Mod VI: Congenital Abnormalities Associated with Respiratory Disorders Flashcards
Congenital Abnormalities Associated with Respiratory Disorders
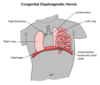
Malformation of the diaphragm allowing herniation of abdominal contents into the thoracic cavity
Congenital Diaphragmatic Hernia
Results in Prevention of prenatal lung development/lung hypoplasia
Congenital Diaphragmatic Hernia
Congenital Diaphragmatic Hernia may result in Prevention of prenatal lung development/lung hypoplasia. What’s a consequence of this?
Hypoxemia → persistent pulmonary HTN
→ ↑ RV pressures → R-to-L shunting thru PDA/PFO
Congenital Diaphragmatic Hernia
What’s the Mortality rate in Congenital Diaphragmatic Hernia?
High mortality rate: 50% not surviving

Congenital Diaphragmatic Hernia
Incidence of Congenital Diaphragmatic Hernia:
1:4,000 live births

Congenital Diaphragmatic Hernia
Which side of the diaghragm is mostly affected by Congenital Diaphragmatic Hernia? Why?
Left side
90% occur on left side
Left side Foramen of Bochdalek closes later than right

Congenital Diaphragmatic Hernia
T/F: Congenital Diaphragmatic Hernia Often detected during prenatal ultrasound
True

Congenital Diaphragmatic Hernia
Clinical features of Congenital Diaphragmatic Hernia
Scaphoid abdomen
Breath sounds absent on involved side
Lung hypoplasia = respiratory distress syndrome

Congenital Diaphragmatic Hernia
Treatment: Respiratory and CV support
Intubated immediately in delivery room
to ↓ air entry into stomach/intestine
Intubating while spontaneous breathing = minimizes air insufflation
If neonate apneic = minimize airway pressures during ventilation with bag and mask to reduce gastric distention
Insert NGT immediately to decompress gut
Congenital Diaphragmatic Hernia
Medical management: PAST vs CURRENT
PAST: Surgical emergency
CURRENT: Delayed closure
Stabilized first with medical & ventilatory treatment
(ECMO, HFV with NO, permissive hypercapnia )
Congenital Diaphragmatic Hernia
Anesthetic Considerations w/ Congenital Diaphragmatic Hernia
AFOI
if not already intubated (post GI decompression) followed by smooth induction
Avoid PPV
(prevents further bowel distention)
Maintain low inspiratory pressures (< 25 cm H2O)
with high ventilatory rates (prevent pneumothorax)
Avoid increases in PVR
(acidosis/hypoxemia/PEEP)
Insert contralateral chest tube
(if Pneumothorax suspected)
Avoid N20
“Gentle Ventilation” with permissive hypercapnia strategies
Inhaled NO
Monitor SaO2
RUE (preductal) - LLE (postductal)
Aid in detection of R-to-L shunting due to persistent PHTN
Place A-line
for frequent assessment of acid-base balance and oxygenation/ventilation
Acidotic?: Hyperventilate/NaHCO3
Maintain body temperature
Selection of technique dependent of stability and hemodynamics of the neonate
Congenital Diaphragmatic Hernia
“Gentle Ventilation” with permissive hypercapnia strategies aim to:
Limit peak inspiratory pressure and minimize barotrauma
Postductal PaCO2 55-60 mmHg - Goal pH >7.35
Preductal SaO2 > 85%
Limit PIP to < 25
Congenital Diaphragmatic Hernia
Benefits of inhaled NO include:
Improve oxygenation
Decrease intrapulmonary shunting
Congenital Diaphragmatic Hernia
SaO2 measured fro the RUE is categorized as:
Preductal

Congenital Diaphragmatic Hernia
SaO2 measured fro the LLE is categorized as:
Postductal

Congenital Diaphragmatic Hernia
Monitor pre and post-ductal SaO2 Aid in detection of:
R-to-L shunting due to persistent PHTN
Congenital Abnormalities Associated with Respiratory Disorders
The obstruction of airway passages between nasal cavity and nasopharynx, where all breathing becomes oral, and could lead to ASPHYIXIATION is also known as:
Choanal Atresia

Choanal Atresia
Incidence of Choanal Atresia:
1 : 8,000 live births

Choanal Atresia Co-existing anomalies
Think: “CHARGE”
C: Coloboma (eye defect)
H: Heart (TOF, PDA, DORV, VSD, A-V canal)
A: Atresia of choanae
R: Retarded growth (other CNS anomalies)
G: Genital (hypogonadism)
E: Ear anomalies

Choanal Atresia
Choanal Atresia is a PEDIATRIC EMERGENCY. How is it managed?
Present with oral airway or OET since birth: maintain airway
Oral RAE: avoid interfering with surgery

Meconium Aspiration Syndrome
Meconium staining occurs in what percentage of births?
10% of births
Associated with asphyxia/fetal death

Meconium Aspiration Syndrome
Etiology of Meconium Aspiration Syndrome
Chronic fetal hypoxia during 3rd trimester
Passage of meconium into amniotic fluid
Swallowed by fetus into trachea/lungs prior to or during birth
Thick, tenacious
Obstructs tracheobronchial tree

