sugars (mannose) on the surface of the beacterium
- Alternative Pathway: activated by bacterial surface polysaccharides, etc.

Plasma Protein Systems: The Clotting System
- aka Coagulation
- proteins that form a fibrin meshwork at injury site
- stops bleeding
- prevents spread of infection
- traps microorganisms for removal
- framework for repair and healing

Plasma Protein Systems: the Kinin System
- group of proteins, including bradykinin
- activated by factor XIIa from the clotting cascade
- cause:
- dilation of blood vessels
- stimulate nerve endings (pain)
- smooth muscle contraction
- increased permeability and leukocytosis
- limited by kininases that degrade these proteins very rapidly

Interferons
- anti-viral proteins that help cells non-specifically target and prevent viral replication
- released in response to detection of viral nucleic acids
- reeleased from any body cell infected by a virus
- triggers virus-blocking enzyme release in body cells that breakdown viral mRNA
- this inhibits viral protein synthesis
- activate the immune system
- slow cell division and tumor growth in body cells
Functions of Inflammatory Cells (examples)
- recognize a limited range of pathogens or pathogen related molecules
- secrete inflammatory mediators
- cytokines:
- interleukins
- interferon
- tumor necrosis factor -alpha
- chemockins
- cytokines:
- kill pathogens and remove debris
Circulating Inflammatory Cells
- neutrophils
- monocytes
- eosinophils
- lymphocytes
- basophils
- platelets
Connective Tissue Inflammatory Cells
- mast cells
- fibroblasts
- macrophages
- lymphocytes
Neutrophil
- white blood cell
- short lived: 6-12 hours
- pus
- phagocytosis
- lobed nucleus

Eosinophil
- white blood cell
- parasite response
- regulate inflammatory mediators by degrading vasoactive molecules
- degrade histamine

Basophils
- white blood cell
- allergies
- asthma
- similar to mast cells
- basophilic granules

Monocytes
- white blood cell
- immature phagocytes
- become phagocytes through maturation
Mast Cell
- type of connective tissue inflammatory cell
- NOT basophils but look similar, have a different precursor origin
- Function:
- found in vascularized connective tissues, near epithelium (dermis, GI tract, respiratory tract)
- **INFLAMMATION**
- increased permeability of blood vessels
- smooth muscle contraction
- regulation of other cells during inflammation and healing by release and synthesis of inflammatory mediators
- histamine
- tryptase
- cytokines, prostaglandins, lekotrienes, growth factors
Mast Cells are activated by:
- physical injury: heat, trauma, UV light, radiation
- chemical agents: toxins, venom, proteolytic enzyme, antimicrobial peptides
- immunologic activation: anaphylatoxins, IgE, bacteria, viruses
Mast Cell Degranulation
- release of contents within granules
- chemotactic factors: attract leukocytes, espc. neutrophils
- MOSTLY RELEASE HISTAMINES
- proinflammatory (H1) receptors
- smooth muscle of bronchi causes bronchoconstriction
- anti-inflammatory (H2) receptors)
- secretion of gastric acid from parietal cells
- proinflammatory (H1) receptors
Injury to endothelium and subendothelial connective tissue triggers:
- endothelial cells
- adherence of leukocytes
- migration of leukocytes to tissue
- prothrombotic events: platelet activation, clot formation
- Platelets:
- hemostasis, coagulation cascade
- release granules: inflammatory mediatorys, coagulation, growth factors, adhesion molecules, protease inhibitors, Calcium, magnesium
- serotonin–vascular effects similar to histamine
Phagocytes
- Neutrophils and monocytes/macrophages are primary phagocytes for destruction of bacteria
- neutrophils = first response
- macrophages and others come later
- Phagocytosis:
- recognition and adhesion of bacteria
- they have antigens that are recognized
- engulf: forms phagosome
- lysosome fuses with the phagosome and forms phagolysosome
- destruction and digestion
- recognition and adhesion of bacteria
Natural Killer Cells
- CD16 and CD25
- specialized to nonspecifically detect and destroy virus infected cells and tumor cells
- detect “non-self” by looking for cells low in MHC “self” markers
- release cells called perforins that lyse the cell membranes of targets
- activated by cytokines
- important alternative to B and Tcell mediated immunity
- **these responses are conserved across species**
Regeneration
- a process where damaged tissue is replaced with healthy tissue of the original type
Repair
- replacement of destroyed tissue with scar tissue
- not as good as regeneration
Scar Tissue
- composed primarily of collagen, a substance which fills in the lesion and restores tissue integrity and strength, but cannot carry out the physiological functions of of the tissue it has replaced
- **Results in a loss of function**
Primary Intention
- wounds that have minimal tissue loss, such as papercuts or surgical incisions
- require very little sealing (epithelialization) and shrinkage (contraction)
- faster process than secondary intention
- heals primarily through the process of collagen synthesis

