Mod IX: Anesthesia for Intracranial Procedures Flashcards
(34 cards)
Anesthesia for Craniotomies
•Premedication
- Versed 1-2mg
- Fentanyl 50-100 mcg
Anesthesia for Craniotomies - Premedication
•Versed 1-2mg - •Avoid in
sedate patients or
patients who may become hypercarbic
(the increased CO2 will increase pressures in the brain)
Anesthesia for Craniotomies - Premedication
•Fentanyl 50-100 mcg - Again, with caution because
you don’t want the patient to hypoventilate
Anesthesia for Craniotomies - Premedication
What is already on anticonvulsant and BP medications?
Continue all anticonvulsant and BP medications
Anesthesia for Craniotomies - Premedication
Why would many of the patients be on H2-blockers?
to combat the gastric side effects of steroid therapy
Anesthesia for Craniotomies
Monitoring and Vascular Access
2 large bore PIVs
Aline
CVP – based on risk assessment of acquiring a VAE
Anesthesia for Craniotomies
Conditions associated with LOW RISK of VAE
Supine, prone, or lateral with minimal head elevation (<15 degrees)
Operation not near major venous sinus
Anesthesia for Craniotomies
Conditions associated with INTERMEDIATE RISK of VAE
Moderate head elevation (15-30 degrees)
Mild head elevation, but operating near major venous sinus
Anesthesia for Craniotomies
Conditions associated with HIGH RISK of VAE
True sitting position (>45 degrees)
Moderate head elevation and
Tumor invading bone or near a major vessel
Anesthesia for Craniotomies
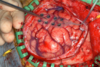
Graphical representation of Supratentorial vs. Infratentorial Tumors
Graphical representation of Supratentorial vs. Infratentorial Tumors
Major Supratentorial brain structure = Cerebrum
Major Infratentorial brain structures = Cerebellum & Brainstem

Anesthesia for Craniotomies
What’s the GOAL of induction? How is it acheived?
Keep the patient normotensive
Avoid up swings and dips in the pressure as a result of your intubation
Anesthesia for Craniotomies - Induction
Agents:
Propofol 1-2 mg/kg
Fentanyl up to 15 mcg/kg
NDMR
Choose volatile agent
Anesthesia for Craniotomies - Induction
Ensure that the DL and intubation is smooth. Prior to DL how should the pt be?
Well anesthetized and paralyzed
Anesthesia for Craniotomies - Maintenance
assist with brain relaxation
Infusions
Anesthesia for Craniotomies - Maintenance
Common infusions
Methohexital (Brevital) 30-50 mcg/kg/hr ~versus~
Propofol (diprivan) 3-6 mcg/kg/hr
Remifentanyl 0.08 – 2 mcg/kg/min
[<strong>Remifentanyl </strong>keeps the pt still and prevent the use of a NDMB especially if neuro monitoring required]
Anesthesia for Craniotomies - Maintenance
Volatile Agent – have to take what into consideration?
Neuromonitoring
Anesthesia for Craniotomies - Maintenance
Goal of Fluids management
Keep patient normovolemic
Anesthesia for Craniotomies
•Mayfield Head frame Placement effect on BP
Can cause a 20% increase in BP
Anesthesia for Craniotomies
•Mayfield Head frame Placement Can cause a 20% increase in BP. How do you prepare for this?
Have a bolus of propofol and/or fentanyl ready to administer prior to placement
Be aware of the onset time of the drug you are administering so that the effect occurs at the appropriate time
Anesthesia for Craniotomies
Once the surgeon places the head frame; who is responsible for moving the head while positioning the patient?
The Surgeon
Once the surgeon places the head frame; THEY are responsible for moving the head while positioning the patient
Anesthesia for Craniotomies
***If you have a patient in the Mayfield, it is critical that the patient does NOT move while in pins. Why?
A simple cough or buck can cause them to break their neck and cause paralysis.
Anesthesia for Craniotomies
When should patient with Mayfield head frame be reversed?
Don’t reverse these patients until head frame removed.
Anesthesia for Craniotomies
Some pictures of the Mayfield head frame
Some pictures of the Mayfield head frame
<em>https://www.youtube.com/watch?v=pgDSbA107Ow</em>

Anesthesia for Craniotomies
Techniques used to allow for safe opening of the dura and access to the tumor, aka:
Brain Relaxation Techniques