Mod X: Anesthesia for CAROTID ARTERY DISEASE Flashcards
Anesthesia for CAROTID ARTERY DISEASE
OBJECTIVES
- State the indications for carotid endarterectomy
- State several frequent co-existing diseases in patients with carotid artery disease
- Describe the anesthetic management of patients undergoing carotid endarterectomy
- Discus intraoperative maneuvers that are utilized to preserve cerebral blood flow
BACKGROUND CVA AND CAROTID ARTERY DISEASE
What’sthe 4th leading cause of death in the U.S. and the leading cause of long-term disability?
Stroke
Stroke is the 4th leading cause of death in the U.S.
Leading cause of long-term disability
Also a Major contributor to increased health care costs
(estimated at $65.8 billion in 2008)
With aging population, an increasing amount of patients will present to the OR with cerebral vascular disease
BACKGROUND CVA AND CAROTID ARTERY DISEASE
There is a strong correlation between strokes and
Carotid artery disease
BACKGROUND CVA AND CAROTID ARTERY DISEASE
CVA may occur from
Embolization of a thrombus or
Plaque debris that cause a reduction in flow
BACKGROUND CVA AND CAROTID ARTERY DISEASE
Regardless of the cause of injury the degree of cerebral injury depends on:
Plaque morphology
Characteristics of the embolus
Duration of hypoperfusion
Integrity of the circle of Willis
Degree cerebral collateral circulation present
CEREBRAL BLOOD FLOW (CBF)
Brain is 2% of body weight, but receives what % of CO?
12-15% of cardiac output

CEREBRAL BLOOD FLOW (CBF)
Total CBF averages
50 ml/100g/min
(750 ml/min)

CEREBRAL BLOOD FLOW (CBF)
Which CBF levels constitute adequate blood flow?
CBF levels >50 ml/100g/min
CEREBRAL BLOOD FLOW (CBF)
Which CBF levels are inadequate? are these a/w permanent injury?
20-50 ml/100g/min CBF is inadequate, but
No permanent injury occurs if blood flow restored
CEREBRAL BLOOD FLOW (CBF)
Which CBF levels may lead to permanent injury?
CBF <20 ml/100g/min => injury will occur
CBF AUTOREGULATION
The phenomenom whereby cerebral blood flow adapts appropriately to changes in mean arterial pressure (MAP) is known as:
Autoregulation
Cerebral blood vessels will constrict when MAP increases and dilate when MAP decreases

CBF AUTOREGULATION
What’s the purpose of Autoregulation?
Serves to maintain a constant CBF despite swings in MAP

CBF AUTOREGULATION
CBF is autoregulated in humans between which MAP values?
60-160 mmHg

CBF AUTOREGULATION
What is CBF regulated by for MAP values >60 or >160?
CBP will be passively regulated by MAP

AUTOREGULATION CURVE
With chronic hypertension the Autoregulation curve shifts to:
The Right
Autoregulation curve shifts to the right with chronic hypertension
This causes the lower and higher ends of the autoregulation range to be higher than in a normotensive pt
This could potentially protect the brain from transient high MAPs
But it occurs at the expense of raising lower limits, which causes an increase risk of ischemia at lower MAPs that would be otherwise tolerated well in a normotensive pt
This is why Hypertensive patients may develop cerebral ischemia at MAPs easily tolerated by normotensive patients

AUTOREGULATION CURVE
With chronic hypotension the Autoregulation curve shifts to:
The Left

CBF AND CHEMICAL CONTROL
What type of relationship exist between CBF and PaCO2 between arterial CO2 25-75 mmHg?
Linear relationship
Linear relationship between CBF and PaCO2 between arterial CO2 25-75 mmHg

CBF AND CHEMICAL CONTROL
How does CO2 causes cerebral vasodilation?
B/c CO2 diffuses freely into the CNS, causing increased concentration of H+ and dilation of the cerebral vessels
This is how Hypoventilation => cerebral vasodilation and inc CBF
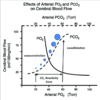
CBF AND CHEMICAL CONTROL
Oxygen tension has an inverse relation with CBF?
Hyperventilation => cerebral vasoconstriction and dec CBF
However, Low arterial oxygen tension increases CBF
When PaO2 fall bellow 50mmHg, there is a rapid inc in CBF

CAROTID ARTERY ENDARTERECTOMY
Most common peripheral vascular surgical procedure
CAROTID ARTERY ENDARTERECTOMY
Estimated 130K procedures performed annually

CAROTID ARTERY ENDARTERECTOMY
Stenosis most commonly at
the bifurcation of the common carotid artery

CAROTID ARTERY ENDARTERECTOMY
Endarterectomy used to reduce symptoms and prevent stroke for over 50 years - why?
Low risk procedure with excellent long-term durability
Many trials have been completed in an effort to recommend the best treatment for pts w/ carotid artery dz, which over the years has actually cause an increase in the number of carotid endarterectomy performed
While carotid surgery has demonstrated postive effects, the terminative benefit must be determined for each pt in order to keep peri-operative strokes and death rates low
Perioperative stroke and death rates must stay low in order to maintain the beneficial effects of surgery over medical therapy

AHA GUIDELINES FOR CAROTID ENDARTERECTOMY
Based on AHA practice recommendations regarding carotid endarterectomies, which Factors are r/t increased risk of stroke?
Age, HTN, ischemic heart disease, diabetes, hyperlipidemia, diabetes, cigarette smoking, & high HCT.
HTN and smoking = two most powerful and treatable risk factors for stroke
AHA GUIDELINES FOR CAROTID ENDARTERECTOMY
Based on AHA practice Recommendations for symptomatic and asymptomatic patients regarding carotid endarterectomies, CAE recommended for symptomatic patients with Carotid Artery Dz of what % stenosis?
>70% stenois
Must also consider operative stroke and death rate along with life expectancy








