Mod XI: ANESTHETIC MANAGEMENT DURING THORACIC SURGERY Flashcards
ANESTHETIC MANAGEMENT DURING THORACIC SURGERY
General anesthesia
Standard induction expected for most thoracic procedures
Any deviation to be discussed with each procedure
Adequate preoxygenation is key!
Standard intravenous induction
Surgeon may want to perform a diagnostic bronchoscopy
If this is the case, place size 8-9 ETT or LMA if flexible bronchoscopy is planned prior to surgery
Traded for DLT at the conclusion of diagnostic bronchoscopy
A bronchoscopy can also be performed at the end of the case
Is the is the plan, the DLT will be replaced with either and ET tube or an LMA
After that, if there is no indication for prolonged ventilatory support, the pt can be extubated
This is why it’s important to communicate with the surgical team prior to starting the procedure, so that if a bronchoscopy is to be performed, adequate preparation can occur
Inhalation anesthetic are typically used for these cases
TIVA can also be used
There are some benefits of using Inhalation anesthetic over TIVA
inhalation agent have a brondilatory function, and they can be rapidly removed at the end of the case
Remember, clinical doses of inhalation agents do not significantly alter HPV
No N2O!
ANESTHETIC MANAGEMENT DURING THORACIC SURGERY
Total Intravenous Anesthesia
TIVA can be used effectively as a technique that does not inhibit HPV
IV anesthetics do not inhibit HPV
No benefit over 1 MAC of volatile agent and no difference in M&M between two choices
ANESTHETIC MANAGEMENT DURING THORACIC SURGERY
Maintenance
Adequate analgesia is imperative
Monitor fluid administration b/c excessive fluid administration has been a/w acute lung injury in the post op period
Can also cause a gravity dependent accumulation of fluid in the dependent lung, which can exacerbate shunting and hypoxemia during OLV
Muscle relaxant facilitates rib spreading
Risk of postoperative residual neuromuscular blockade
ANALGESIA FOR THORACIC SURGERY
Thoracotomy one of the most painful surgeries - Pain primarily caused by
Resection of thoracic tissue and
Bone for surgical exposure
Places pts at High risk for atelectasis and pneumonia d/t shallow breathing
Goal = balance between comfort and respiratory depression

ANALGESIA FOR THORACIC SURGERY
Pain after thoracic surgery leads to:
Splinting
Decreased resp effort
Hypoxemia
Respiratory acidosis
ANALGESIA FOR THORACIC SURGERY
Hollistic multimodal approach should be used to reduce post op pain - This can be done by
IV patient-controlled analgesia (PCA), coupled with
Thoracic epidural, or
Paravertebral block
ANALGESIA FOR THORACIC SURGERY
Thoracic epidural
Placed prior to induction
Catheter placed at T6-T8
Cautious use of IV narcotics if narcotics placed in epidural
ANALGESIA FOR THORACIC SURGERY
Paravertebral block
Placed at level of incision, plus 1-2 intercostal interspaces above and below
Provides good short-term pain relief
POSITIONING FOR THORACIC SURGERY
After induction of anesthesia and confirmation of correct tube placement, the pt is placed in which position?
Lateral Decubitus position with the surgical side up
POSITIONING FOR THORACIC SURGERY
After the Lateral Decubitus position is assumed a roll is placed caudal to axilla - What is it called? what’s its purpose?
Axillary roll placed caudal to axilla
Purpose it to keep the pt weight off the brachial plexus and the axillary fascia
Eventhough this roll is called the Axillary roll, it should never be positioned into the axilla b/c doing so may cause neurovascular compression

POSITIONING FOR THORACIC SURGERY
Positioning the Arms:
Arms padded and extended forward on arm boards
Support nondependent arm with pillows, Mayo stand or double arm boards
Be careful not to abduct the shoulder more than 90 degrees, or flex or extend pass the neutral point

POSITIONING FOR THORACIC SURGERY
Head support:
Head support on pillows to maintain head and neck alignment with spine
Lateral flexion can cause compression of neck vessels compromising cerebral perfusion
Careful not to compress dependent ear, pad with foam doughnut pillow to prevent pressure from the head
Careful not to place pressure on dependent eye to prevent corneal abarasion and retinal ischemia

POSITIONING FOR THORACIC SURGERY
Potential nerve injuries:
Brachial plexus most common!!! b/c it has two points of potential compression or stretch
Common peroneal nerve & Suprascapular nerve also have the potential for injury
ANESTHETIC MANAGEMENT DURING THORACIC SURGERY
Emergence
OLV or bronchial blocker will be discontinued
Remember to deflate bronchial cuff to reduce pressure on the bronchial mucosa, and to help prevent injury when removing the DLT
ANESTHETIC MANAGEMENT DURING THORACIC SURGERY
Re-expansion of the operative lung
The operative will then be re-expanded under direct visualization, so that the surgeon can look atelectatic areas, and for air leaks
Lungs inflated 20-30 cmH2O to reinflate atelectatic areas and to check for air leaks
ANESTHETIC MANAGEMENT DURING THORACIC SURGERY
Placement of chest tube:
Chest tube placed to facilitate removal of fluid in the pleura cavity, and to aid in lung re-expansion
ANESTHETIC MANAGEMENT DURING THORACIC SURGERY
Extubation:
Patients typically extubated in OR unless contraindicated
ANESTHETIC MANAGEMENT DURING THORACIC SURGERY
Post op ventilatory support:
If postoperative ventilatory support needed, DLT swapped for single lumen ETT
Done under direct vizualisation with a laryngoscope blade or
Glidescope (great idea)
ANESTHETIC MANAGEMENT FOR BRONCHOSCOPY (FLEXIBLE & RIGID)
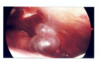
Purpose of Bronchoscopy (Flexible & Rigid):
To vizualise the upper airway as well as distal anatomies in the trachea and bronchi
Flexible => flexible scope
Rigid => Stiff scope like

ANESTHETIC MANAGEMENT FOR BRONCHOSCOPY
Flexible BRONCHOSCOPY:
Diagnostic procedure
Commonly performed prior to lung resection to reconfirm diagnosis, or to determine the invasion or obstruction of the distal airway
Allows for distal airway examination
Awake versus General
General with ETT or LMA
Oral versus nasal
ANESTHETIC MANAGEMENT FOR BRONCHOSCOPY
Rigid BRONCHOSCOPY
Diagnostic procedure
Procedure of choice for tracheal stenosis (tracheal dilation), airway obstruction, foreign body removal, and massive hemoptysis
General anesthesia
ANESTHETIC CONSIDERAATIONS FOR BRONCHOSCOPY: FLEXIBLE
Routes:
Oral or nasal approach

ANESTHETIC CONSIDERAATIONS FOR BRONCHOSCOPY: FLEXIBLE
Anesthetic technique:
Awake bronchoscopy
With or without sedation
Topical anesthesia via nebulizer, aerosol, or soaked pledgets
Laryngeal or glossopharyngeal nerve block
“Spray as you go” technique
General
LMA or ETT
Spontaneous vs. positive pressure ventilation

ANESTHETIC CONSIDERAATIONS FOR BRONCHOSCOPY: FLEXIBLE
Potential complications:
Dental/tissue damage
Airway rupture
Pneumothorax
Airway bleeding
Airway edema