Secondary Intention
- much slower than primary intention
- requires a lot of tissue replacement
- this causes epithelialization, scar formation, and contraction to take longer

Phases of Wound Healing
- Phase 1: hemostasis
- takes seconds to hours
- vasoconstriction
- platelet aggregation
- leucocyte migration
- takes seconds to hours
- Phase 2: Inflammatory Phase
- takes hours to days (1-3 days)
- early–neutrophils
- chemoattractant release
- late macrophages
- phagocytosis and removal of foreign body/bacteria
- takes hours to days (1-3 days)
- Phase 3: Proliferative Phase
- takes days to weeks (3 days to 1 month)
- fibroblast proliferation
- collagen synthesis
- ECM (extracellular matrix) reorganization
- angiogenisis
- epithelialization
- takes days to weeks (3 days to 1 month)
- Phase 4: Remodeling
- takes weeks to months
- remodeling
- epithelialization
- ECM remodeling
- increase in tensile strength of wound
- takes weeks to months
Causes of Dysfunctional Wound Healing
- ischemia
- excessive bleeding
- excessive fibrin deposition
- predisposing disorder i.e. diabetes mellitus
- obesity
- wound infection
- inadequate nutrition
- use of certain drugs
- **tobacoo smoking**
Examples of Dysfunctional Wound Healing
- chronic wounds: last a long time
- wound disruption: wound continually sloughs off
- dehiscence: sutured wound pulls apart
- contracture: excessive wound contraction may result in deformity
B-Cells
B-Lymphocytes
- born AND mature in the bone marrow
- activated by CD4-T-Cells
- housed in lymphoid tissues
- recognize free pathogens (bacteria, toxins, viruses)
- involved in antibody-mediated immunity (aka Humoral Immunity)
- have specific antigen receptors: B-Cell Receptors (BCRs)
T-Cells
T-Lymphocytes
- born in bone marrow, mature in Thymus
- housed in lymphoid tissues
- recognize infected or cancerous body cells
- involved in cell-mediated immunity
- involved in activating total, combined immune responses
- have specific antigen receptors:
- T-cell Receptors (TCRs)
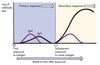
The adaptive immune system is:
Humoral (antibody mediated) Immunity and Cellular (Cell-Mediated) Immunity
- antigen-specific: requires the production of specific lymphocytes and antibodies against a specific antigen
- systemic: not restricted to the initial infection site
- has memory: second encounter causes a more rapid and vigorous response
Antibody
- aka immunoglobin
- Y -shaped protein made by plasma cells in response to a SPECIFIC antigen
- each antibody can only bind to **one specific antigen**
- the purpose of this binding is to help destroy the antigen
- an antibody is a type of immunoglobulin
Immunocompetent Cells
B cells or T Cells
- cells display a unique type of receptor that responds to a distinct antigen
- become immuncompetent before they encounter antigens they may later attack
- are exported to secondary lymphoid tissue where encounters with antigens occur
- mature into fully functional antigen-activated cells upon binding with their recognized antigen
Lymphocyte Development
- origin: bone marrow, hematopoietic stem cells
- maturation: bone marrow (B cells) or thymus (T cells)
- immunocompetence: able to recognize one specific antigen, displays unique antigen receptor
-
**Self-Tolerance**: able to recognize “self” cells and be unresponsive to self-antigens
- positive selection: maintain only cells that recognize “self” proteins -MHC
- negative selection: remove cells that are reactive to “self”- self-antigen