Meconium Aspiration Syndrome
Pathogenesis of Meconium Aspiration Syndrome
Complete obstruction: distal atelectasis
Partial obstruction: overinflation of distal airspaces = pneumothorax
Bile = chemical pneumonitis
Meconium inhibits surfactant
Hypoxemia → PPHTN
Meconium Aspiration Syndrome
Management of Meconium Aspiration Syndrome
Decrease effects of aspiration
Routine oropharyngeal suctioning immediately at time of delivery
Apgar 7-9:
requires no additional airway management
Apgar < 7:
Tracheal suction prior to 1st breath
Intubate and suction prior to instituting PPV
Mechanically ventilate
Long expiratory times to decrease air trapping if partial obstruction
HF oscillatory ventilation to recruit closed segments if complete
Induce alkalosis
Inhaled NO
Exogenous surfactant
Bronchopulmonary Dysplasia (Chronic Lung Disease)
T/F: Bronchopulmonary Dysplasia (Chronic Lung Disease) Develops following respiratory distress syndrome and resultant lung injury
True
Bronchopulmonary Dysplasia (Chronic Lung Disease)
Principle Risk factors for Bronchopulmonary Dysplasia (Chronic Lung Disease) are:
Low birth weight (1500 g)
Gestational age (more immature)
Bronchopulmonary Dysplasia (Chronic Lung Disease)
Consequential Risk factors for Bronchopulmonary Dysplasia (Chronic Lung Disease) are:
O2 toxicity (High FiO2 for > 28 days)
Development of pneumothorax or interstitial emphysema
Iatrogenic fluid overload
Mechanical injury (MV for first 3 days or more of life)
Presence of PDA
Bronchopulmonary Dysplasia (Chronic Lung Disease)
Other additional causes of Bronchopulmonary Dysplasia (Chronic Lung Disease) are:
Pneumonia
Sepsis
Persistent pulmonary HTN
Pulmonary hypoplasia
Apnea of prematurity
Bronchopulmonary Dysplasia (Chronic Lung Disease)
What the Pathophysiology of Bronchopulmonary Dysplasia (Chronic Lung Disease)?
Pulmonary immaturity + Surfactant-deficit alveoli
=> Respiratory distress syndrome
Bronchopulmonary Dysplasia (Chronic Lung Disease)
How does maintaining oxygenation/ventilation in the Treatment of Bronchopulmonary Dysplasia (Chronic Lung Disease) produces pulmonary injury?
High FiO2 and continued supplemental O2→O2 free radicals→ Oxygen toxicity = airway inflammation
PPV of surfactant deficit alveoli→ overdistention (barotrauma) and transudation of fluid into alveoli (hyaline membrane disease)
Bronchoconstriction develops in 80%
Bronchopulmonary Dysplasia (Chronic Lung Disease)
Clinical presentation of Bronchopulmonary Dysplasia (Chronic Lung Disease):
Tachypnea with retractions
Rales/wheezing
Increased PVR→ ↑PAP→ RV hypertrophy = Cor pulmonale
Persistent requirement for supplemental O2
Hypercarbia
“BPD” spells
(Sudden severe bronchospasm with cyanosis with physical agitation or stimulation)
Bronchopulmonary Dysplasia (Chronic Lung Disease)
Anesthetic considerations w/ Bronchopulmonary Dysplasia (Chronic Lung Disease)
Pulmonary function should be optimized if possible
Prevalence of bronchospasm and airway reactivity should be considered when planning anesthetic
LMA preferred to ET - Deep extubation - Regional
Hand ventilation
Allows determination of pulmonary compliance
Decreases risk of pneumothorax
Avoid events that aggravate pulmonary HTN
Acidosis - Hypoxia - Hypercarbia - Hypothermia

Persistent Pulmonary Hypertension
Pathogenesis of Persistent Pulmonary Hypertension:
Increased PVR→ Pulmonary HTN
→ R-L shunting across patent foramen ovale→ cyanosis

Persistent Pulmonary Hypertension
Etiology of Persistent Pulmonary Hypertension
Hypoxemia
Acidosis
Respiratory distress syndrome
Meconium aspiration

Persistent Pulmonary Hypertension
Treatment of Persistent Pulmonary Hypertension
Tx is aimed at Decreases PVR, Decreased R-L shunting
Intubation with mechanical ventilation
Induce respiratory/metabolic alkalosis
(Will decrease PVR)
Support BP (fluids/pressors)
Inhaled NO
Decreases PVR, R-L shunting, increases systemic oxygenation
ECMO*

Persistent Pulmonary Hypertension
When is ECMO* indicated in the treatment of Persistent Pulmonary Hypertension?

Reserved for severe hypoxemia
Requires heparinization and platelet infusion during use
Mortality due to intraventricular hemorrhage
http://circ.ahajournals.org/content/109/25/3106.full

Persistent Pulmonary Hypertension
In the treatment of Persistent Pulmonary Hypertension, what are contraindications to using ECMO*?

Intraventricular hemorrhage
Severe neurological impairment
Cyanotic CHD
http://circ.ahajournals.org/content/109/25/3106.full