Lymphocyte Activation
- activation: happens when they actually encounter their specific antigen in the body
- proliferation and differentiation: once activated they will increase in number and make other immune cells
B-Cell Activation
Humoral (antigen-mediated) Immunity
- Pathogen invades the body
- B-cells with BCRs (B-Cell Receptors) are waiting to find their specific antigen
- Specific B-Cells with BCR recognizes specific pathogen and makes
-
plasma cells: produce specific antibodies for that pathogen
- 2000 antibodies per second
- lifespan of 5-7days
- memory cells: store memory of antigens to produce antibodies upon later infection, lay dormant until 2nd infection by same organism
-
plasma cells: produce specific antibodies for that pathogen
IgG
- MOST COMMON
- secreted to respond to most antigens
- highest after second exposure
- memory
- crosses placenta
- small monomer

IgM
- primary reaction
- stays on B-cell to act as B-cell receptor for antigen
- pentamer with 10 antigen binding sites
IgA
- secreted mostly in:
- mucus membranes
- tears
- saliva
- nasal
- respiratory
- gastrointestinal
- breast milk
- dimer with 4 binding sites
IgE
- secreted to respond to parasitic worms, allergic responses
- larger monomer
IgD
- binds to basophils and mast cells during hypersensitivity reactions
- small monomer
Anatomy of a an Antibody

Antibody-Mediated Responses
- Neutralize: combine with molecules, viruses to physically prevent them from interacting with cells
- agglutination: clump molecules, bacterial cells together, render non-functional
- Precipitation: separate them from solution like a chemical precipitate
-
Tagging for Destruction: mark free pathogens, attract other cells to destroy them
- complement system
- phagocytes
- natural killer cells
Active Immunity vs. Passive Immunity
-
Active Immunity: occurs when antibodies are made actively by memory cells
- present as long as memory cells are intact
- natural: due to infection with pathogen
- artificial: vaccines with attenuated pathogens
- present as long as memory cells are intact
-
Passive Immunity: occurs when antibodies are put into the body without memory cells, gone when supply is gone
- natural: breastmilk, IgA
- artificial: serum injection
Self Cells vs Infected Cells
- “self” is signified by MHC proteins on cell surface
- antigen presenting cells will display antigens from phagocytized pathogens
3 Types of T-Cells
- cytotoxic T-Cells (CD8)
- helper T-Cells (CD4)
- Regulatory T-Cells (CD4-25)
Class I MHC - SELF
- “MHC-self” signals that it is a self cell
- present on every body cell like a biochemical fingerprint, varies across individuals
- can display antigens “MHC I-antigen” signals that it is a body cell that has been infected
Class II MHC- APC
- present only on antigen presenting cells
- “MHCII-antigen” complex signals that an invading pathogen has been found by an APC
Cytotoxic T-Cell Function
- aka CD8 cells
- recognize body cells infected by pathogens by binding to MHC 1-self-antigen complexes
- CD8 cells then destroy infected body cells by lysis or granzymes/perforin released from its granules that induce apoptosis
- can be:
- virus infected
- mutated cancer cells
- transplanted donor cells
- can be:

Helper T-Cells
- aka CD4 cells
- recognize APC MHC II-antigen presenting cells
- release cytokines, chemicals that are necessary to activate other immune cells
- activate B-cells
- activate cytotoxic T-cells
- attract neutrophils and macrophages
Regulatory T-Cells
- aka CD4-25
- inhibit innate and adaptive immune responses to keep the system in check
- under research for autoimmune disease control
Helper T-Cells (CD4) activate B Cells
- helper T-Cells (CD4) stimulate and activate B-Cells
- Helper T-Cells can also recognize APC MHC II- antigen on B-cells
- release immune stimulating molecules to activate B-cells
- required for complete B-cell response
- **HIV virus attacks Helper T-cells**
opsonin
released by the complement system
attracts phagocytes and helps them to phagocytize pathogens
defensins
small peptides secreted by eptihelia cells and found in granules of leukocytes (neutrophils) that distrupt cell membrane of bacteria
DAMPs and PAMPs
- Damage associated Molecule Patterns:
- released when membranes are damaged or cells die
- Pathogen Associated Molecule Patterns:
- conserved patterns across pathogens
- peptidoglycans
- lipopolysaccharides
- viral RNA/DNA
- conserved patterns across pathogens
- detected by PRRs
- pattern recognition receptors
- located on leukocytes
- natural killer cells
- mast cells


